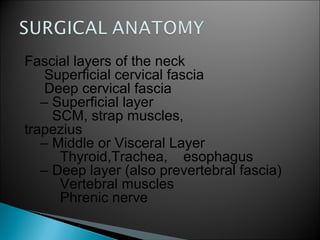
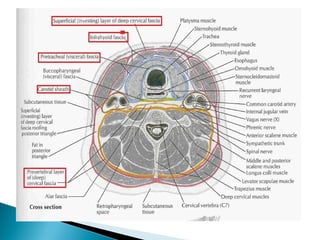
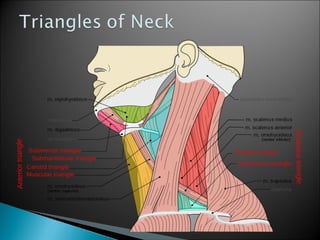
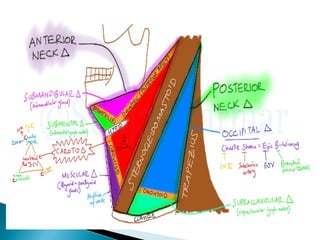
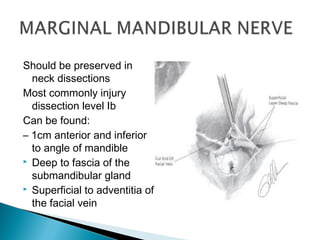
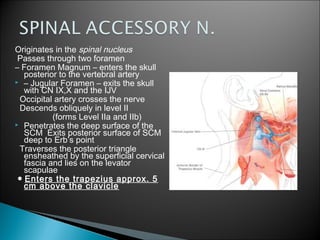
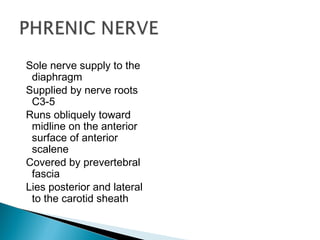
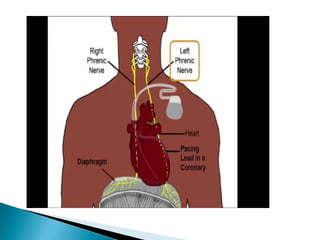
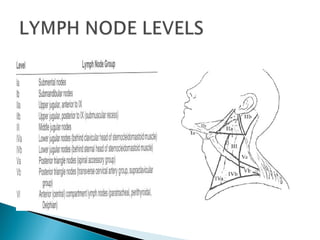
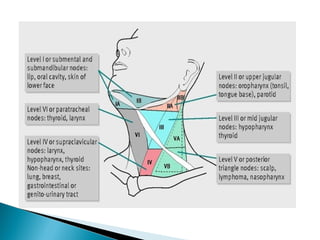
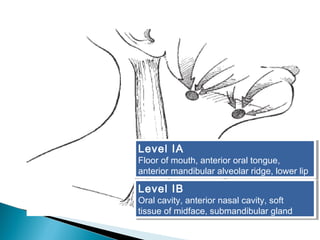
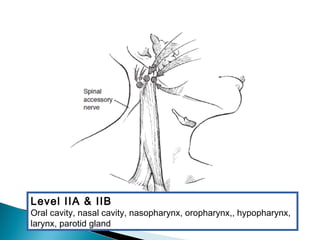
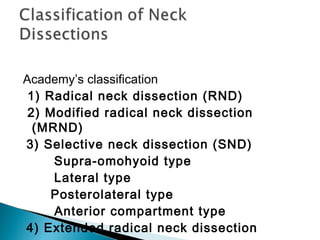
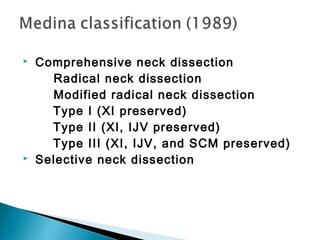
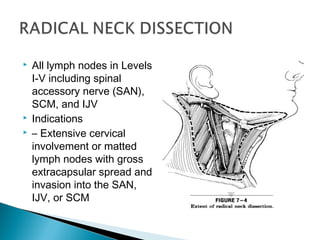
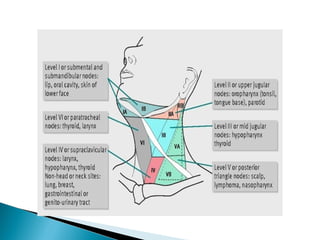
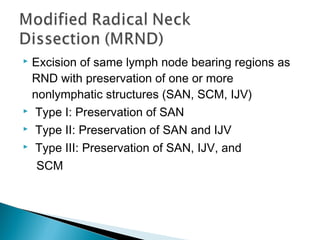
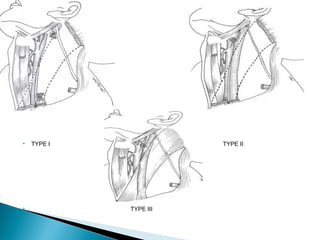
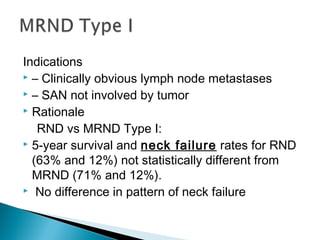
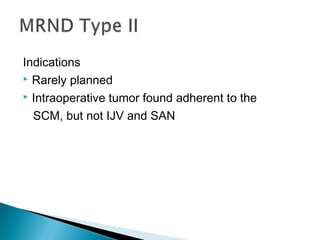
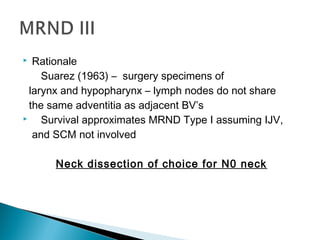
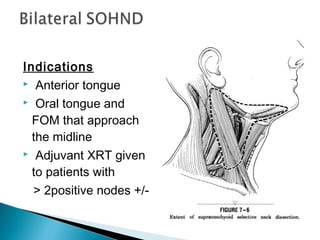
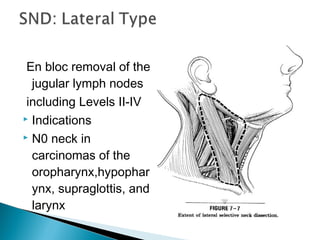
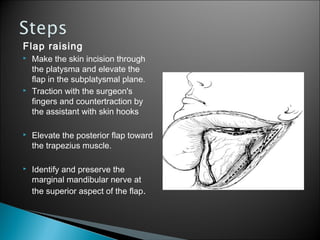
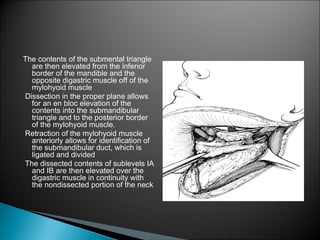
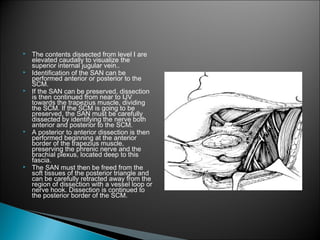
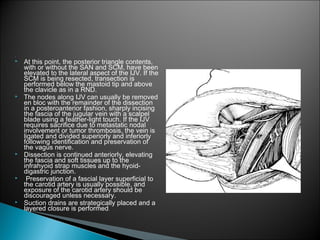
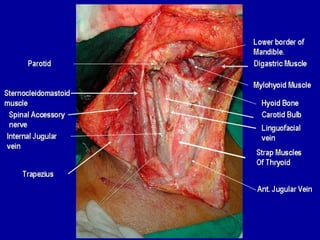
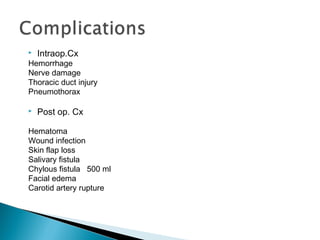
This document discusses neck dissections, including classifications, indications, and techniques. There are several types of neck dissections including radical neck dissection (RND), modified radical neck dissection (MRND), and selective neck dissection (SND). RND removes all lymph nodes from levels I-V while preserving important structures like the spinal accessory nerve (SAN) and internal jugular vein (IJV) distinguishes MRND from RND. SND only removes certain lymph node groups. The document outlines the surgical steps for performing neck dissections and discusses complications.