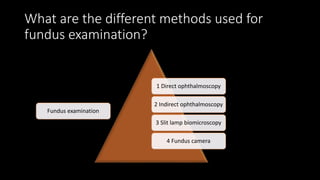
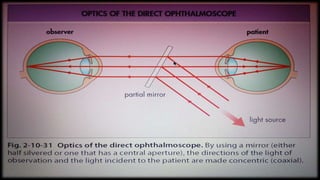
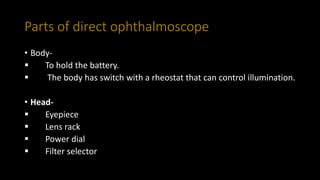
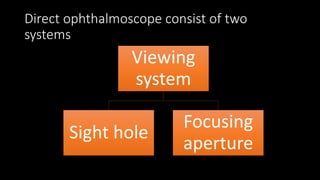
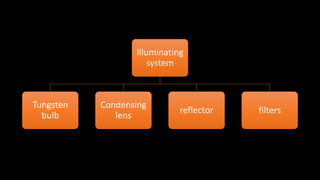
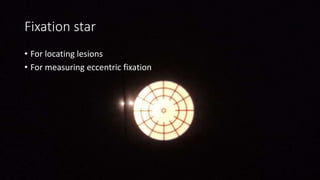
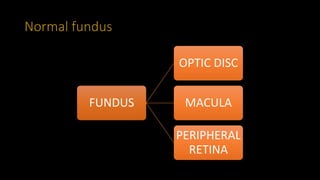
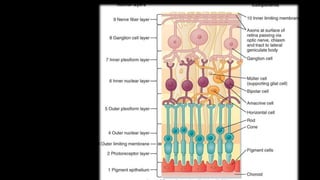
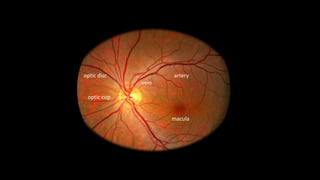
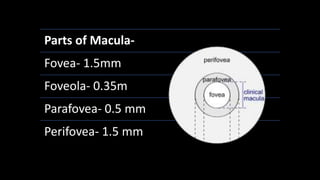
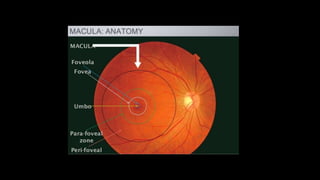
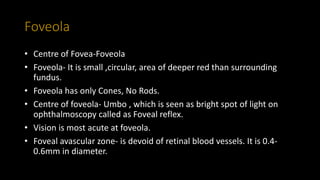
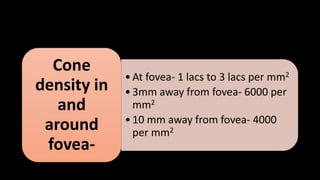
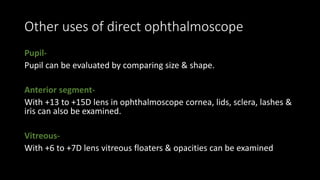
The document is a comprehensive guide on direct ophthalmoscopy, detailing its history, procedure, optical principles, and the parts of a direct ophthalmoscope. It discusses various aspects of fundus examination, common uses, and the conditions that can be diagnosed using this method. Additionally, it outlines the advantages and disadvantages of direct ophthalmoscopy and the anatomy of the retina and fundus.