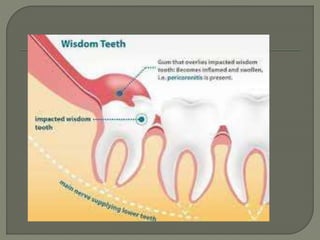
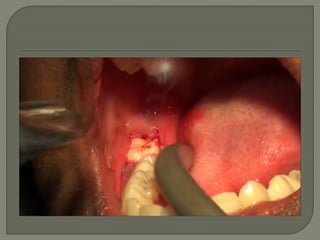
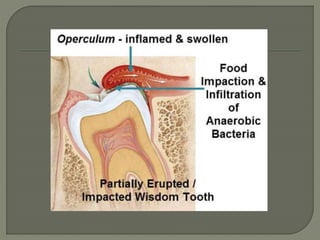
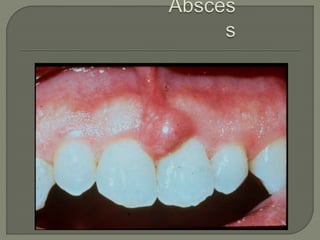
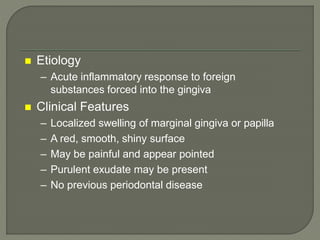
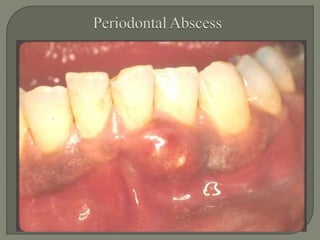
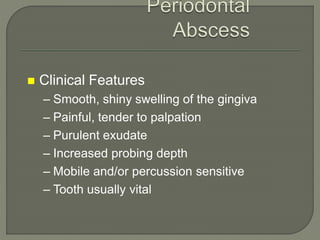
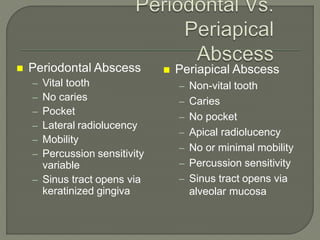
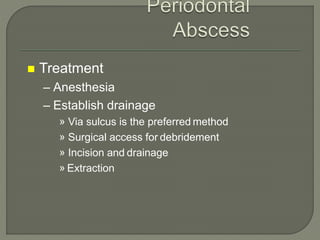
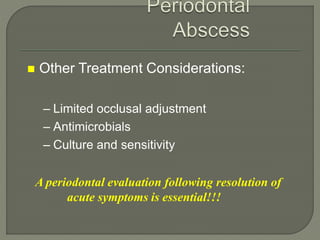
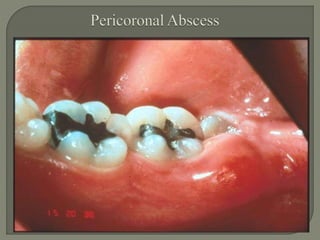
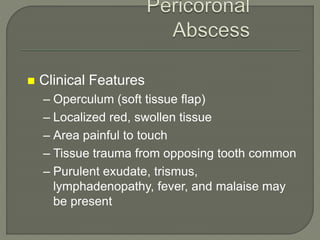
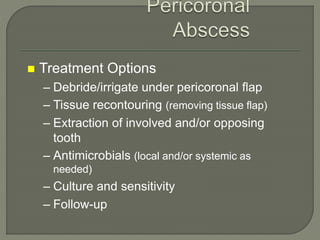
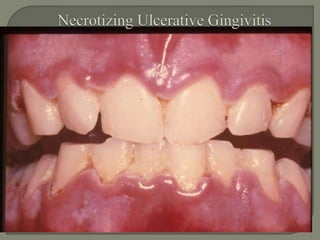
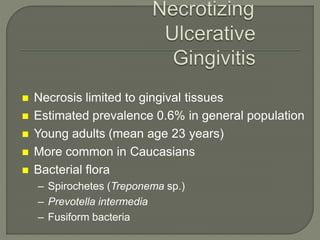
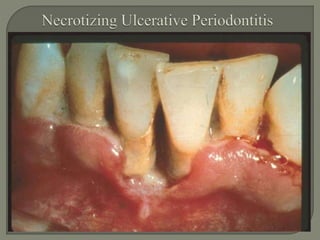
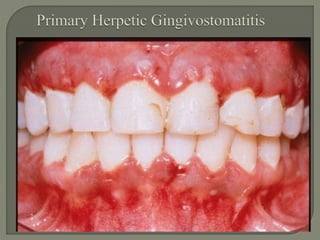
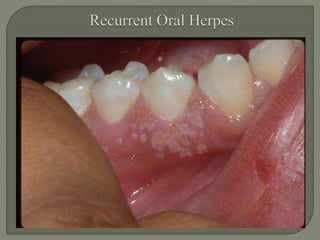
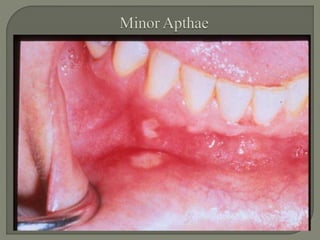
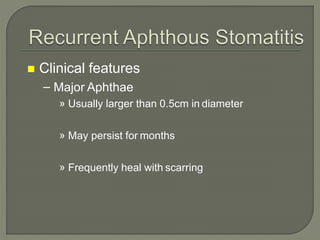
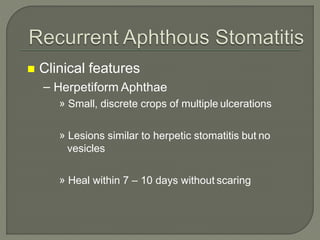
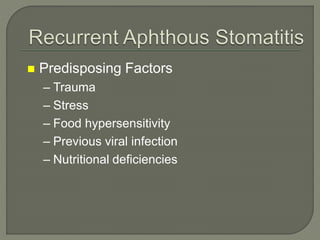
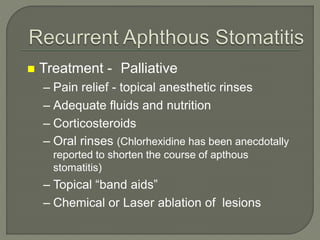
This document discusses several acute periodontal conditions: abscesses of the periodontium including gingival, periodontal, and pericoronal abscesses; necrotizing periodontal diseases including necrotizing ulcerative gingivitis and necrotizing ulcerative periodontitis; gingival diseases of viral origin such as herpesvirus; and recurrent aphthous stomatitis. It provides details on the etiology, clinical features, and treatment of each condition.