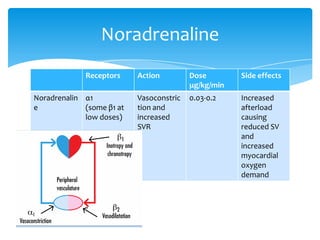
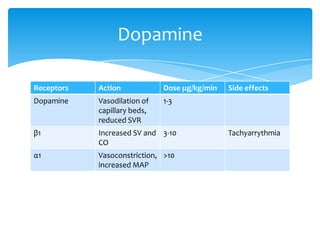
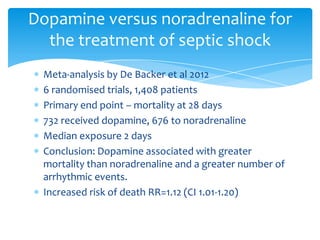
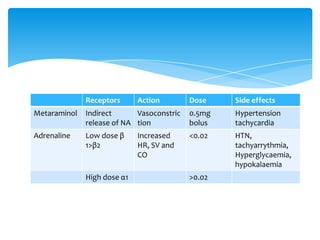
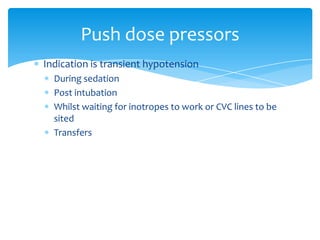
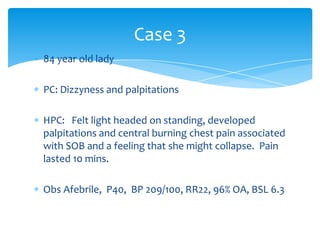
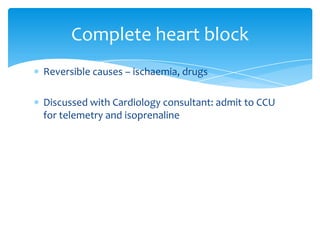
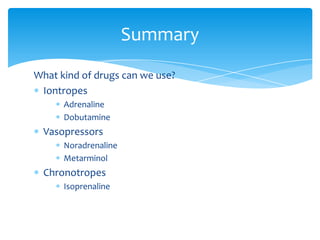
This document discusses the use of inotropes and vasopressors in the emergency department for management of shock. It provides an overview of different drug classes including their mechanisms of action, dosages, and side effects. Case studies are presented to demonstrate how these drugs may be used in scenarios involving hypotension, shock, and heart block. Key drugs discussed include norepinephrine, dopamine, adrenaline, metaraminol, and isoprenaline. The document emphasizes the importance of determining the type of shock and selecting an appropriate drug to increase cardiac output, systemic vascular resistance, or both depending on the clinical situation.
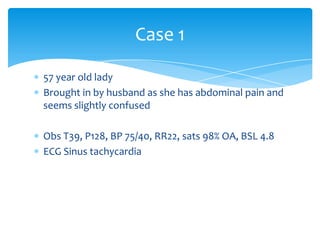
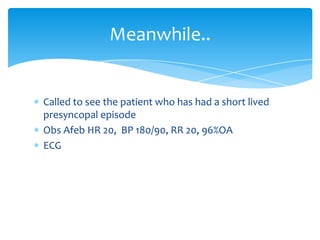
![Shock
Shock is the failure to adequately oxygenate tissues
to meet metabolic demand, resulting in end organ
failure.
Adjustable factors affecting tissue oxygenation
[Hb]
PaO2
Cardiac output
Systemic vascular resistance](https://image.slidesharecdn.com/inotropes-140219210427-phpapp01/85/Ionotropes-and-vasopressor-use-in-the-ED-5-320.jpg)