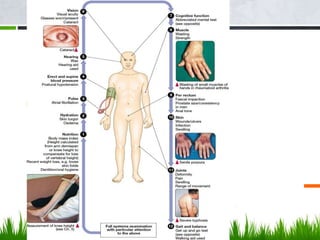
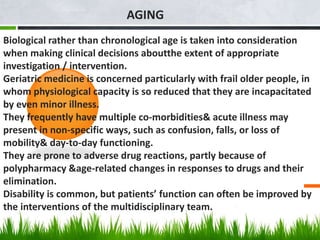
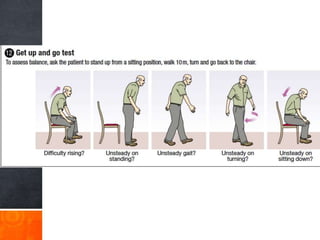
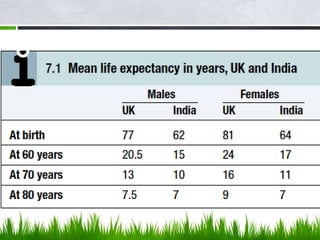
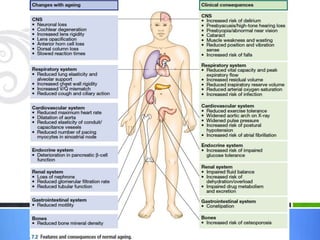
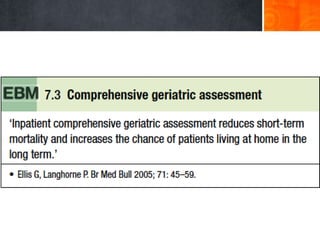
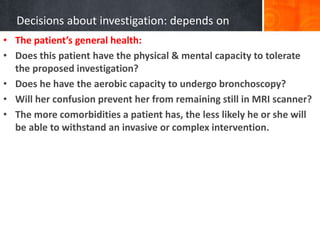
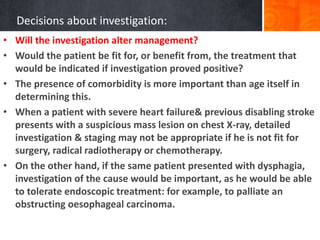
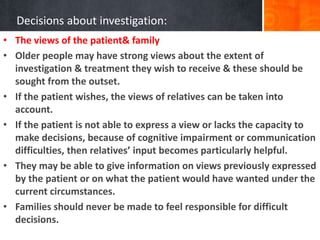
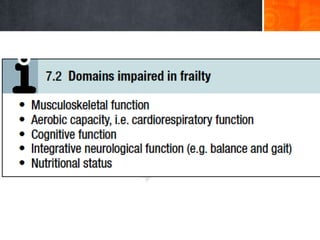
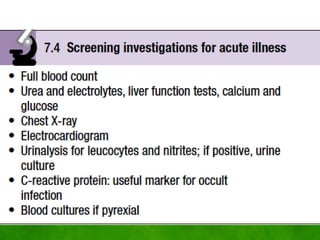
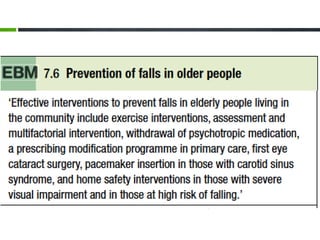
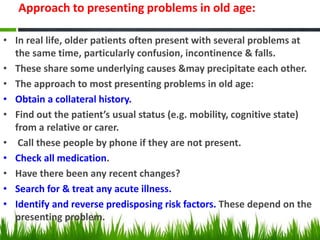
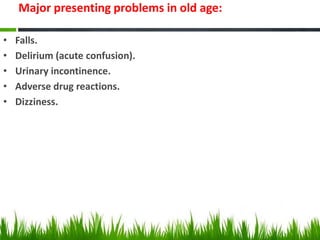
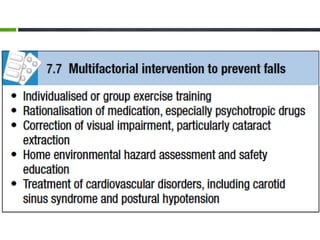
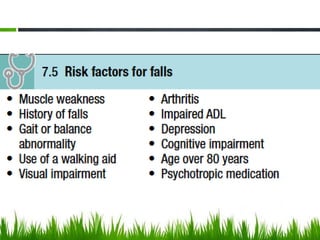
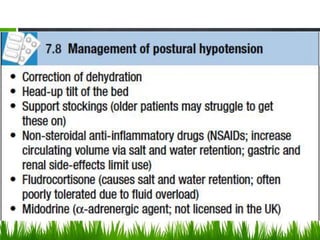
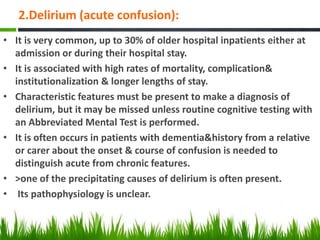
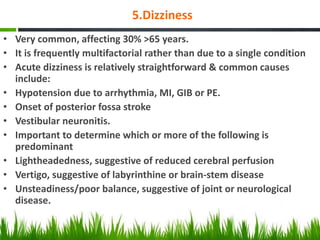
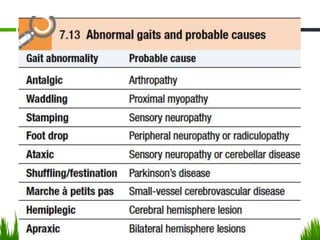
Geriatric medicine focuses on frail older patients whose health is easily impacted by minor illness. These patients often have multiple medical issues and atypical presentations of conditions. Decisions about their care require considering biological age, tolerance for interventions, impact on management, and patient/family preferences. Falls are a major problem and can result from acute illness, syncope, or mechanical issues like weakness, poor vision or balance. Thorough evaluation and targeting modifiable risk factors can help prevent falls and fractures in older adults.