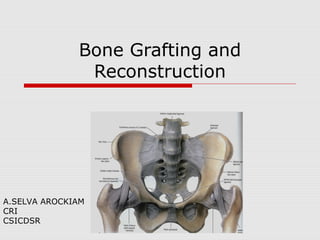
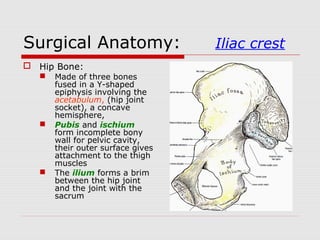
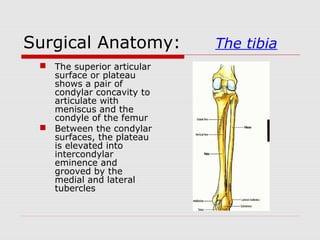
The document provides information on bone grafting and reconstruction. It discusses the historical background of bone grafting gaining experience from wars. It then describes the three biological mechanisms involved in bone grafting: osteogenesis, osteoconduction, and osteoinduction. The document proceeds to provide detailed information on the surgical anatomy of potential bone graft harvesting sites, including the rib, iliac crest, and tibia. It describes the structural features and harvesting procedures for each bone.