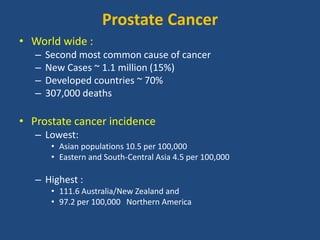
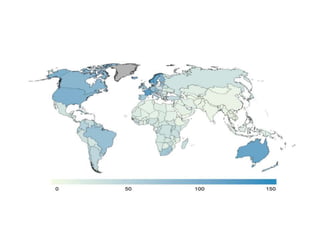
Prostate cancer is the second most common cancer globally, with varying incidence rates influenced by geography and lifestyle changes. In India, prostate cancer cases are rising due to urban migration and increased medical awareness, with current rates approaching those in Western countries. Treatment options vary by stage, including watchful waiting, surgery, radiation therapy, and hormonal treatment, each tailored to patient-specific factors.


















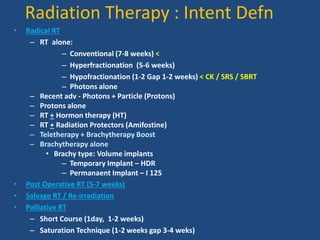
![Overview Treatment Options by Stage for Prostate Cancer
Stage ( AJCC TNM Staging Criteria) Standard Treatment Options
Stage I •Watchful waiting or active surveillance
•Radical prostatectomy
•External-beam radiation therapy (EBRT)
•Interstitial implantation of radioisotopes
Stage II •Watchful waiting or active surveillance
•Radical prostatectomy
•External-beam radiation therapy (EBRT) with or without hormonal therapy
•Interstitial implantation of radioisotopes
Stage III •External-beam radiation therapy (EBRT) with or without hormonal therapy
•Hormonal manipulations (orchiectomy or luteinizing hormone-releasing hormone [LH-RH] agonist)
•Radical prostatectomy with or without EBRT
•Watchful waiting or active surveillance
Stage IV •Hormonal manipulations
•Bisphosphonates
•External-beam radiation therapy (EBRT) with or without hormonal therapy
•Palliative radiation therapy
•Palliative surgery with transurethral resection of the prostate (TURP)
•Watchful waiting or active surveillance
Recurrent •Chemotherapy for hormonal management of prostate cancer
•Immunotherapy](https://image.slidesharecdn.com/radiationtherapyinprostatecancer2014-141001084406-phpapp01/85/Radiation-therapy-in-prostate-cancer-22-320.jpg)