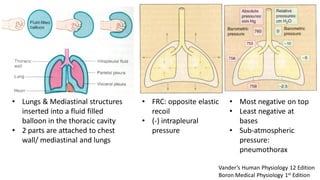
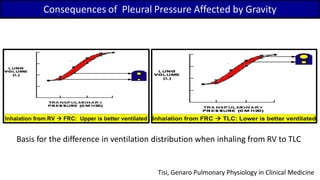
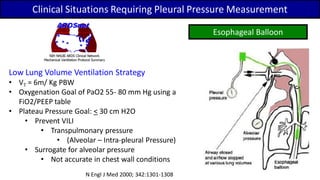
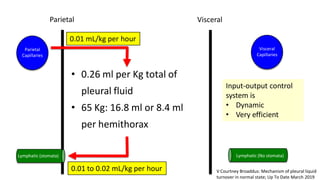
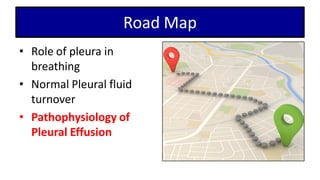
The document discusses pleural physiology, emphasizing the role of the pleura in breathing, pleural fluid turnover, and the pathophysiology of pleural effusions. It explains the mechanics of pleural pressure, factors affecting fluid turnover, and the causes of fluid accumulation in diseases. The key takeaway is that pleural effusion results from an imbalance in fluid formation and drainage, influenced by various physiological and pathological factors.




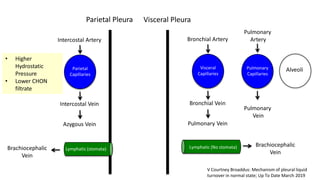
![Parietal
Capillaries
Lymphatic (stomata)
Parietal
Visceral
Capillaries
Visceral
Lymphatic (No stomata)
Pulmonary
Capillaries
Alveoli
Interstitial
Compartment
Interstitial
Compartment
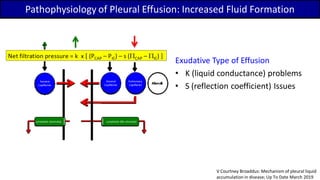
Net filtration pressure = k x [ (PCAP – PIC) – s (PCAP – PIC) ]
• K: Liquid conductance
• PCAP: capillary hydrostatic pressure
• PIC: Interstitial Compartment hydrostatic pressure
• S: reflection coefficient
• 0: Completely permeable to protein
• 1: Non- permeable to protein
• PCAP: capillary oncotic pressure
• PIC: Interstitial Compartment oncotic pressure(+) : favors fluid moving out of the capillaries
V Courtney Broaddus: Mechanism of pleural liquid
turnover in normal state; Up To Date March 2019](https://image.slidesharecdn.com/01pleuralphysiologyreferenced-190410115331/85/01-pleural-physiology-referenced-13-320.jpg)
![Parietal Visceral
K (Liquid conductance) Same
PCAP Higher Lower
PIC Same
S (Reflection Coefficient) Same
PCAP Same
PIC Same
Net filtration pressure
(cm H2O)
14 9
Net filtration pressure = k x [ (PCAP – PIC) – s (PCAP – PIC) ]
Parietal
Capillaries
Lymphatic (stomata)
Parietal
Visceral
Capillaries
Visceral
Lymphatic (No stomata)
V Courtney Broaddus: Mechanism of pleural liquid
turnover in normal state; Up To Date March 2019](https://image.slidesharecdn.com/01pleuralphysiologyreferenced-190410115331/85/01-pleural-physiology-referenced-14-320.jpg)


![Parietal
Capillaries
Lymphatic (stomata)
Visceral
Capillaries
Lymphatic (No stomata)
Pulmonary
Capillaries Alveoli
Net filtration pressure = k x [ (PCAP – PIC) – s (PCAP – PIC) ]
Pathophysiology of Pleural Effusion: Increased Fluid Formation](https://image.slidesharecdn.com/01pleuralphysiologyreferenced-190410115331/85/01-pleural-physiology-referenced-19-320.jpg)
![Pathophysiology of Pleural Effusion: Increased Fluid Formation
Parietal
Capillaries
Lymphatic (stomata)
Visceral
Capillaries
Lymphatic (No stomata)
Pulmonary
Capillaries Alveoli
Net filtration pressure = k x [ (PCAP – PIC) – s (PCAP – PIC) ] Increased Liquid Conductance
• Induced substances released during
• Malignancy
• Infection
• Inflammation
• Fluid: Exudative Type (usually
concomitant with decreased in
reflection coefficient)
V Courtney Broaddus: Mechanism of pleural liquid
accumulation in disease; Up To Date March 2019
Net filtration pressure = k x [ (PCAP - PIC) – s (πCAP – πIC) ]](https://image.slidesharecdn.com/01pleuralphysiologyreferenced-190410115331/85/01-pleural-physiology-referenced-20-320.jpg)
![Pathophysiology of Pleural Effusion: Increased Fluid Formation
Parietal
Capillaries
Lymphatic (stomata)
Visceral
Capillaries
Lymphatic (No stomata)
Pulmonary
Capillaries Alveoli
Net filtration pressure = k x [ (PCAP – PIC) – s (PCAP – PIC) ]
Increased Capillary Hydrostatic Pressure
• High systemic venous pressure
• High pulmonary venous pressure
• Fluid: Transudative Type
V Courtney Broaddus: Mechanism of pleural liquid
accumulation in disease; Up To Date March 2019
Net filtration pressure = k x [ (PCAP - PIC) – s (πCAP – πIC) ]](https://image.slidesharecdn.com/01pleuralphysiologyreferenced-190410115331/85/01-pleural-physiology-referenced-21-320.jpg)



![Intrinsic Factors: Inhibition of lymphatic smooth
muscle contraction
• Products of inflammation
• Endocrine abnormalities (hypothyroidism)
• Radiation or drugs (chemotherapeutic agents)
• Cancer cell infiltration
Extrinsic Factors: Lymphatics are normal
• Limitation of respiratory movements
(diaphragm paralysis)
• Mechanical compression (pleural fibrosis)
• Blockade of stomata (pleural malignancy)
• Decrease intrapleural pressure (atelectasis)
• Increased systemic venous pressure
Parietal
Capillaries
Lymphatic (stomata)
Visceral
Capillaries
Lymphatic (No stomata)
Pulmonary
Capillaries Alveoli
Net filtration pressure = k x [ (PCAP – PIC) – s (PCAP – PIC) ]
Pathophysiology of Pleural Effusion: Decreased Drainage
V Courtney Broaddus: Mechanism of pleural liquid
accumulation in disease; Up To Date March 2019
Net filtration pressure = k x [ (PCAP - PIC) – s (πCAP – πIC) ]](https://image.slidesharecdn.com/01pleuralphysiologyreferenced-190410115331/85/01-pleural-physiology-referenced-26-320.jpg)
![Intrinsic Factors: Inhibition of lymphatic smooth
muscle contraction
• Products of inflammation
• Endocrine abnormalities (hypothyroidism)
• Radiation or drugs (chemotherapeutic agents)
• Cancer cell infiltration
Extrinsic Factors: Lymphatics are normal
• Limitation of respiratory movements
(diaphragm paralysis)
• Mechanical compression (pleural fibrosis)
• Blockade of stomata (pleural malignancy)
• Decrease intrapleural pressure (atelectasis)
• Increased systemic venous pressure
Parietal
Capillaries
Lymphatic (stomata)
Visceral
Capillaries
Lymphatic (No stomata)
Pulmonary
Capillaries Alveoli
Net filtration pressure = k x [ (PCAP – PIC) – s (PCAP – PIC) ]
Pathophysiology of Pleural Effusion: Malignancy
V Courtney Broaddus: Mechanism of pleural liquid
accumulation in disease; Up To Date March 2019
Net filtration pressure = k x [ (PCAP - PIC) – s (πCAP – πIC) ]](https://image.slidesharecdn.com/01pleuralphysiologyreferenced-190410115331/85/01-pleural-physiology-referenced-27-320.jpg)
![Intrinsic Factors: Inhibition of lymphatic smooth
muscle contraction
• Products of inflammation
• Endocrine abnormalities (hypothyroidism)
• Radiation or drugs (chemotherapeutic agents)
• Cancer cell infiltration
Extrinsic Factors: Lymphatics are normal
• Limitation of respiratory movements
(diaphragm paralysis)
• Mechanical compression (pleural fibrosis)
• Blockade of stomata (pleural malignancy)
• Decrease intrapleural pressure (atelectasis)
• Increased systemic venous pressure
Parietal
Capillaries
Lymphatic (stomata)
Visceral
Capillaries
Lymphatic (No stomata)
Pulmonary
Capillaries Alveoli
Net filtration pressure = k x [ (PCAP – PIC) – s (PCAP – PIC) ]
Pathophysiology of Pleural Effusion: Pulmonary Embolism
Majority of pleural effusion 2nd to
PE are exudative.
V Courtney Broaddus: Mechanism of pleural liquid
accumulation in disease; Up To Date March 2019
Net filtration pressure = k x [ (PCAP - PIC) – s (πCAP – πIC) ]](https://image.slidesharecdn.com/01pleuralphysiologyreferenced-190410115331/85/01-pleural-physiology-referenced-28-320.jpg)
![Intrinsic Factors: Inhibition of lymphatic smooth
muscle contraction
• Products of inflammation
• Endocrine abnormalities (hypothyroidism)
• Radiation or drugs (chemotherapeutic agents)
• Cancer cell infiltration
Extrinsic Factors: Lymphatics are normal
• Limitation of respiratory movements
(diaphragm paralysis)
• Mechanical compression (pleural fibrosis)
• Blockade of stomata (pleural malignancy)
• Decrease intrapleural pressure (atelectasis)
• Increased systemic venous pressure
Parietal
Capillaries
Lymphatic (stomata)
Visceral
Capillaries
Lymphatic (No stomata)
Pulmonary
Capillaries Alveoli
Net filtration pressure = k x [ (PCAP – PIC) – s (PCAP – PIC) ]
Pathophysiology of Pleural Effusion: Left Heart Failure
V Courtney Broaddus: Mechanism of pleural liquid
accumulation in disease; Up To Date March 2019
Net filtration pressure = k x [ (PCAP - PIC) – s (πCAP – πIC) ]](https://image.slidesharecdn.com/01pleuralphysiologyreferenced-190410115331/85/01-pleural-physiology-referenced-29-320.jpg)
![Parietal
Capillaries
Lymphatic (stomata)
Visceral
Capillaries
Lymphatic (No stomata)
Pulmonary
Capillaries Alveoli
Net filtration pressure = k x [ (PCAP – PIC) – s (PCAP – PIC) ]
Pathophysiology of Pleural Effusion: Left Heart Failure
Interlobular peri-bronchovascular sub-pleural interstitium Pleural cavity
V Courtney Broaddus: Mechanism of pleural liquid
accumulation in disease; Up To Date March 2019
Net filtration pressure = k x [ (PCAP - PIC) – s (πCAP – πIC) ]](https://image.slidesharecdn.com/01pleuralphysiologyreferenced-190410115331/85/01-pleural-physiology-referenced-30-320.jpg)