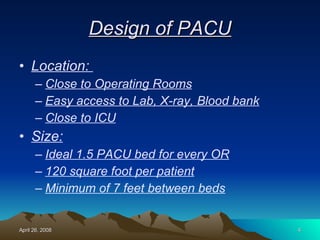
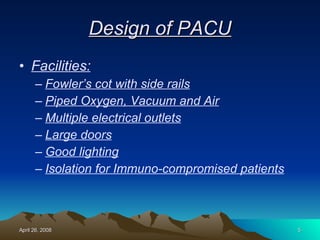
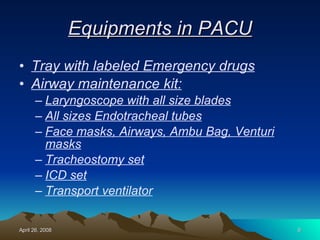
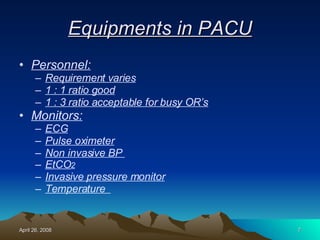
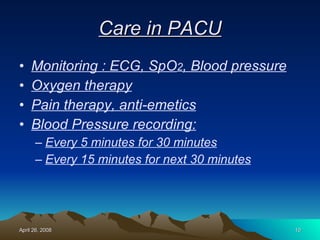
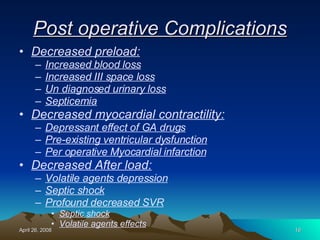
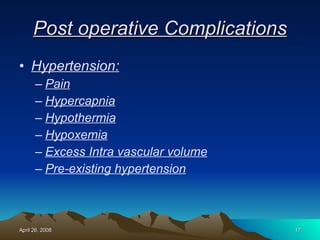
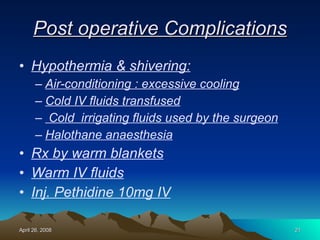
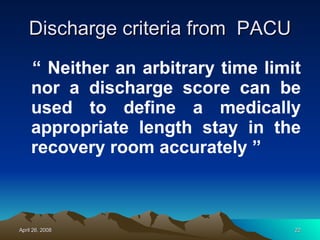
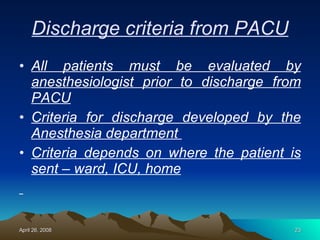
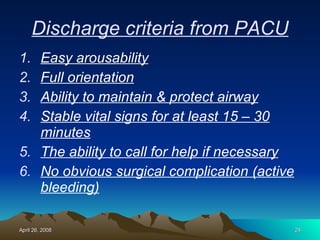
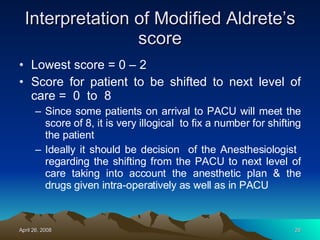
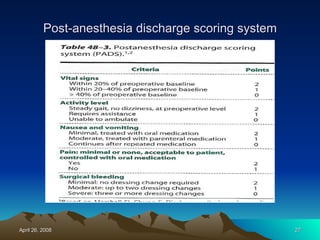
The document discusses the history and importance of post-anesthesia care units (PACUs) and outlines their design, equipment, staffing needs, and standard procedures for patient care and monitoring. Key aspects of PACU care include criteria for patient transfer from the operating room to PACU, routine post-anesthesia monitoring and treatment, potential post-operative complications, discharge criteria, and scoring systems used to evaluate patient recovery status.