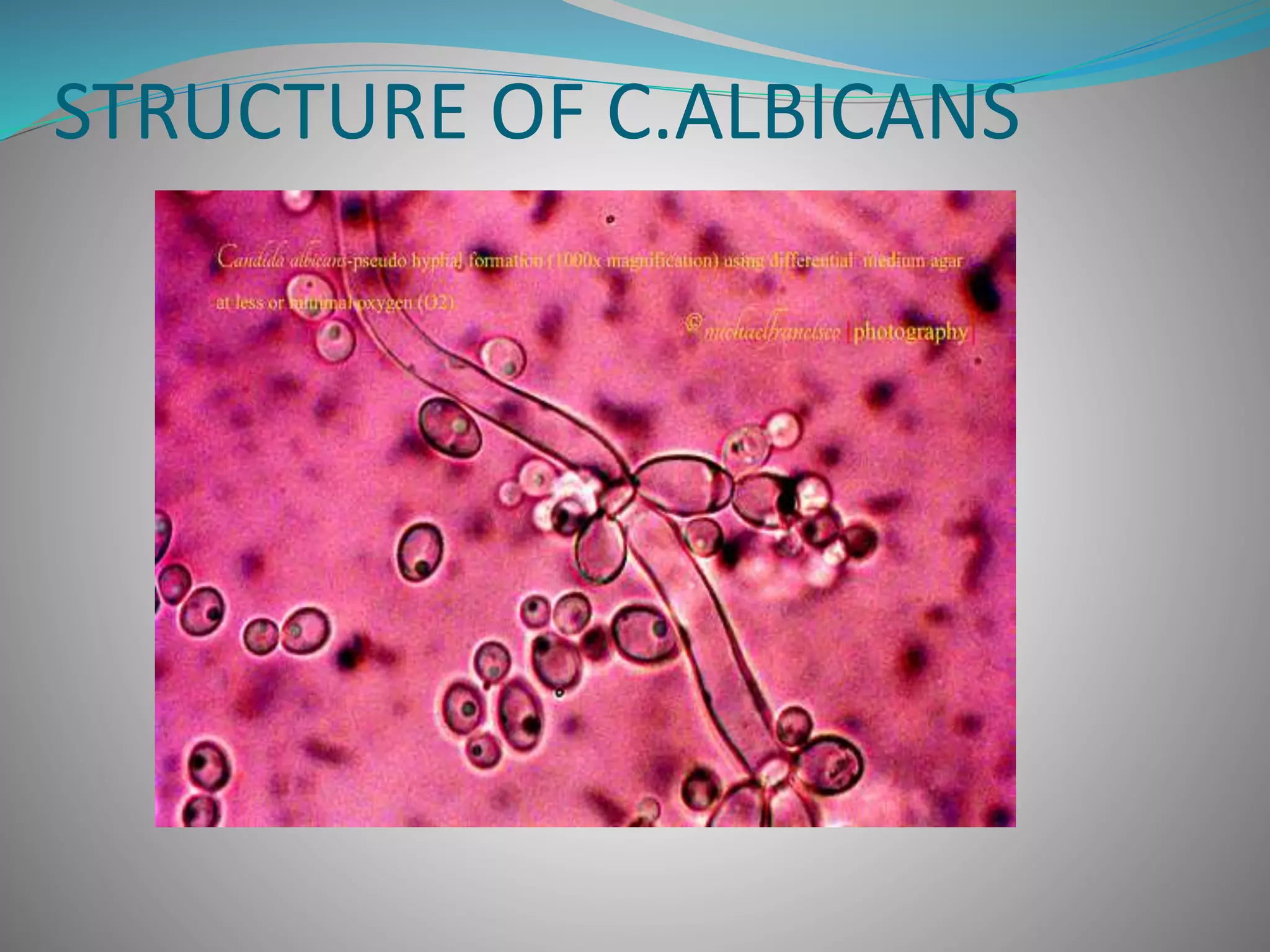
Candida albicans is a yeast that can cause infections in humans. It normally lives harmlessly in the body but can overgrow and cause disease when the environment changes. It has several forms ranging from yeast to hyphal filaments. Over 75% of women experience at least one vaginal candidiasis infection. Risk factors include antibiotics use, pregnancy, diabetes, and weakened immune system. Symptoms depend on the infected area and include rashes, vaginal discharge, and oral thrush. Diagnosis involves microscopic examination of samples. Treatment involves topical or oral antifungal drugs like fluconazole that work by disrupting the fungal cell membrane or inhibiting ergosterol production. Prevention focuses on good