This document discusses prostate cancer, including:
1. Prostate cancer is one of the most common cancers in men and usually grows slowly initially remaining confined to the prostate gland.
2. The main types of prostate cancer are adenocarcinoma and rare subtypes like small cell carcinoma and sarcomas.
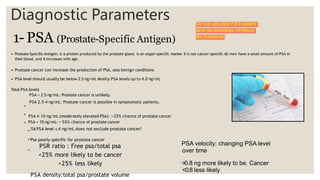
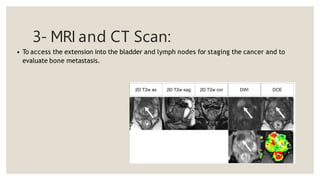
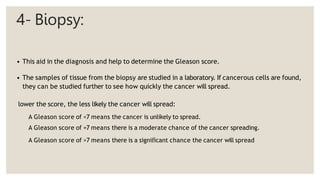
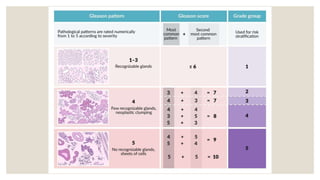
3. Diagnostic tests include a digital rectal exam, PSA testing, MRI/CT scans, transrectal ultrasound, and biopsy to determine Gleason score.