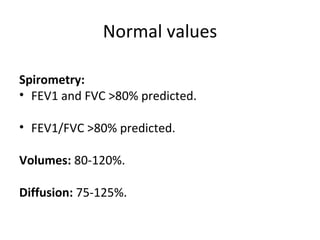
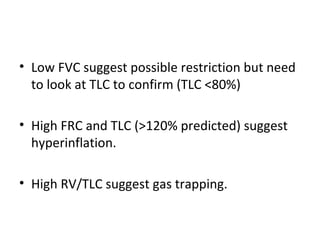
Pulmonary function testing involves analyzing flow volume loops, lung volumes, and gas diffusion.
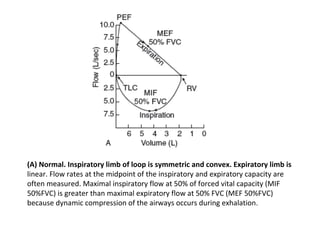
(1) A normal loop has a symmetric, convex inspiratory limb and linear expiratory limb, with maximal inspiratory flow greater than maximal expiratory flow due to dynamic compression.
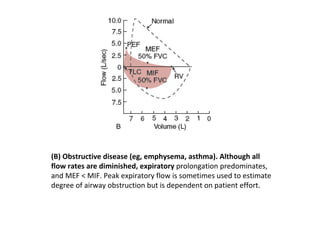
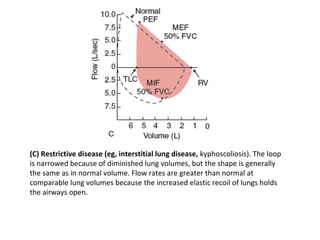
(2) Obstructive diseases like asthma show diminished expiratory flow predominating over inspiratory flow. Restrictive diseases narrow the loop but maintain shape due to increased elastic recoil.
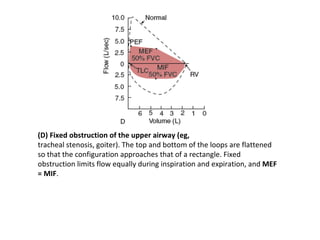
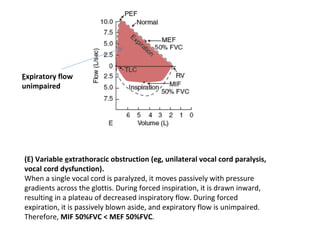
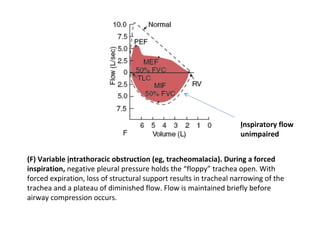
(3) Fixed or variable upper airway obstructions flatten the loop, while variable lower airway obstructions create inspiratory or expiratory plateaus depending on the location of obstruction.