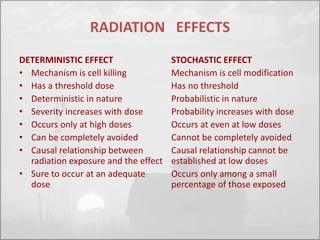
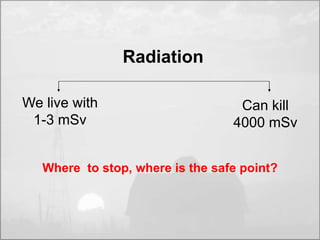
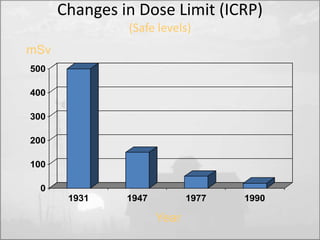
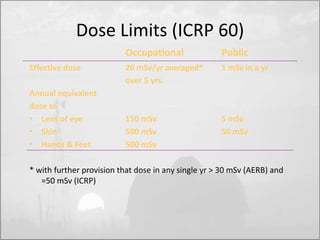
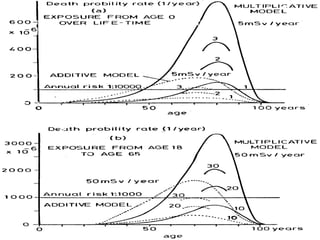
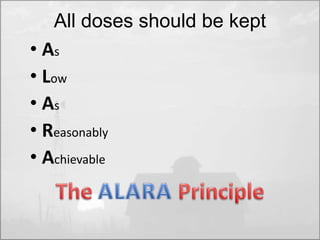
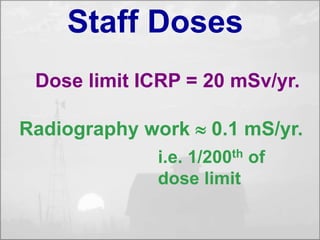
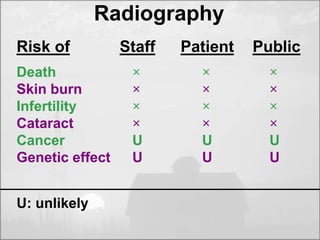
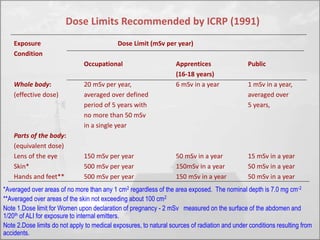
The objectives of radiation protection according to the ICRP and NCRP are to prevent serious radiation effects and reduce stochastic effects to acceptable levels while allowing beneficial practices involving radiation exposure. This is achieved through principles of justification, optimization and dose limitation. Justification requires that practices only be adopted if benefits outweigh radiation risks. Optimization aims to keep exposures as low as reasonably achievable. Dose limitation sets defined exposure limits for workers and the public.



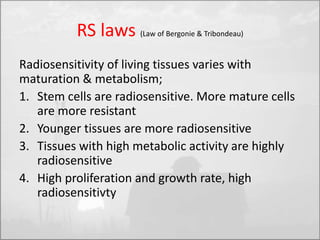
![Radiosensitivity [RS]
• RS = Probability of a cell,
tissue or organ of suffering an
effect per unit of dose.](https://image.slidesharecdn.com/radprotca-141003084618-phpapp02/85/Radiation-Protection-41-320.jpg)