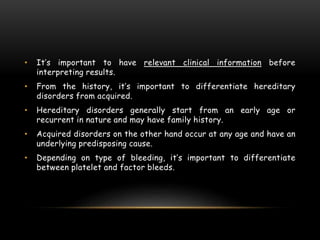
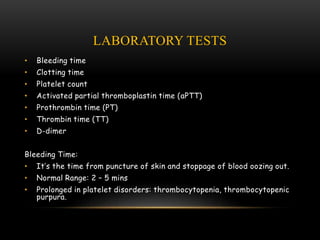
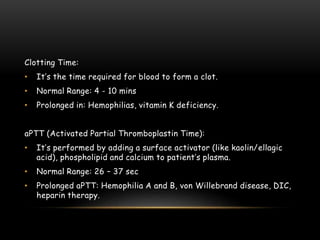
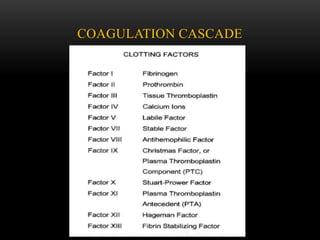
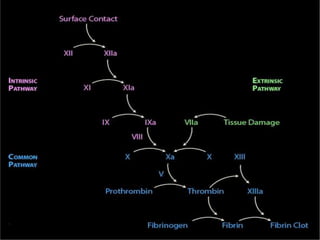
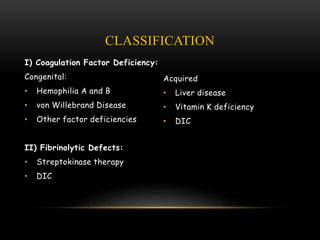
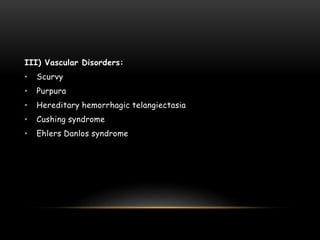
This document discusses bleeding disorders, including their classification and diagnosis. It begins by introducing hemostasis and the coagulation cascade. Bleeding disorders are then classified into four categories: coagulation factor deficiencies, fibrinolytic defects, vascular disorders, and platelet disorders. The diagnosis of bleeding disorders involves considering clinical information like symptoms and family history, as well as laboratory tests such as bleeding time, platelet count, prothrombin time, and D-dimer level. Taking a thorough medical history is important for properly evaluating patients with potential bleeding disorders.
![IV) Platelet Disorders:
1] Quantitative Disorders (Thrombocytopenia):
2] Qualitative Disorders:
Congenital:
• Glanzmann thrombasthenia
• von Willebrand disease
Acquired:
• Liver disease
• Drug-induced
• Alcoholism
Immune Mediated:
• Idiopathic
• Collagen vascular disease
• Sarcoidosis
Non-Immune Mediated:
• Microangiopathic hemolytic anemia
• Leukemia
• Myelofibrosis](https://image.slidesharecdn.com/bleedingdisorder-220222064839/85/Bleeding-Disorders-Classification-and-Diagnosis-10-320.jpg)