1) Frailty refers to a loss of physiologic reserve that makes older adults susceptible to disability from minor stresses or challenges. It is not dependent on age, diagnosis, or functional ability.
2) Common features of frailty include weakness, weight loss, muscle wasting, exercise intolerance, frequent falls, immobility, and instability of chronic diseases.
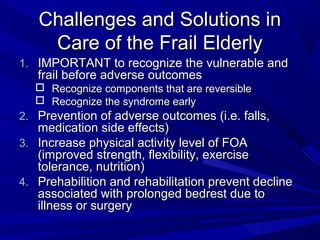
3) Frailty exists on a continuum from vigorous to frail. Early intervention can help reduce disability and adverse outcomes like falls, injuries, hospitalizations, and death in frail older adults.



![Associated Features of Frailty
Older Age
Female
Less Education
Lower Income
Poorer Health (Multiple co-morbid
chronic disease)
(Fried et al [2001], Community-based study)](https://image.slidesharecdn.com/frailty-130113073935-phpapp02/85/Frailty-7-320.jpg)











![Advancing Health and Well Being
Into Old Age in Filipino Society
(Philippine [Inter-Agency] and DSWD Plan of Action CY 2007)
1. Advocacy on prevention of common diseases
2. Conduct regular medical check-up of senior
citizens in rural health units (RHU).
3. Conduct care giving trainings to families of sick
and frail senior citizens
4. Conduct seminars on gerontology, physical
fitness program, nutrition education and dietary
counseling](https://image.slidesharecdn.com/frailty-130113073935-phpapp02/85/Frailty-24-320.jpg)
![Advancing Health and Well Being
Into Old Age in Filipino Society
(Philippine [Inter-Agency] and DSWD Plan of Action CY 2007)
5. Establish geriatric wards in government
and private hospitals.
6. Implementation of neighborhood support
services for older persons (NSSOP).
7. Ensure the implementation of the
Philippine Plan of Action for Nutrition
(PPAN) as a blueprint and country’s
guide for action to achieve nutritional
adequacy for Filipinos](https://image.slidesharecdn.com/frailty-130113073935-phpapp02/85/Frailty-25-320.jpg)
