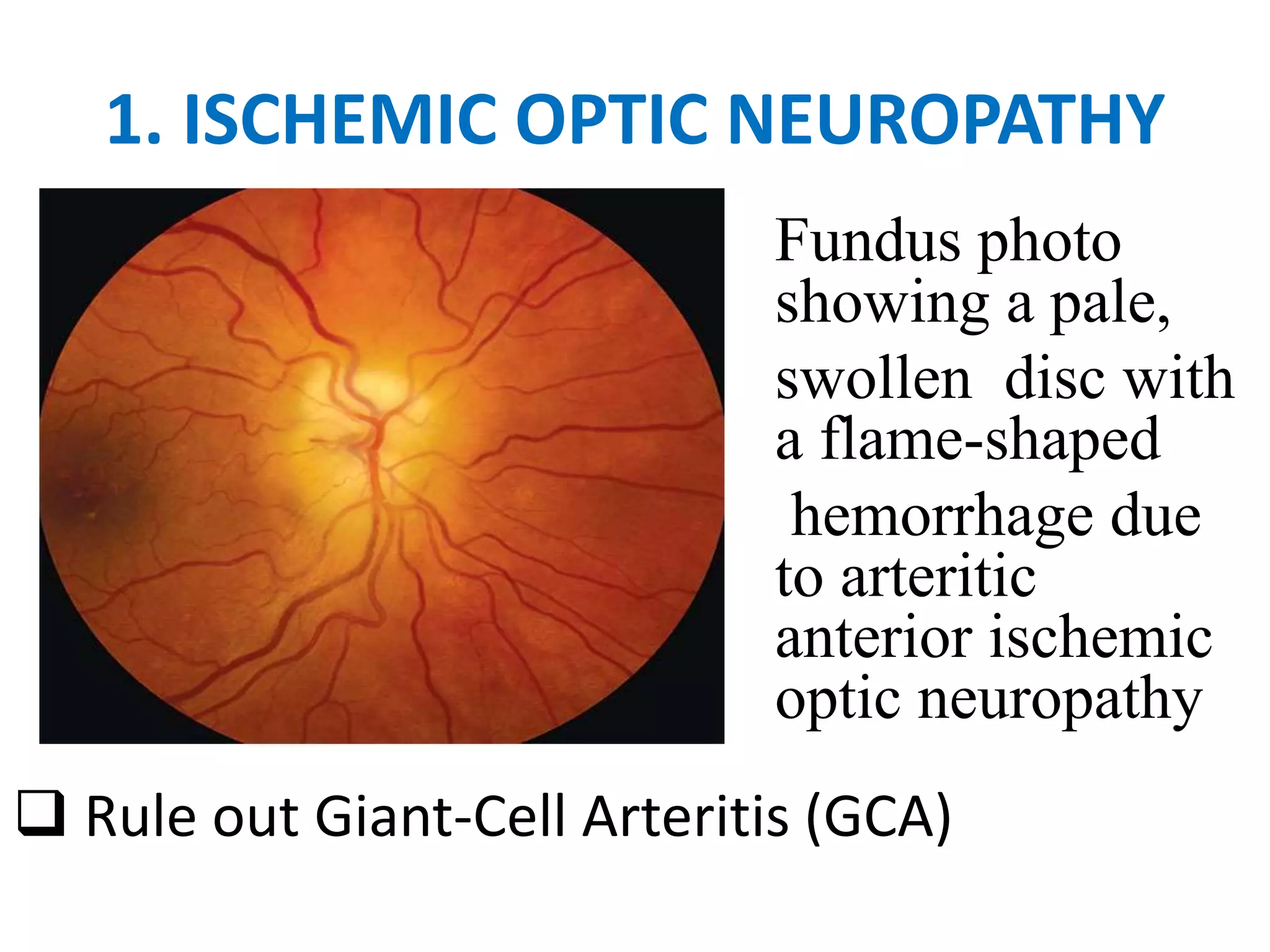
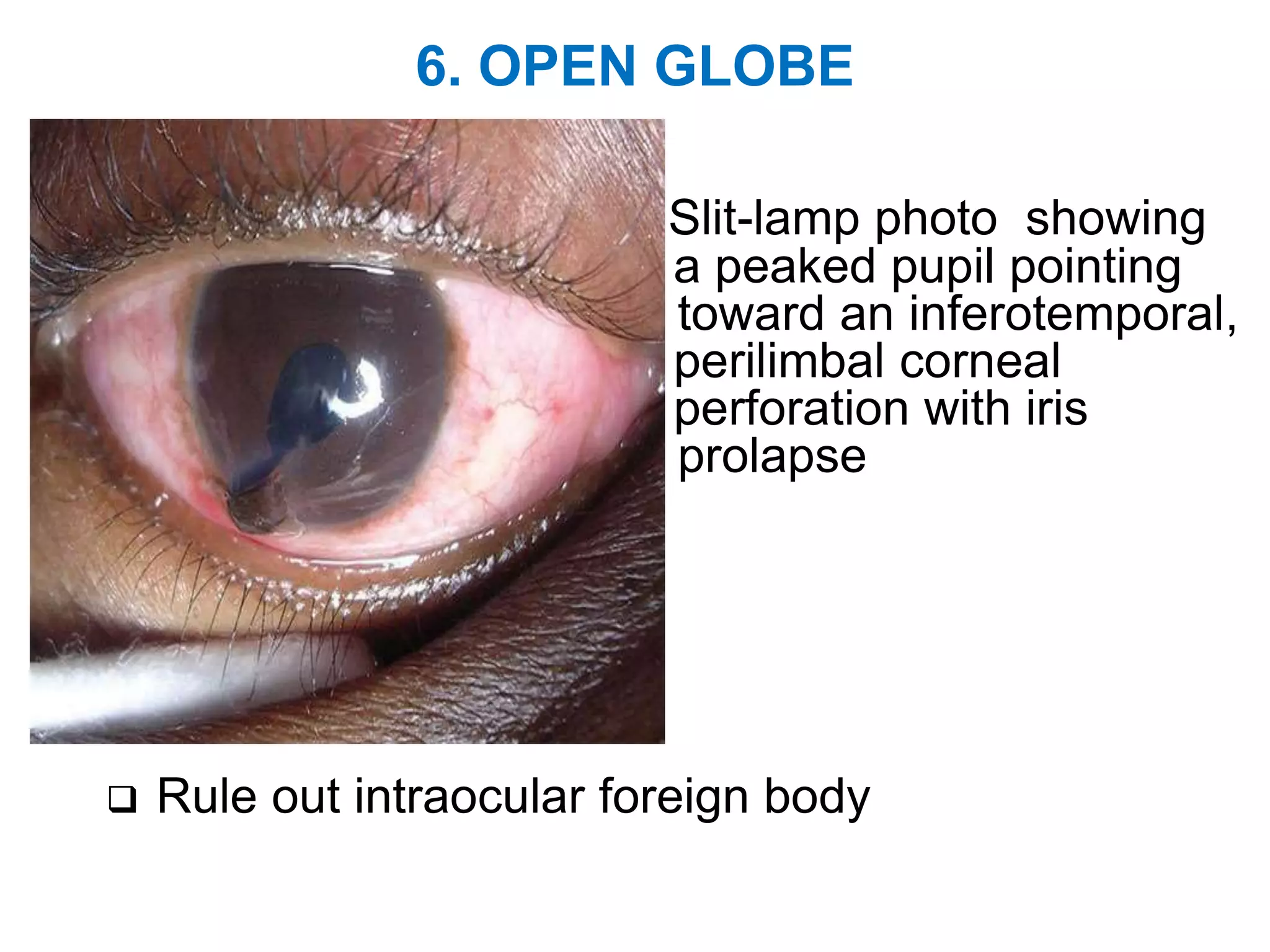
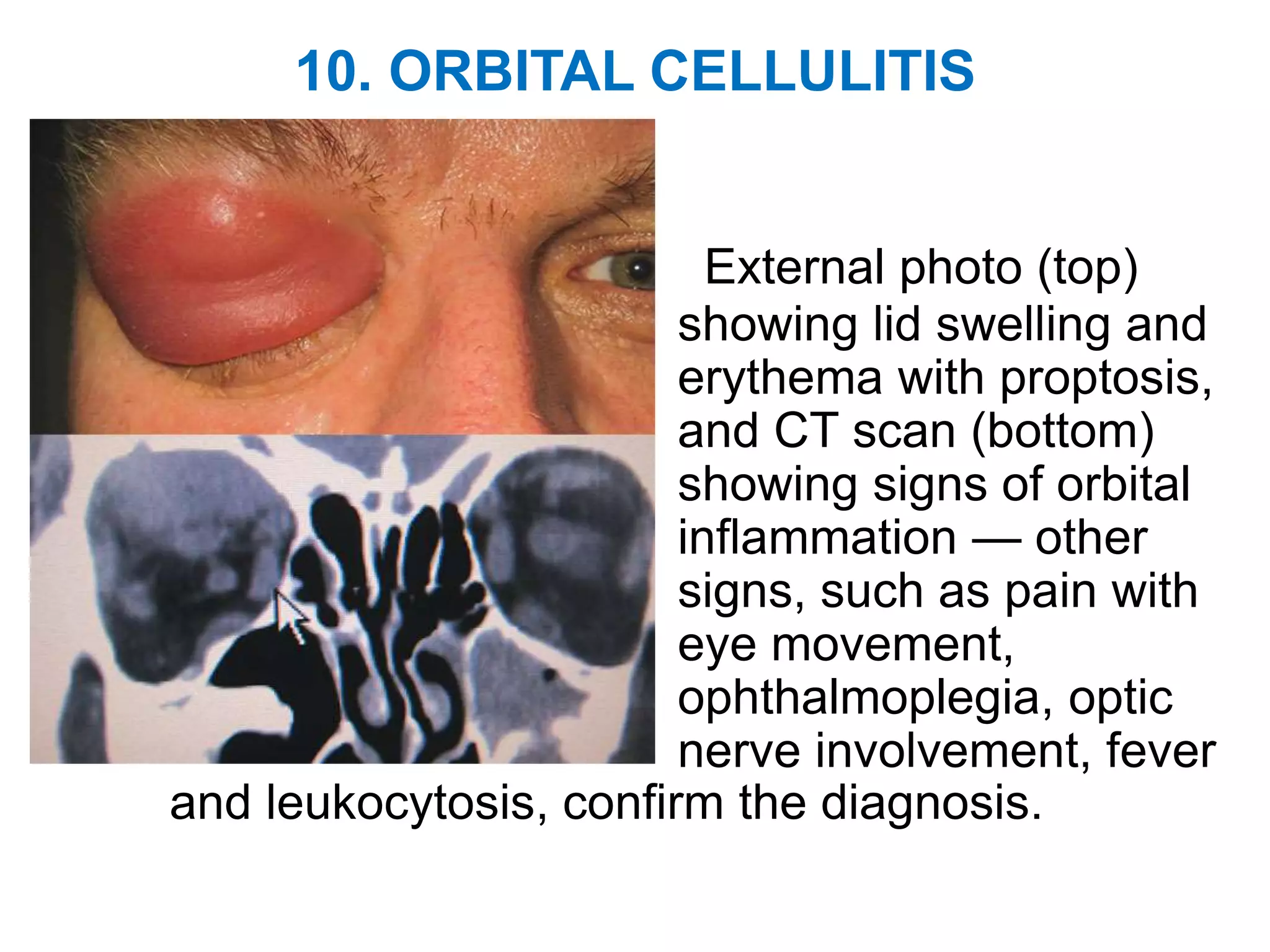
This document provides information about ocular emergencies for student nurses, including objectives, classifications of emergencies, top ten emergencies, symptoms, and management of issues like chemical injuries, foreign bodies, and trauma. It aims to help students recognize, assess, diagnose, and properly treat ocular emergencies to prevent vision loss. The top ten emergencies covered include ischemic optic neuropathy, central retinal artery occlusion, retinal detachment, nerve palsy, corneal infections, open globe injuries, glaucoma, endophthalmitis, alkali injuries, and orbital cellulitis.