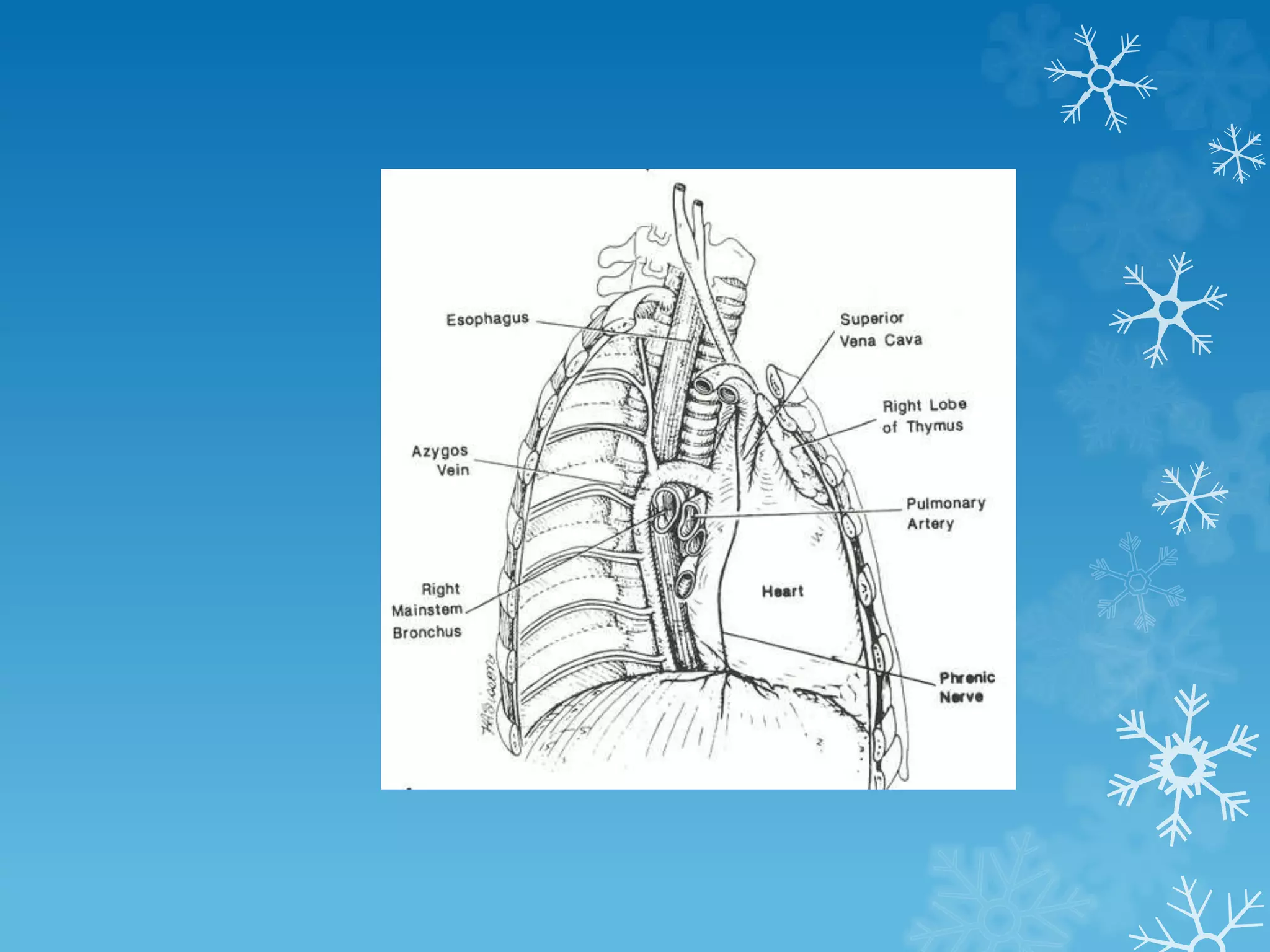
This document discusses lung and mediastinal tumours. It covers the epidemiology, etiological factors like smoking, histological classifications, clinical presentation, investigations including imaging and biopsies, staging, treatments such as surgery, chemotherapy and radiation, and complications. It also discusses tumours that can occur in the different mediastinal compartments and associated conditions.