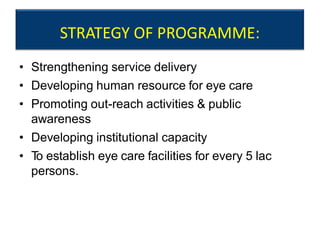
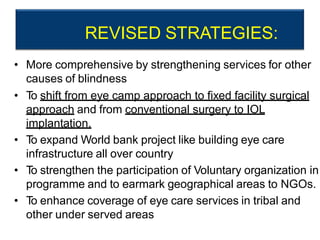
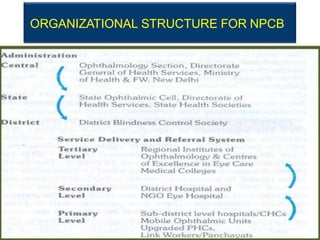
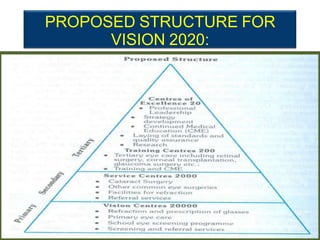
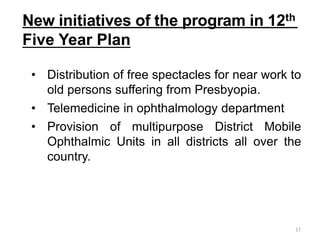
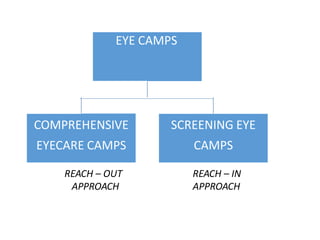
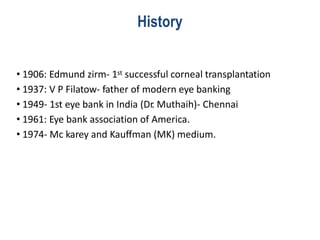
The document discusses India's National Programme for Control of Blindness (NPCB). It was launched in 1976 with the goal of reducing blindness prevalence from 1.4% to 0.3% by 2020. The NPCB focuses on activities like cataract surgeries, eye camps, school eye screening, and eye banking. It has a decentralized structure with District Blindness Control Societies. The NPCB aims to strengthen eye care infrastructure, human resources, and increase public awareness. It coordinates with NGOs and private practitioners to provide comprehensive eye care services across India.