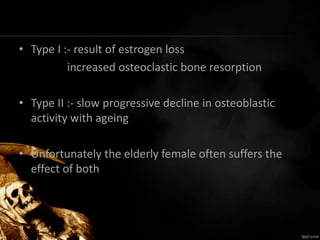
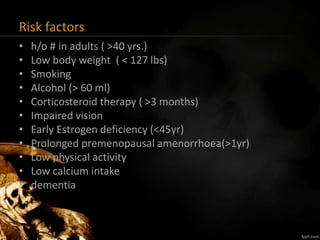
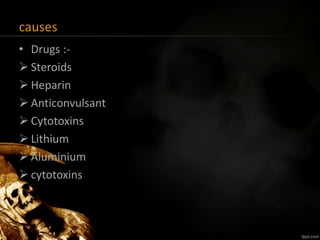
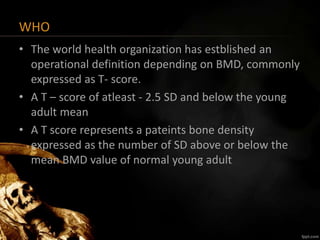
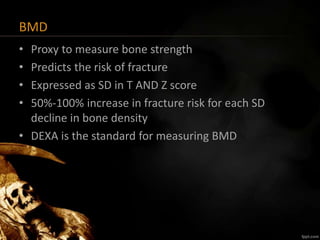
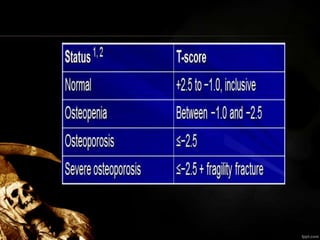
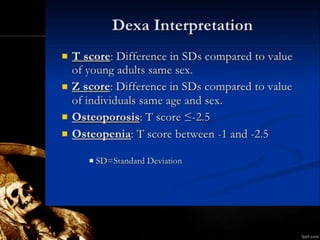
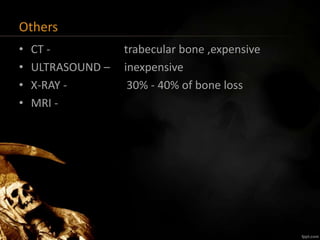
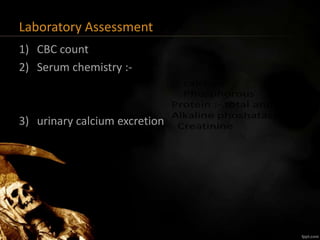
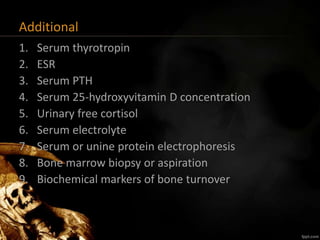
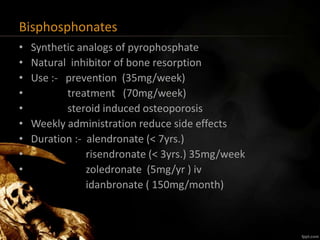
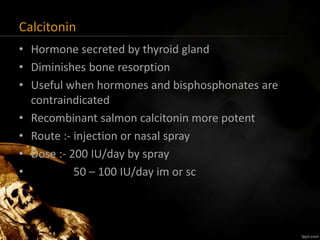
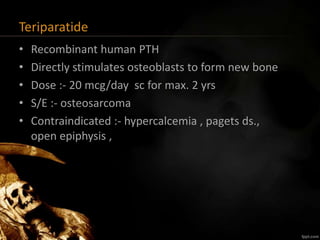
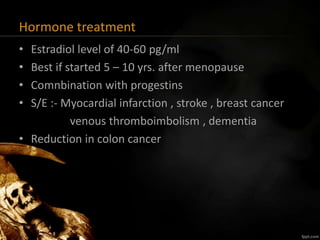
Osteoporosis is a systemic bone disease characterized by low bone mass and deterioration of bone tissue, leading to increased bone fragility and risk of fractures. It is most common in postmenopausal women. Risk factors include smoking, low body weight, steroid use, excess alcohol intake, and family history of fractures. Diagnosis involves measuring bone mineral density via DEXA scan. Treatment aims to prevent fractures and bone loss, and includes adequate calcium and vitamin D, weight-bearing exercise, falls prevention, pharmacologic agents like bisphosphonates, and surgery for fractures. Regular screening and monitoring of at-risk individuals is important.