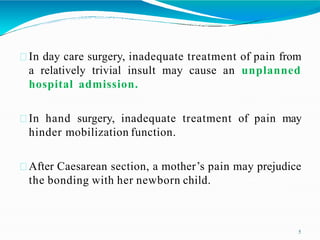
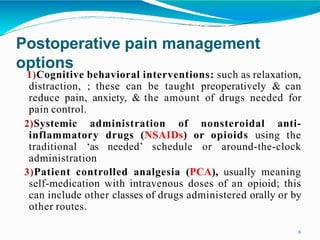
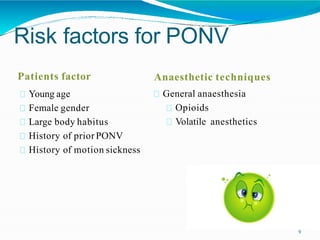
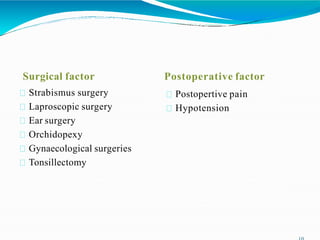
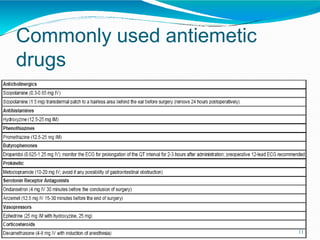
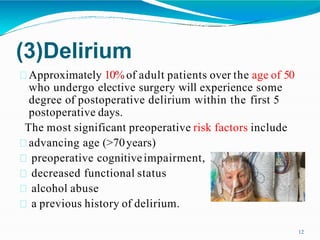
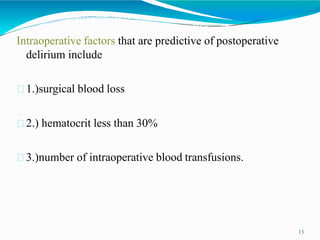
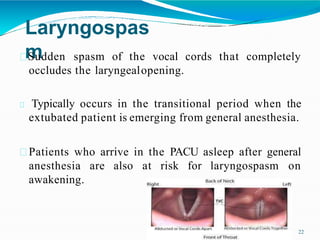
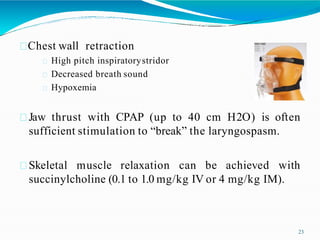
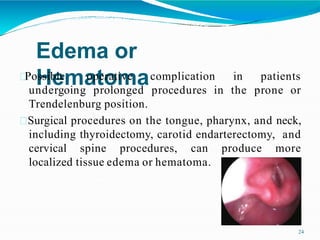
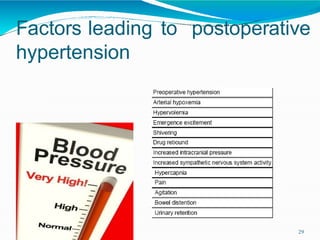
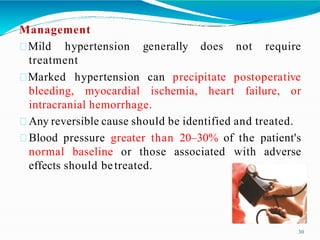
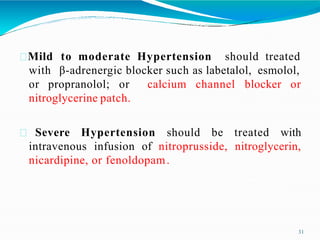
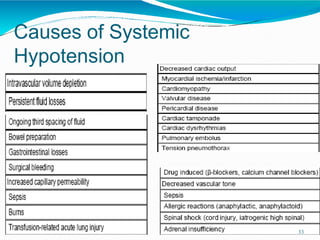
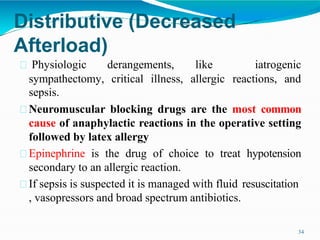
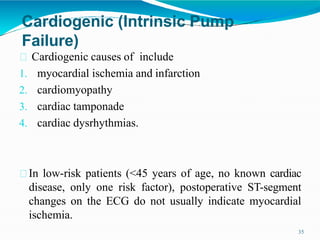
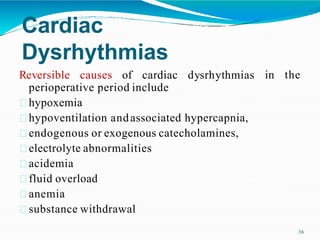
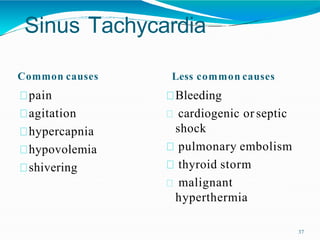
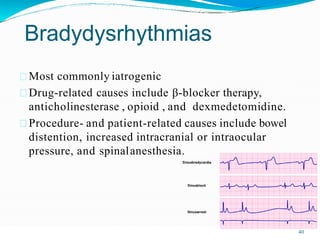
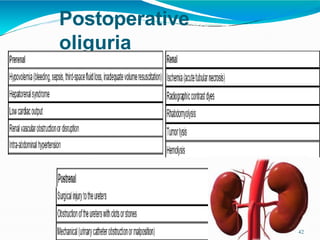
The document discusses post-operative complications, emphasizing the importance of proper management in the post-anesthesia care unit (PACU). Key complications include postoperative pain, nausea and vomiting, delirium, shivering, respiratory complications, hemodynamic instability, and renal dysfunction, each requiring specific management strategies. The role of anesthesiologists is highlighted in overseeing patient safety during the recovery process, ensuring a smoother transition from general anesthesia to recovery.