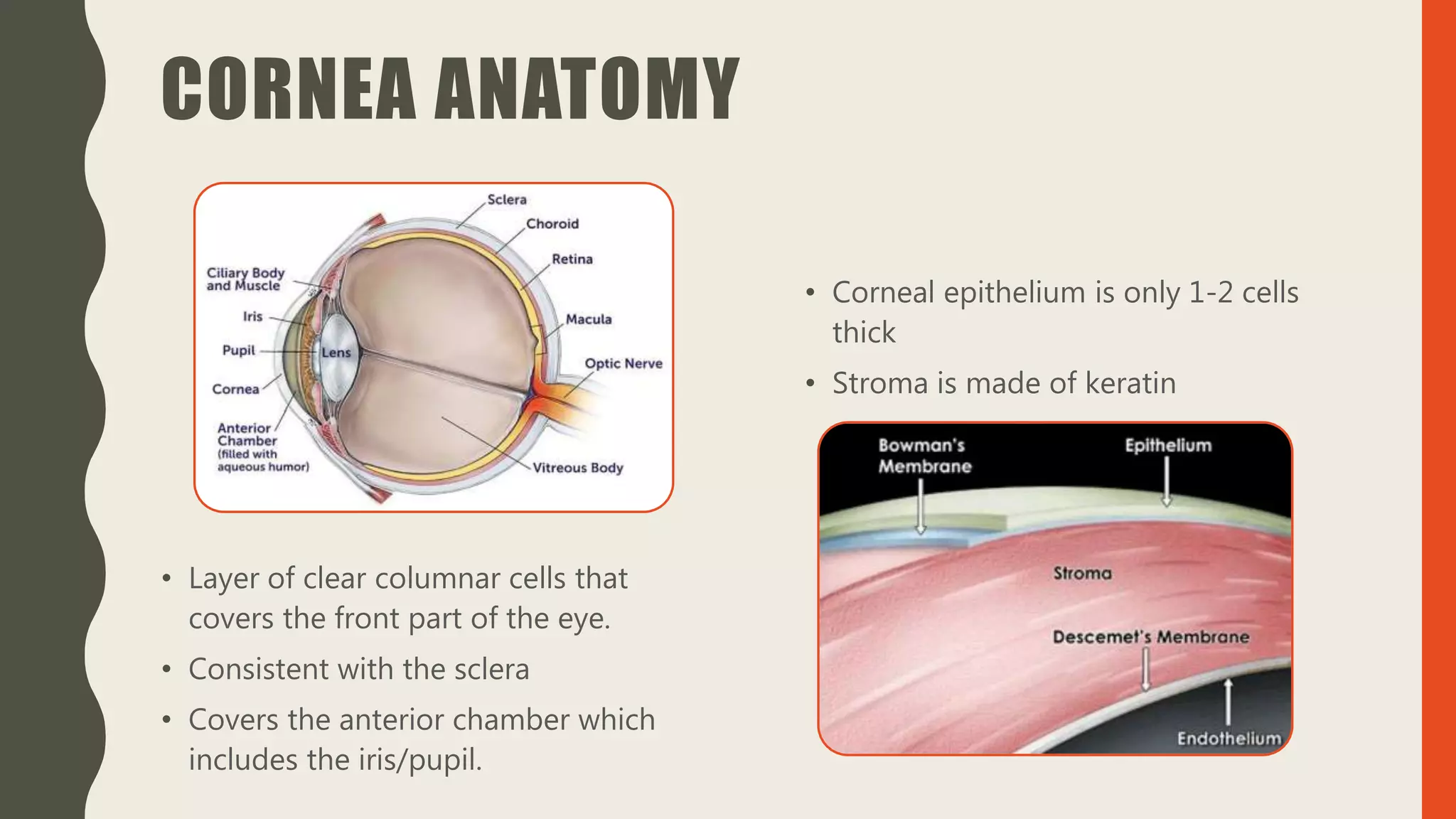
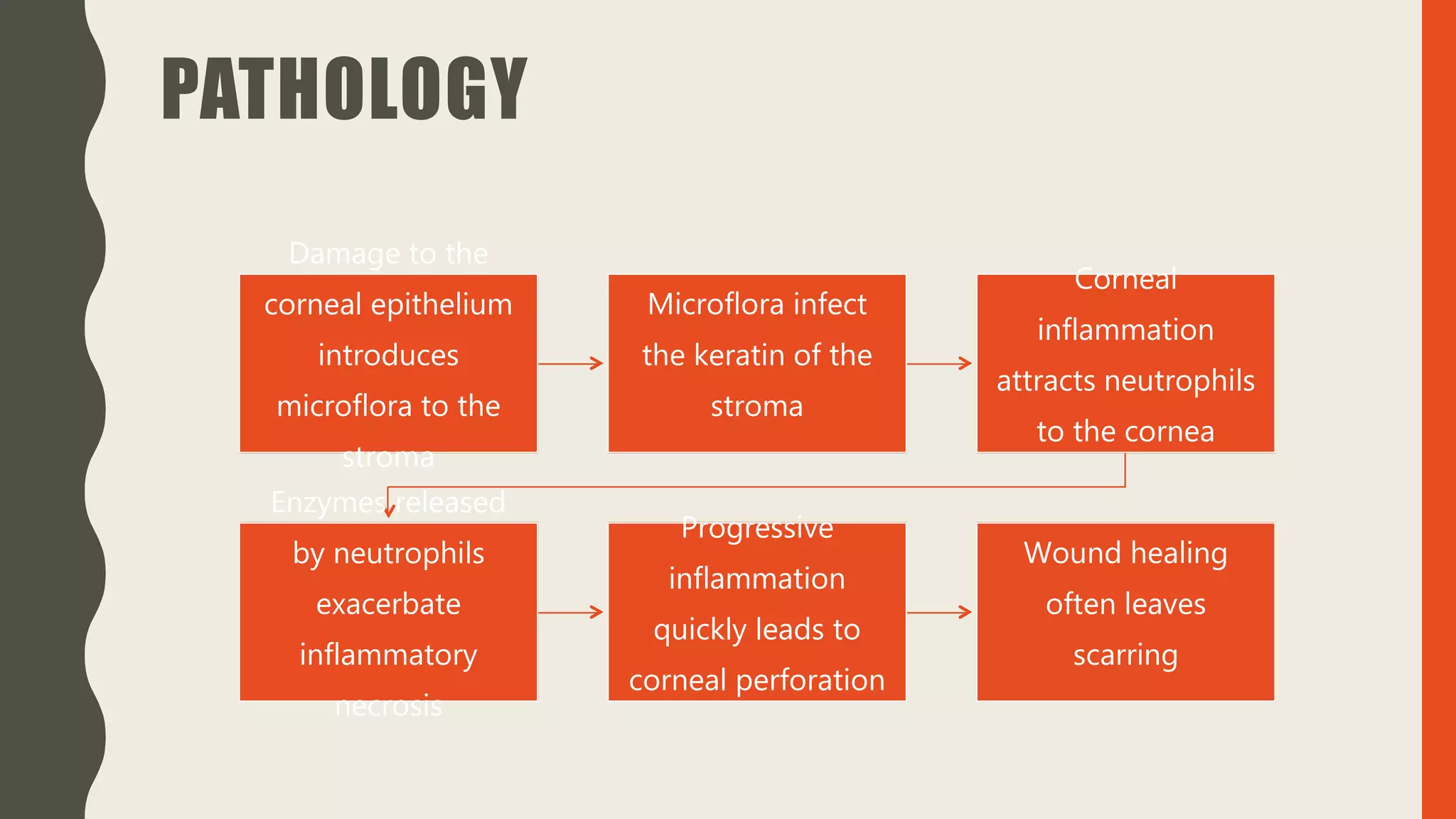
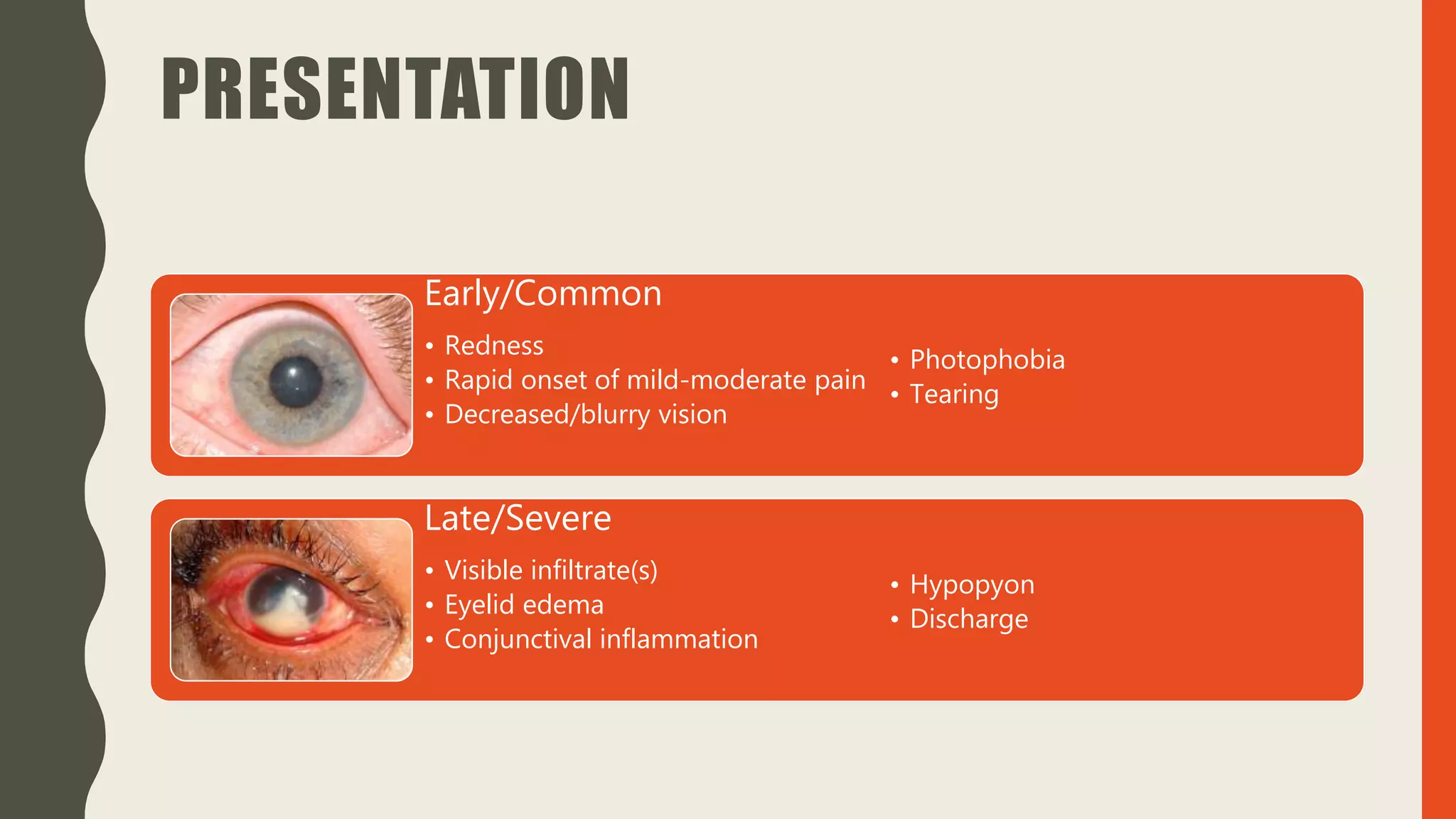
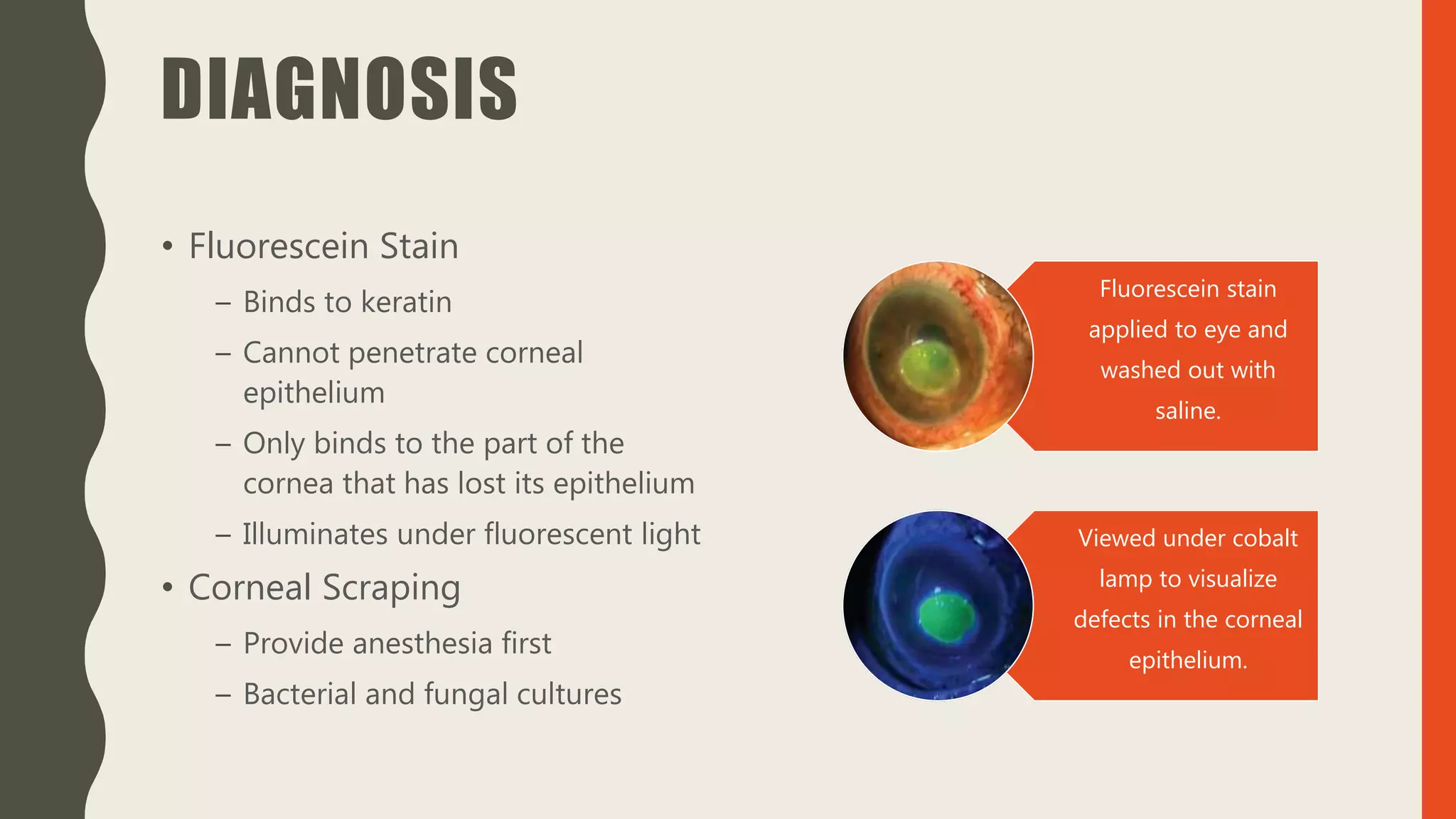
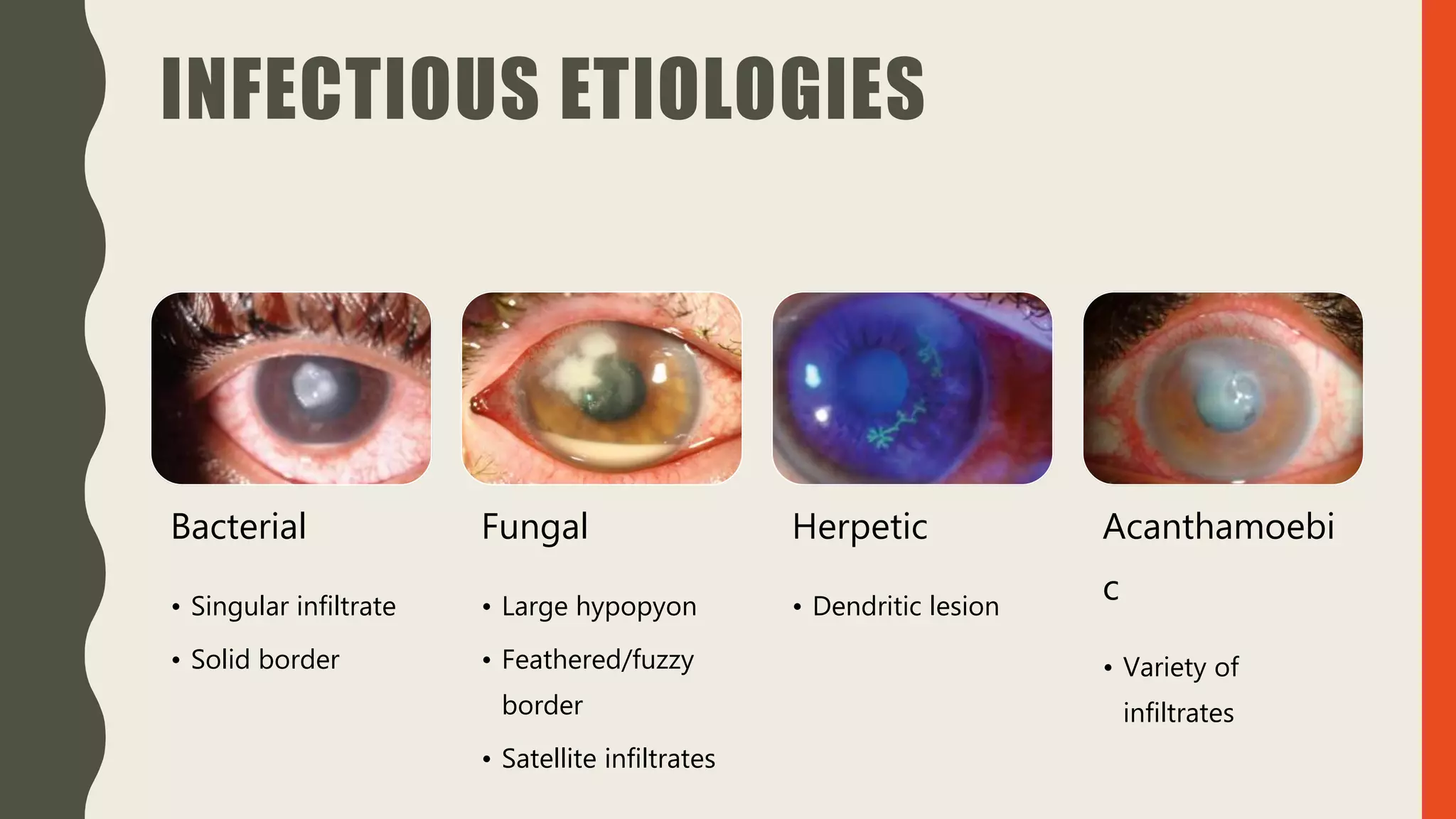
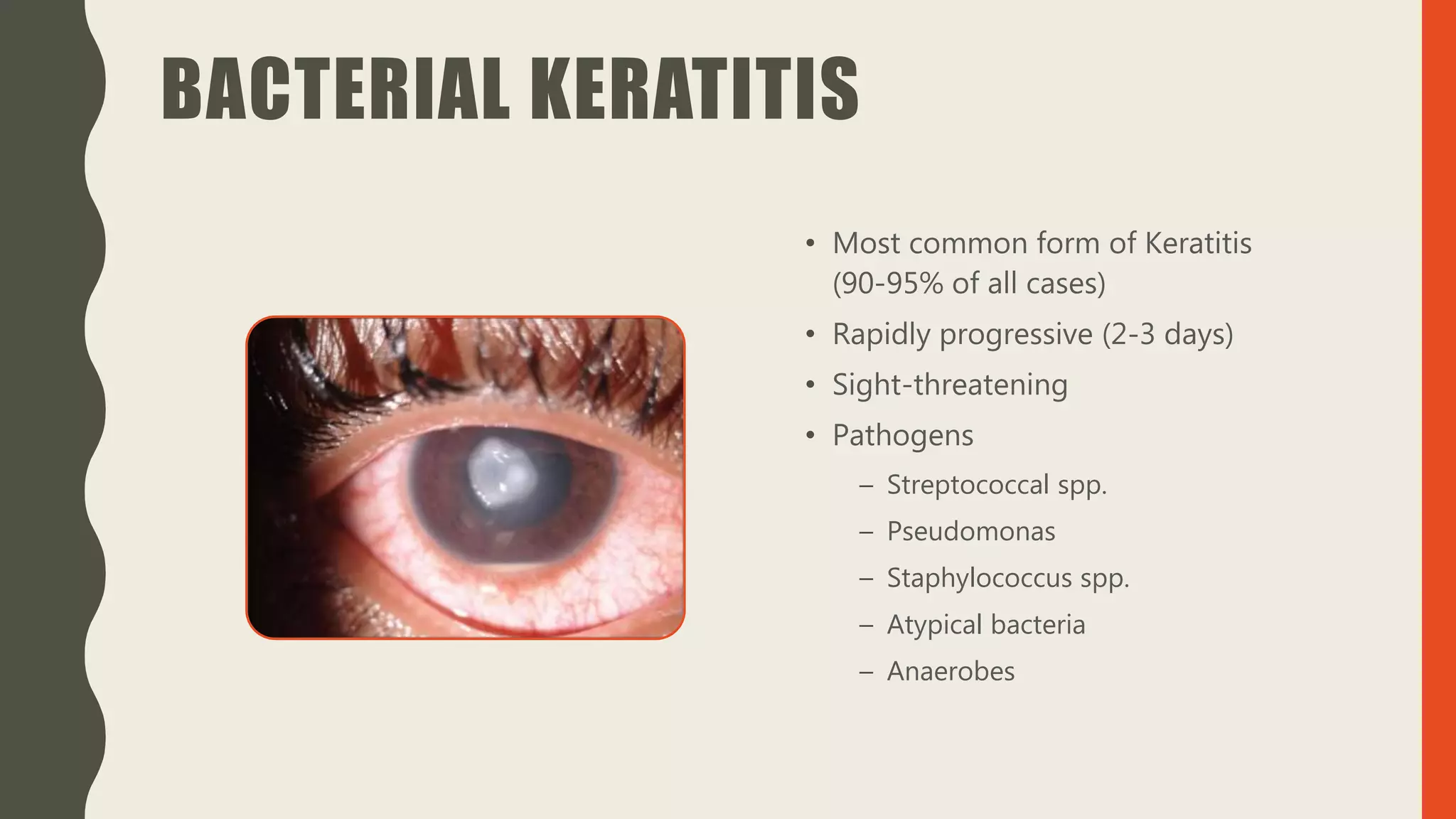
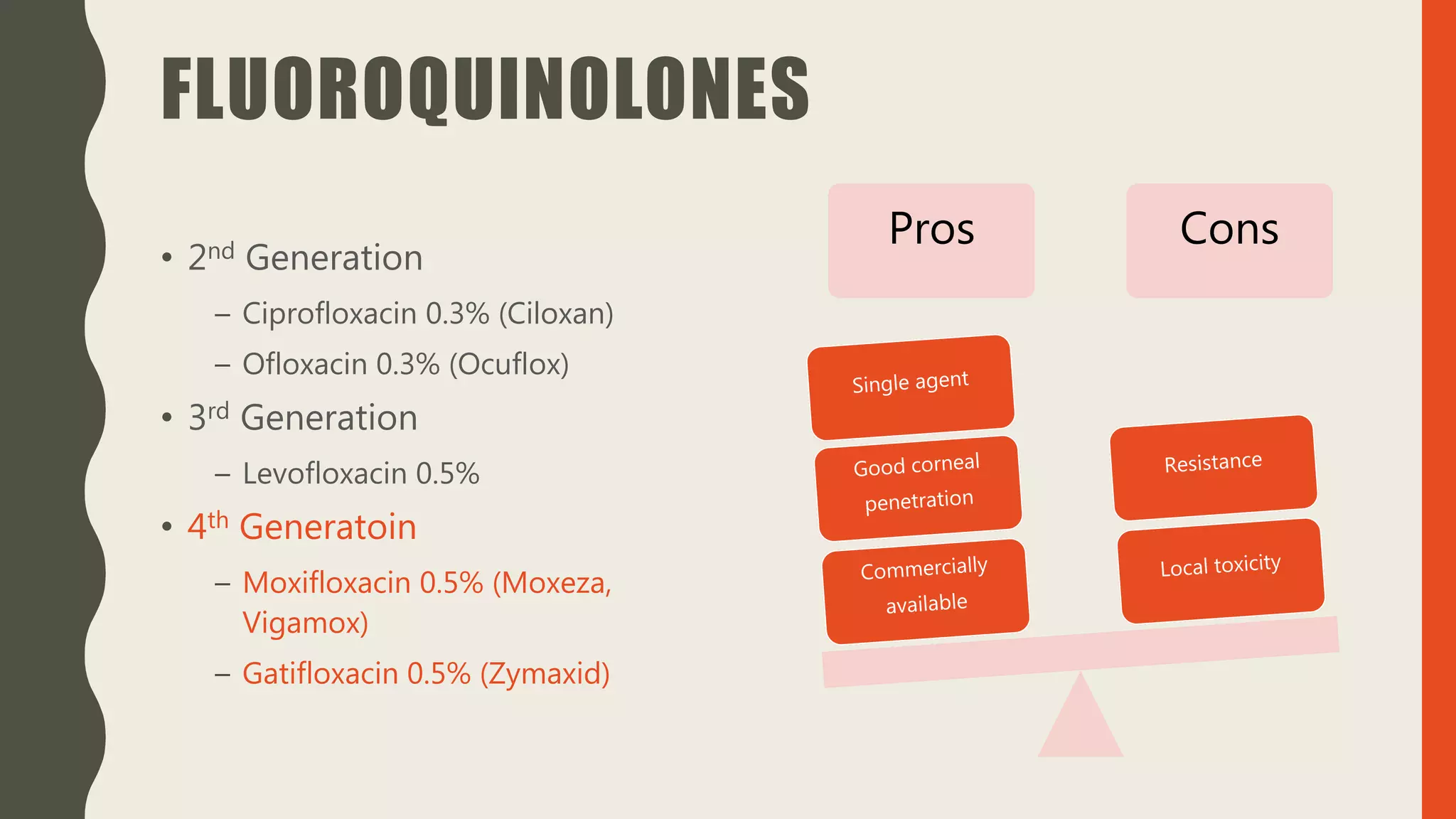
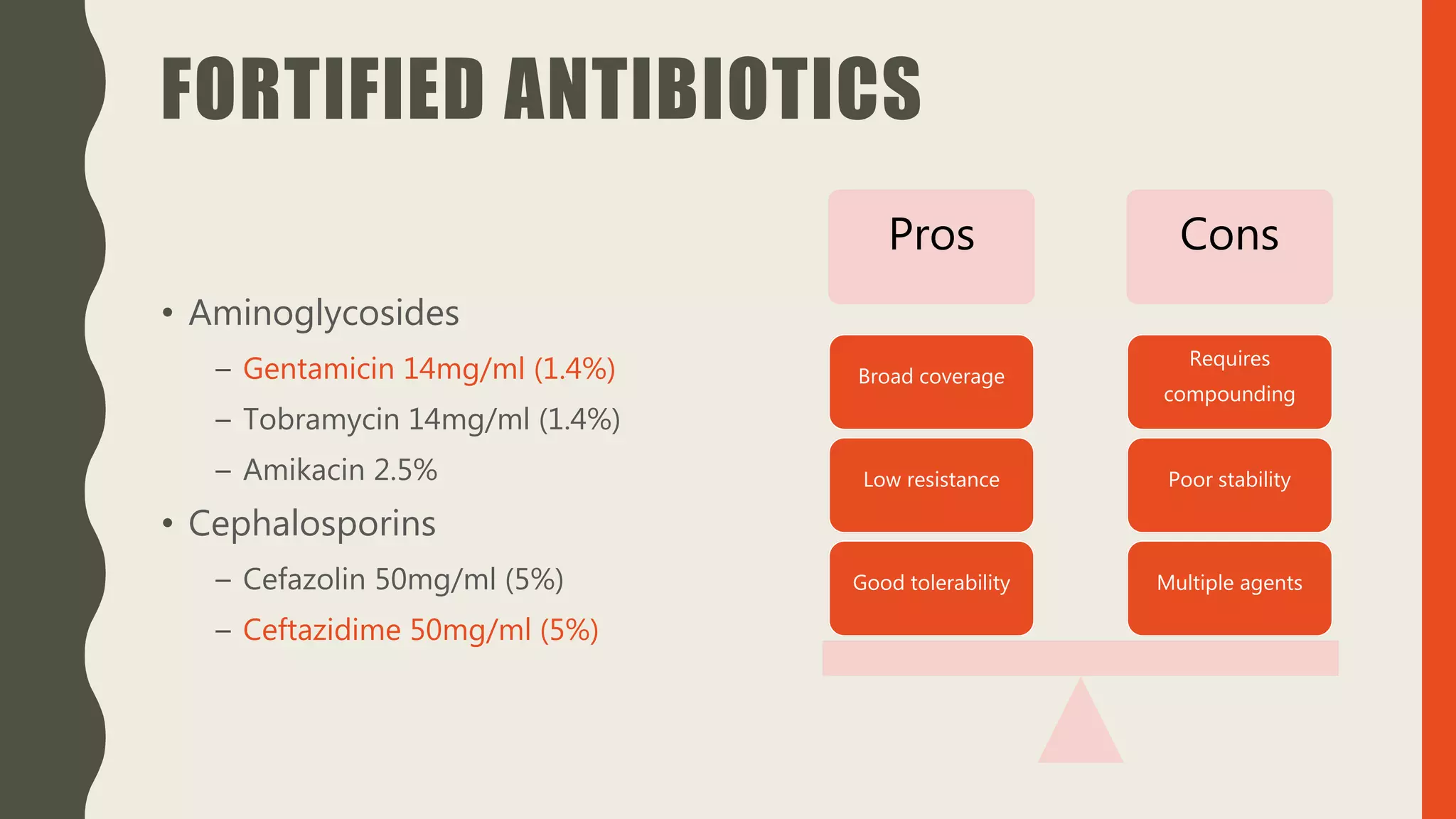
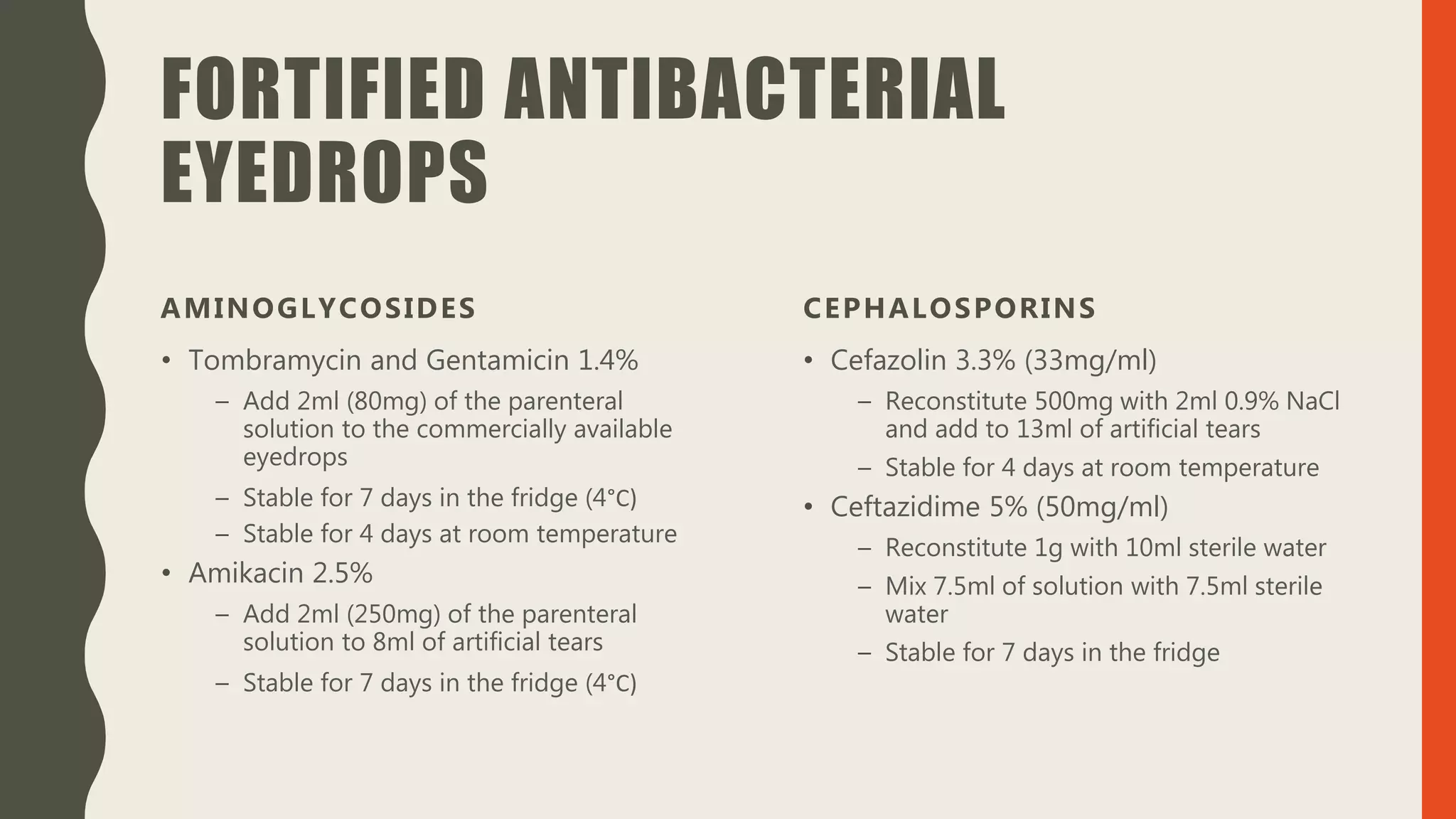
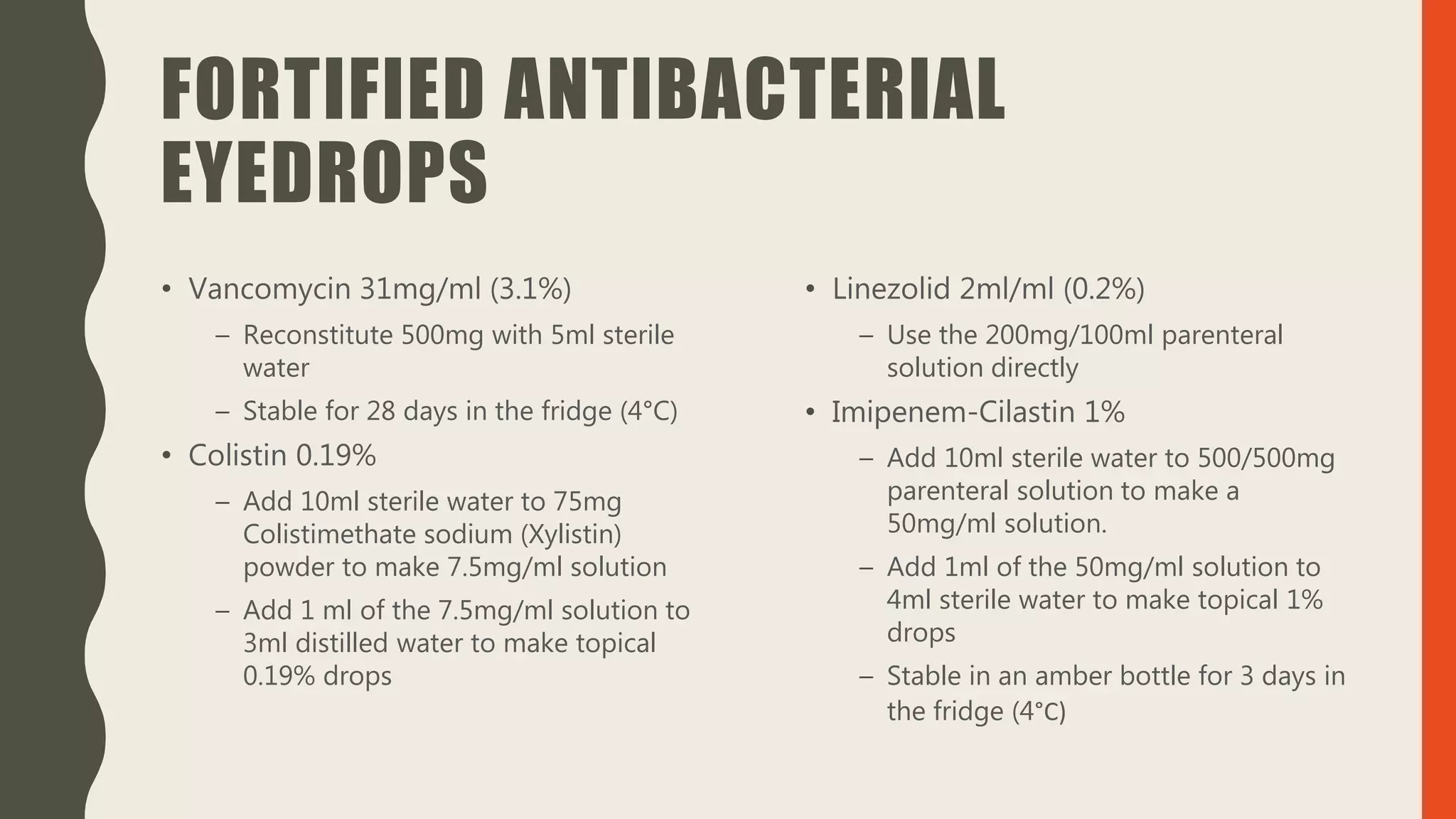
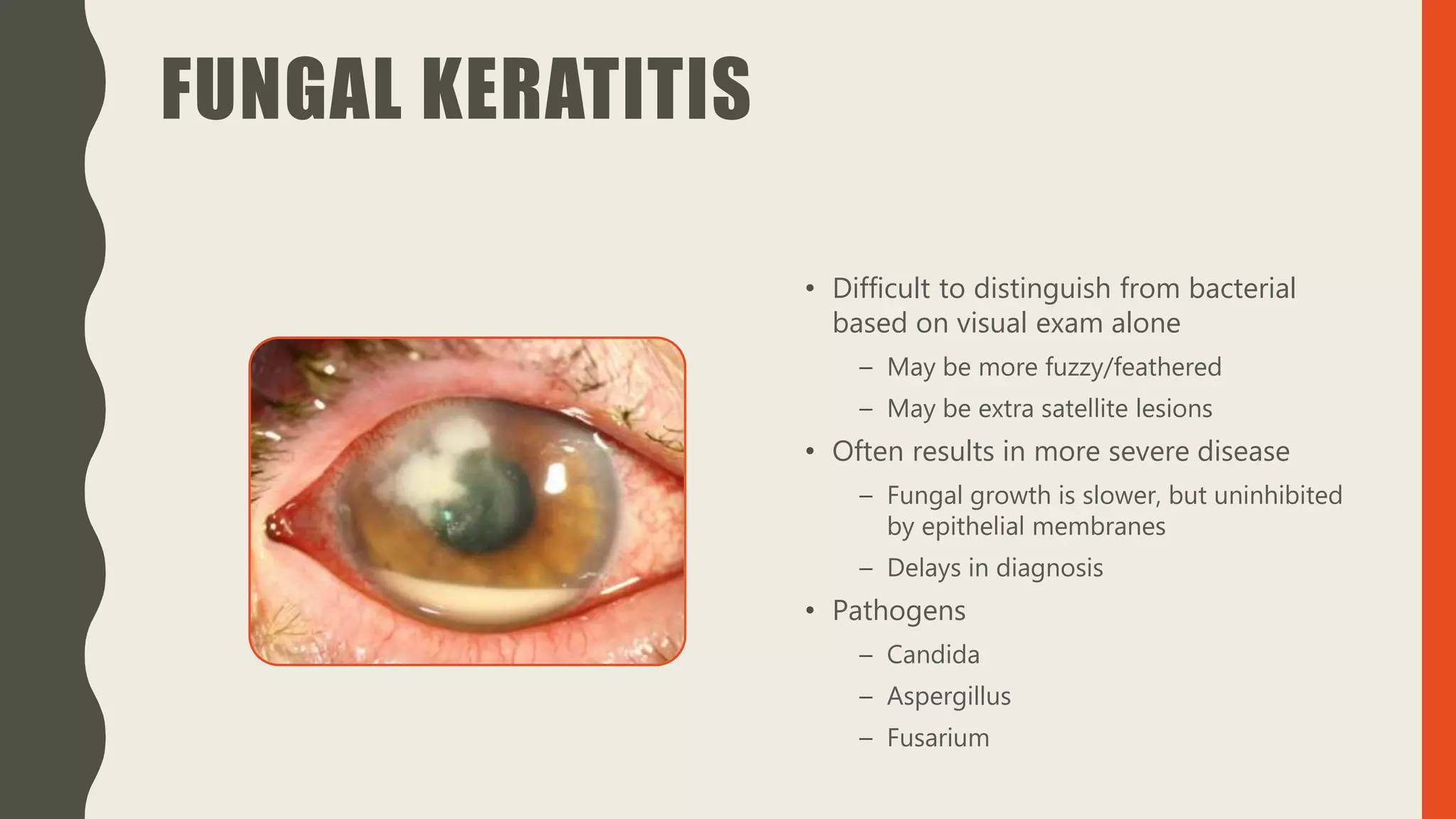
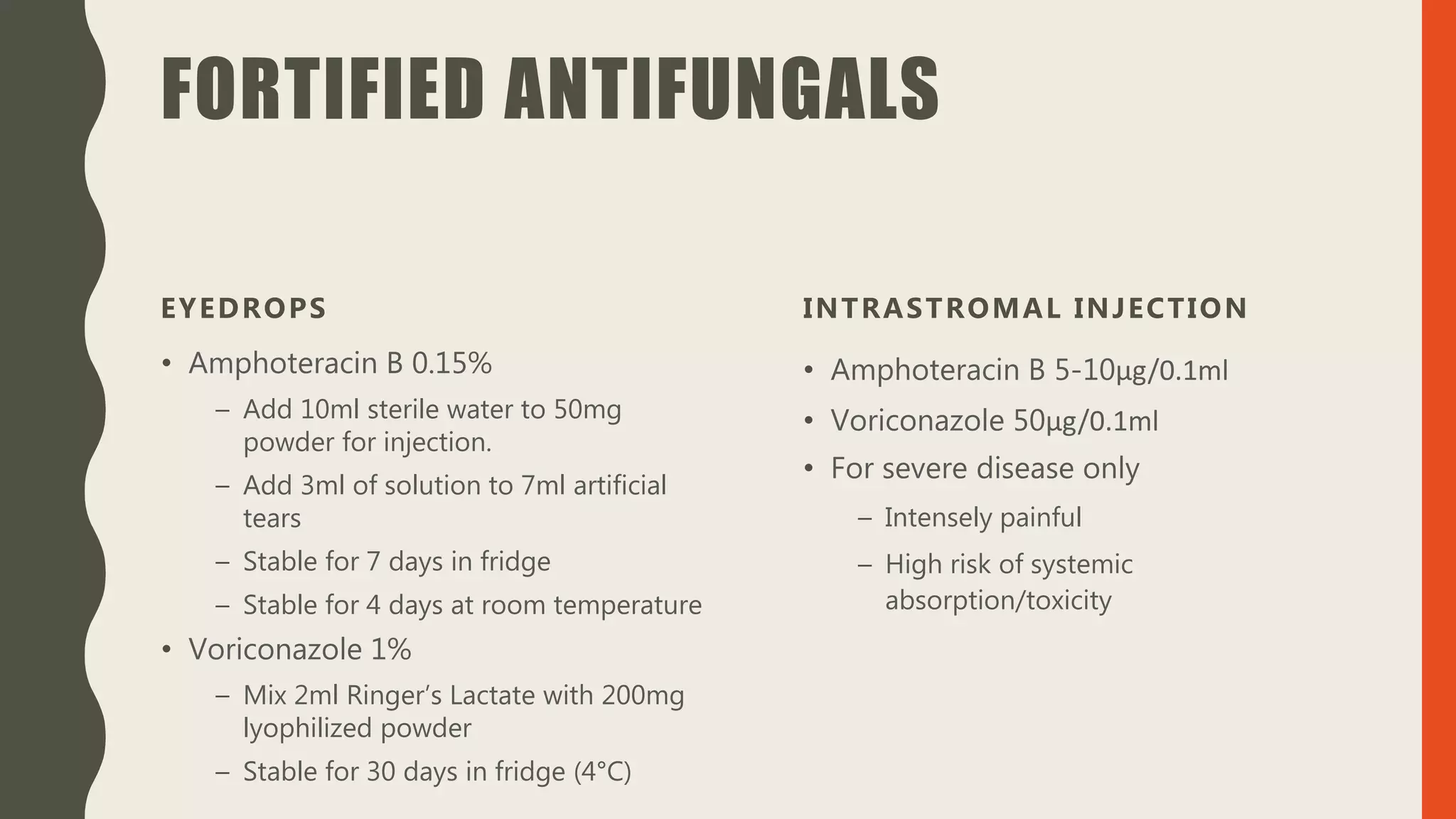
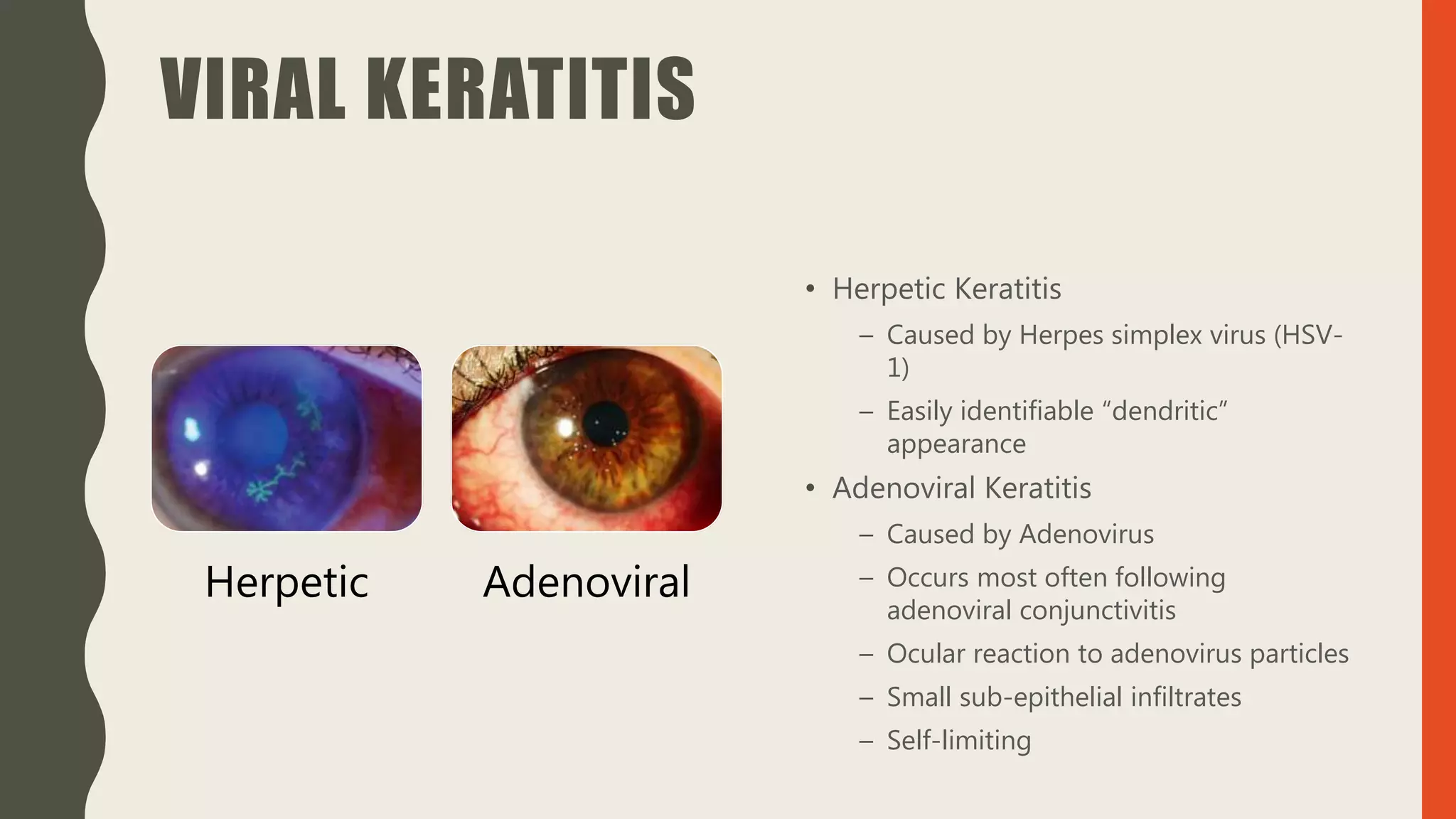
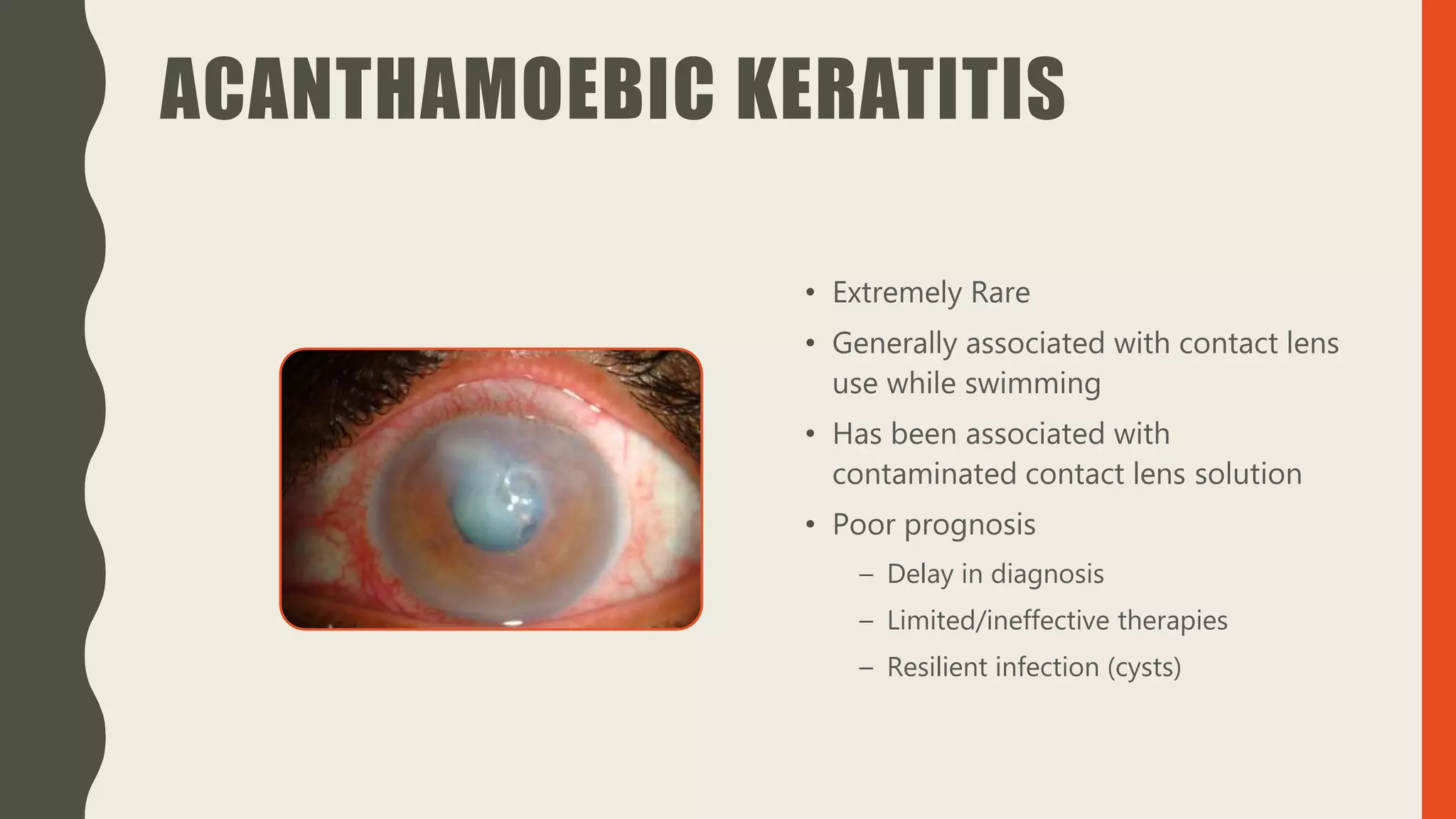
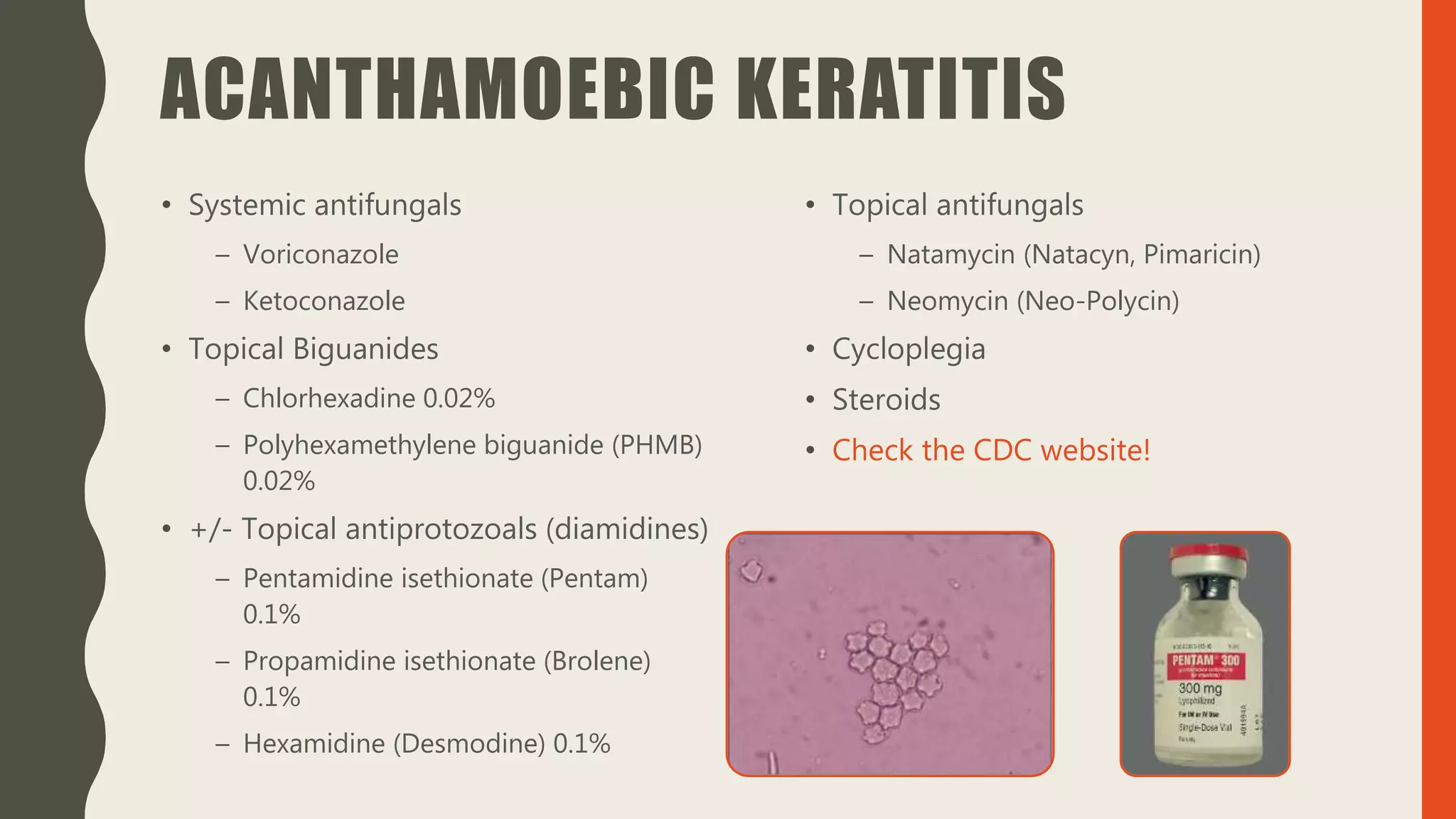
This document provides an overview of infectious keratitis. Keratitis is an infection of the cornea that is usually caused by contact lens use or trauma. Bacterial keratitis is the most common type and can progress rapidly, threatening vision. Diagnosis involves fluorescein staining and corneal scrapings for analysis. Treatment involves topical antibiotics like fluoroquinolones every hour along with cycloplegics for pain. Other types include fungal, viral like herpes simplex, and rare parasitic infections like acanthamoeba. Early diagnosis and aggressive treatment are important to prevent vision loss and perforation of the cornea.