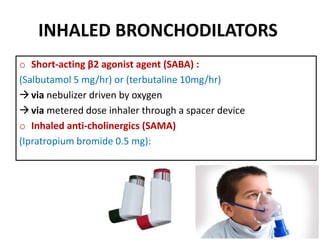
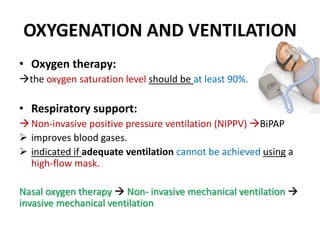
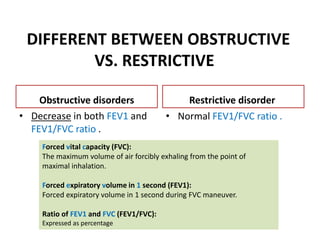
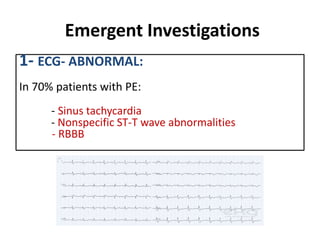
This document discusses the treatment of acute exacerbations of asthma and COPD. For asthma, treatment involves high doses of inhaled bronchodilators, systemic corticosteroids, oxygen therapy, and intravenous fluids. For COPD, treatment focuses on oxygenation, ventilation support using non-invasive ventilation if needed, nebulized short-acting bronchodilators, corticosteroids, and antibiotics for bacterial infections. Lung volumes measured via spirometry can differentiate obstructive disorders like COPD and asthma from restrictive disorders. Obstructive disorders show reduced airflow and FEV1/FVC ratio, while restrictive disorders have normal ratio but reduced lung volumes. Emergent tests for diagnosis include ECG, arterial blood gases,