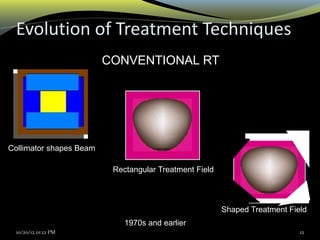
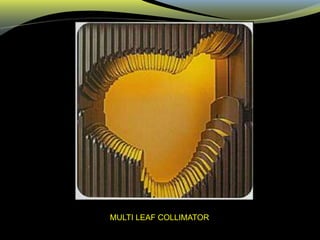
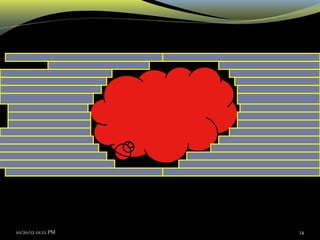
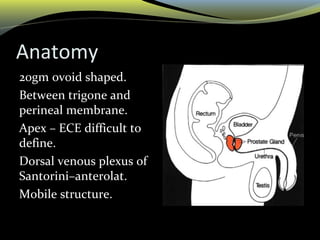
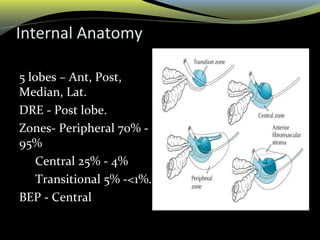
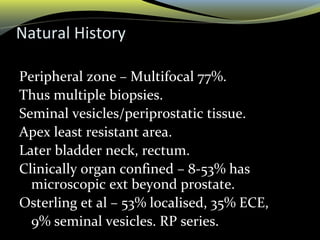
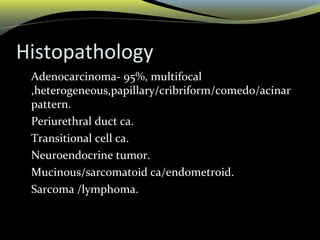
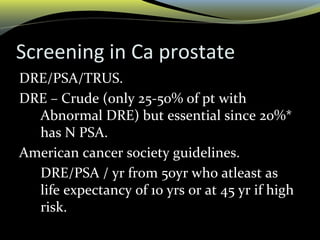
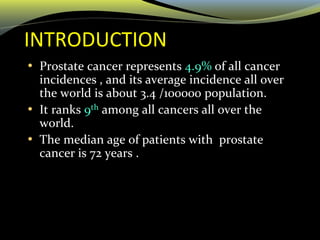
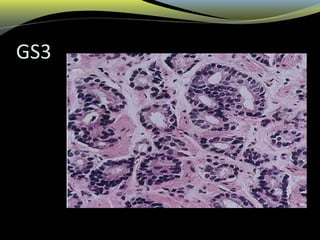
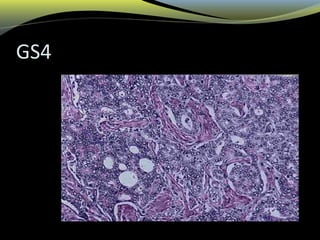
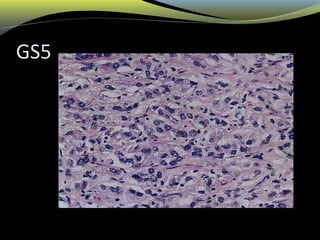
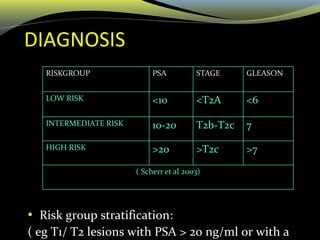
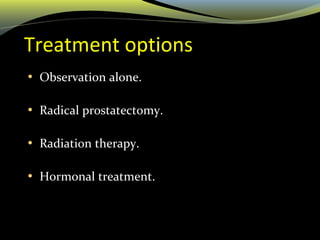
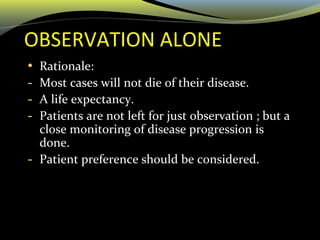
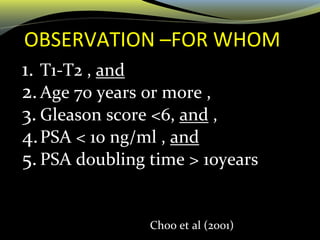
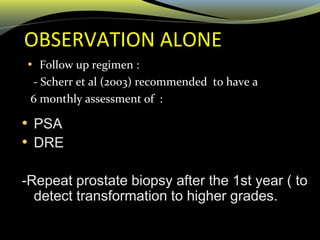
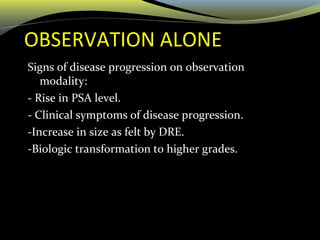
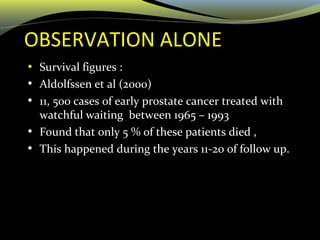
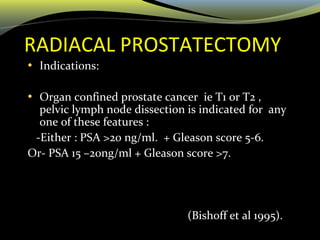
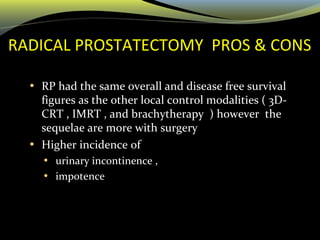
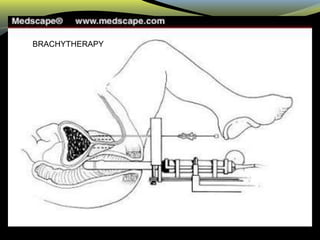
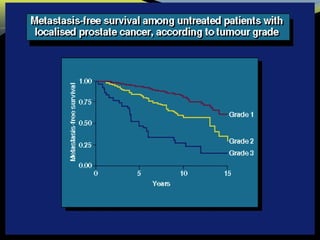
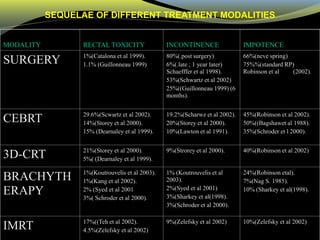
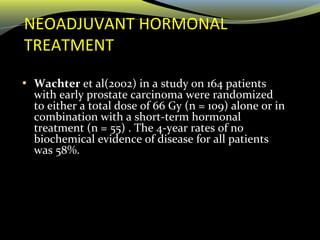
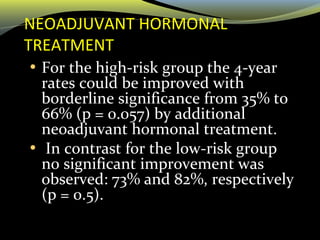
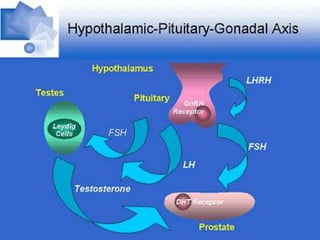
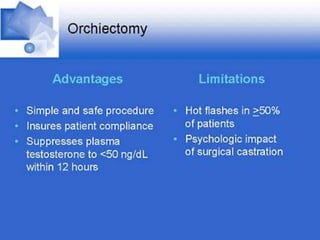
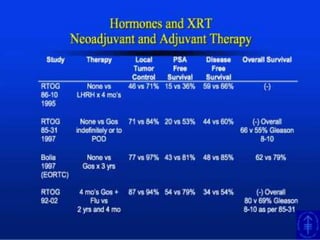
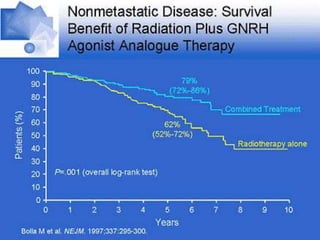
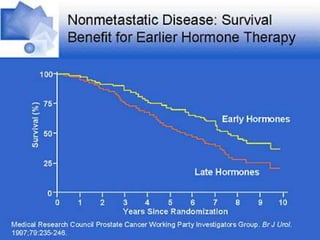
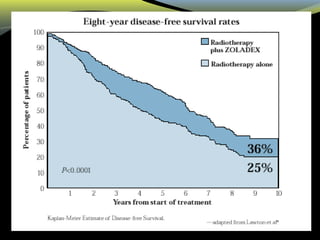
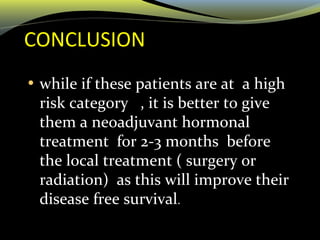
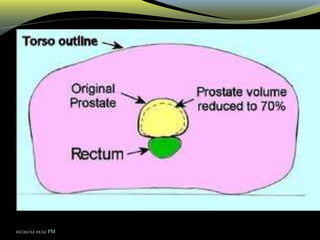
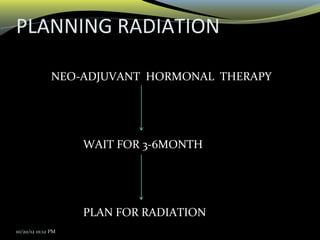
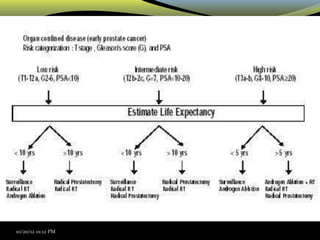
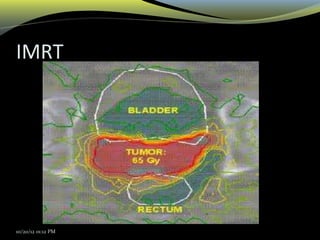
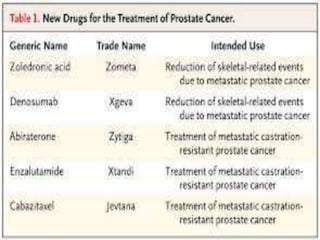
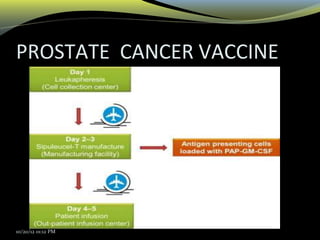
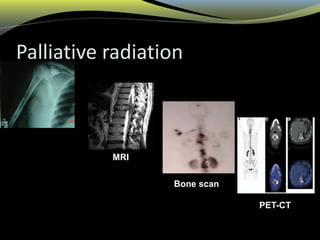
This document discusses the radiotherapeutic management of prostate cancer. It begins by introducing the multidisciplinary team involved in diagnosis and treatment. It then covers diagnosis, including various screening tests and pathology findings. Treatment options discussed include observation, surgery, radiation therapy and hormonal treatment. The document focuses on the evolution of radiation techniques from conventional to IMRT and brachytherapy. It compares outcomes and side effects of different local treatment modalities and discusses the role of neoadjuvant hormonal therapy.
![Dr. Kanhu Charan Patro
M.D,D.N.B[RT],P.D.C.R,C.E.P.C,FSIOP,FAROI
[EX – TATA MEMORIAL HOSPITAL]
Chief Consultant- Radiation Oncology
MAHATMA GANDHI CANCER HOSPITAL
VISAKHAPATNAM
Email-drkcpatro@gmail.com ,M-09160470564
RADIOTHRPEUTIC MANAGEMENT OF PROSTATE CANCER](https://image.slidesharecdn.com/mgchprostate-210305001334/75/PROSTATE-CANCER-IN-NUTSHELL-1-2048.jpg)