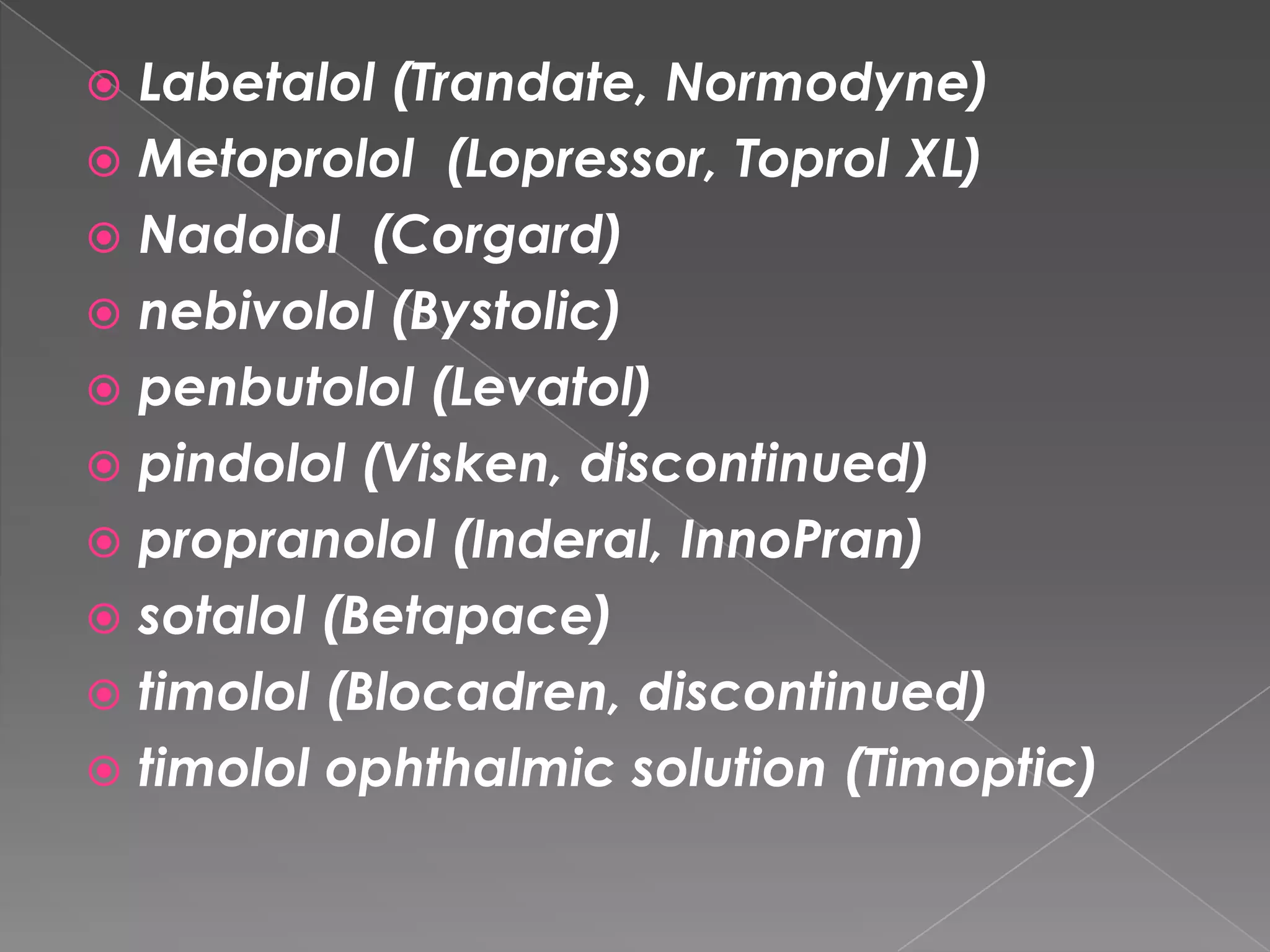
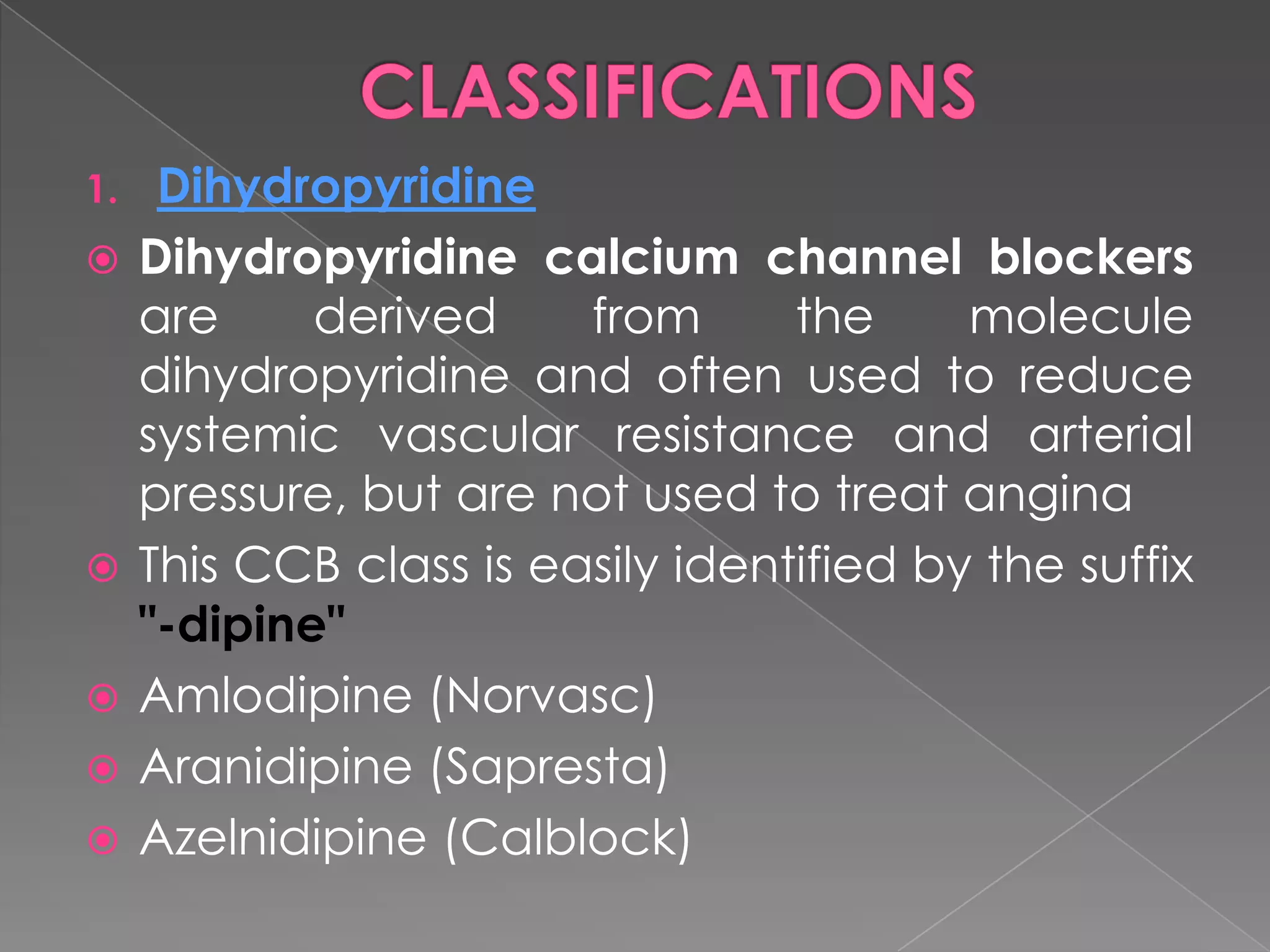
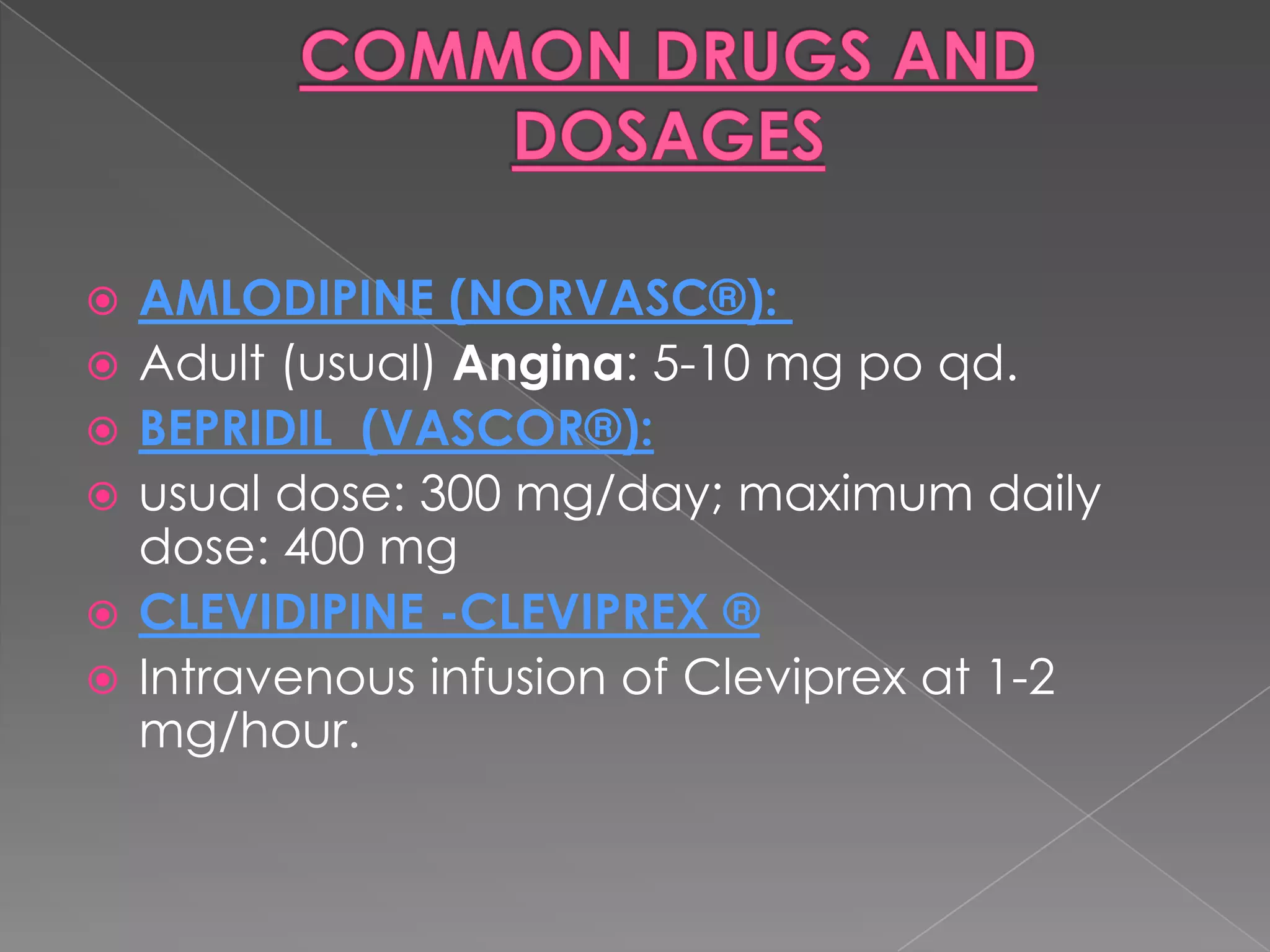
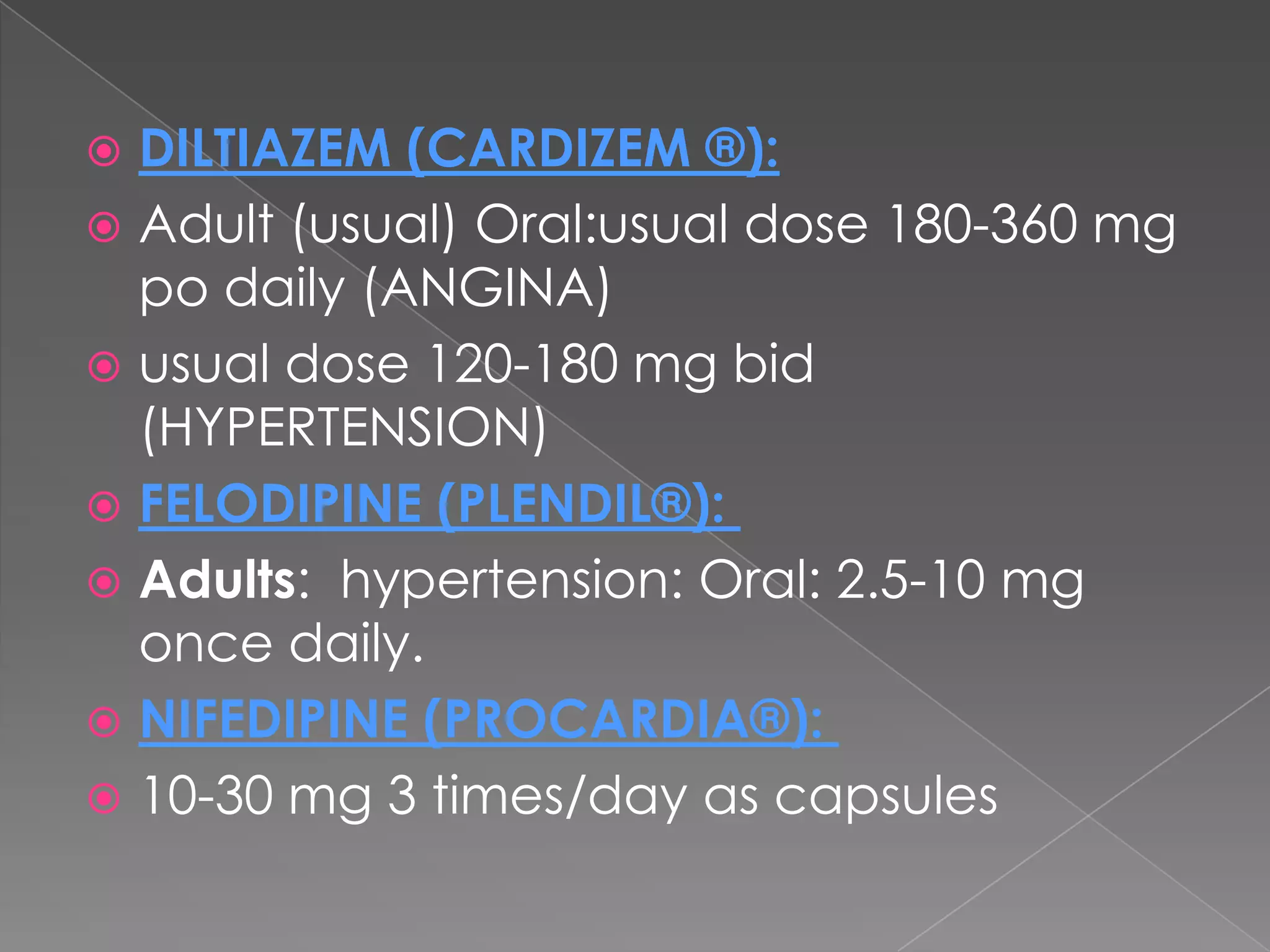
Beta blockers and calcium channel blockers are widely used to treat cardiovascular disease. The first beta blocker, dichloroisoproterenol, was synthesized in 1958. Sir James Black discovered the first clinically significant beta blockers, propranolol and pronethalol, in 1962. Calcium channel blockers were first identified in 1964 and block the movement of calcium through calcium channels. Common types include dihydropyridines, phenylalkylamines, and benzothiazepines.