Goniometry is the measurement of joint range of motion using a goniometer. There are several types of validity and reliability that are important when assessing measurement tools like goniometry. Validity refers to how well a test measures what it intends to, including face validity, construct validity, and criterion-related validity. Reliability is the degree to which repeated measurements provide consistent results and includes test-retest reliability, parallel forms reliability, and internal consistency reliability. Goniometry involves aligning a goniometer's arms according to bony landmarks and measuring active or passive range of motion in degrees. Several factors can affect range of motion measurements and different joints have characteristic capsular patterns when soft tissues are impaired.








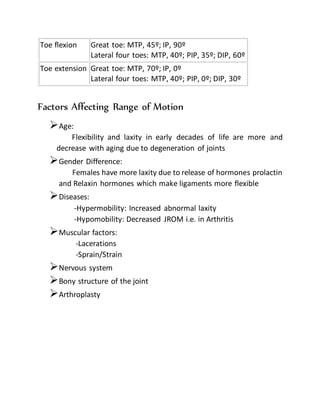
![Hip Flexion
Extension
Abduction
Adduction
Internal rotation
External rotation
0°-100°
0°-30°
0°-40°
0°-20°
0°-40°
0°-50°
Knee Flexion 0°-150°
Ankle Plantarflexion
Dorsiflexion
0°-40°
0°-20°
Foot Inversion
Eversion
0°-30°
0°-20°
Active range of motion norms for the hand and fingers
Motion Degrees
Finger flexion MCP:85°-90°; PIP: 100°-115°; DIP: 80°-90°
Finger extension MCP:30°-45°; PIP: 0°; DIP: 20°
Finger abduction 20°-30°
Finger adduction 0°
Thumb flexion CMC: 45°-50°; MCP: 50°-55°; IP: 85°-90°
Thumb extension MCP: 0°; IP: 0°-5°
Thumb adduction 30°
Thumb abduction 60°-70°
Normal ranges of motion, and end feels, for the toes[2, 3]
Motion Normal Range (Degrees)](https://image.slidesharecdn.com/goniometrydocument-170926071823/85/Goniometry-13-320.jpg)