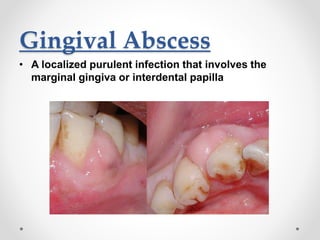
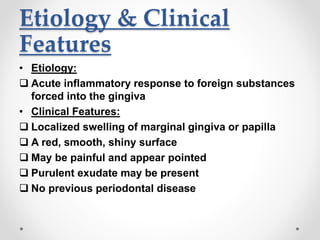
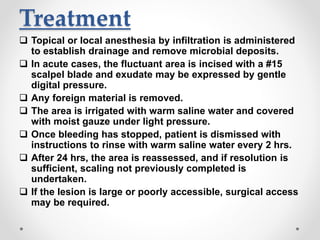
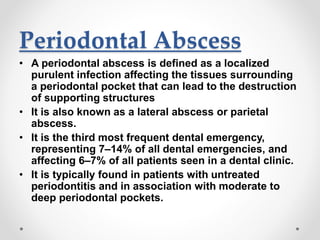
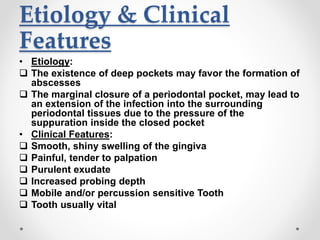
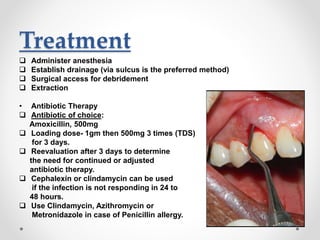
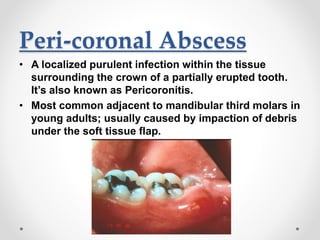
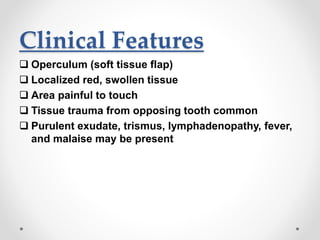
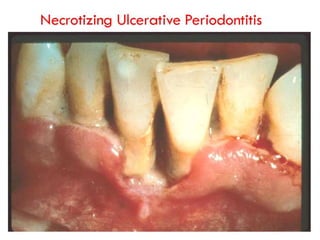
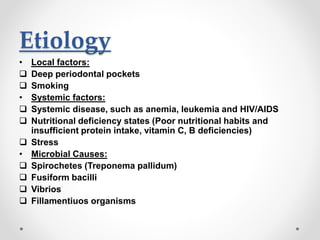
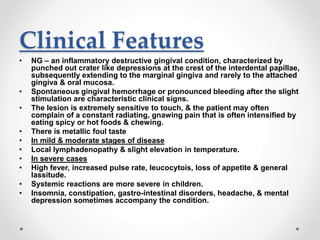
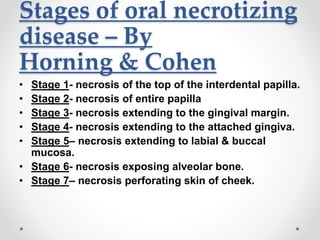
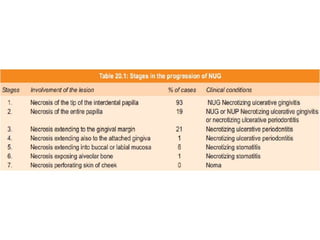
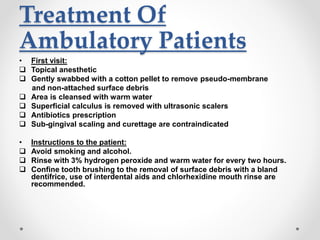
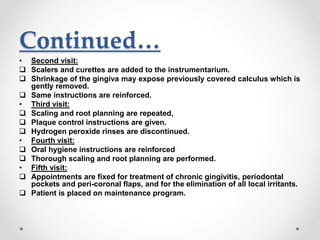
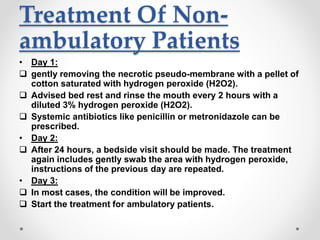
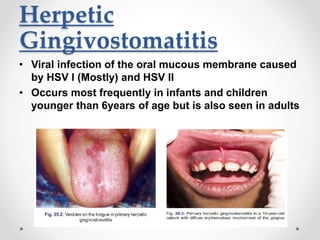
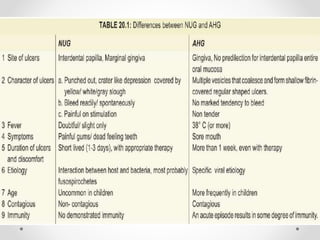
This document discusses several acute gingival infections: abscesses, necrotizing ulcerative gingivitis (NUG), and herpetic gingivostomatitis. It describes the etiology, clinical features, and treatment for each condition. Abscesses are classified as gingival, periodontal, or peri-coronal and can be treated with drainage, irrigation, and antibiotics if needed. NUG is a disease caused by bacteria that causes gingival necrosis and pain. Its stages and treatment focus on removal of debris and dead tissue. Herpetic gingivostomatitis is a viral infection seen in children that causes vesicles and ulcers in the mouth.