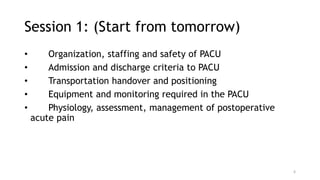
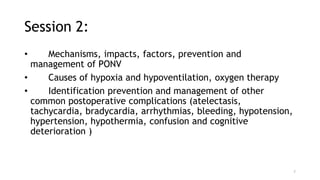
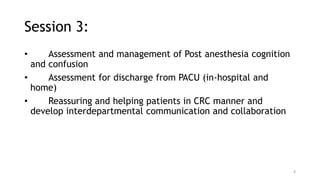
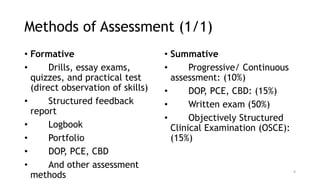
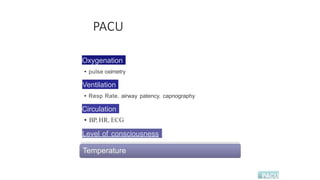
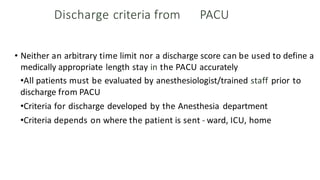
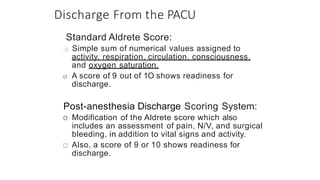
This document outlines the course objectives and content for a Post Anesthesia Care Unit (PACU) training course. The course objectives cover topics such as postoperative patient transportation and handover, PACU equipment, monitoring and roles, postoperative pain management, complications and their treatment. The document details the sessions that will cover these topics over 4 days. It also provides the assessment methods for the course and reference materials. The overall goal of the PACU training course is to educate medical professionals on providing safe and effective postoperative care to patients in the recovery phase after anesthesia and surgery.