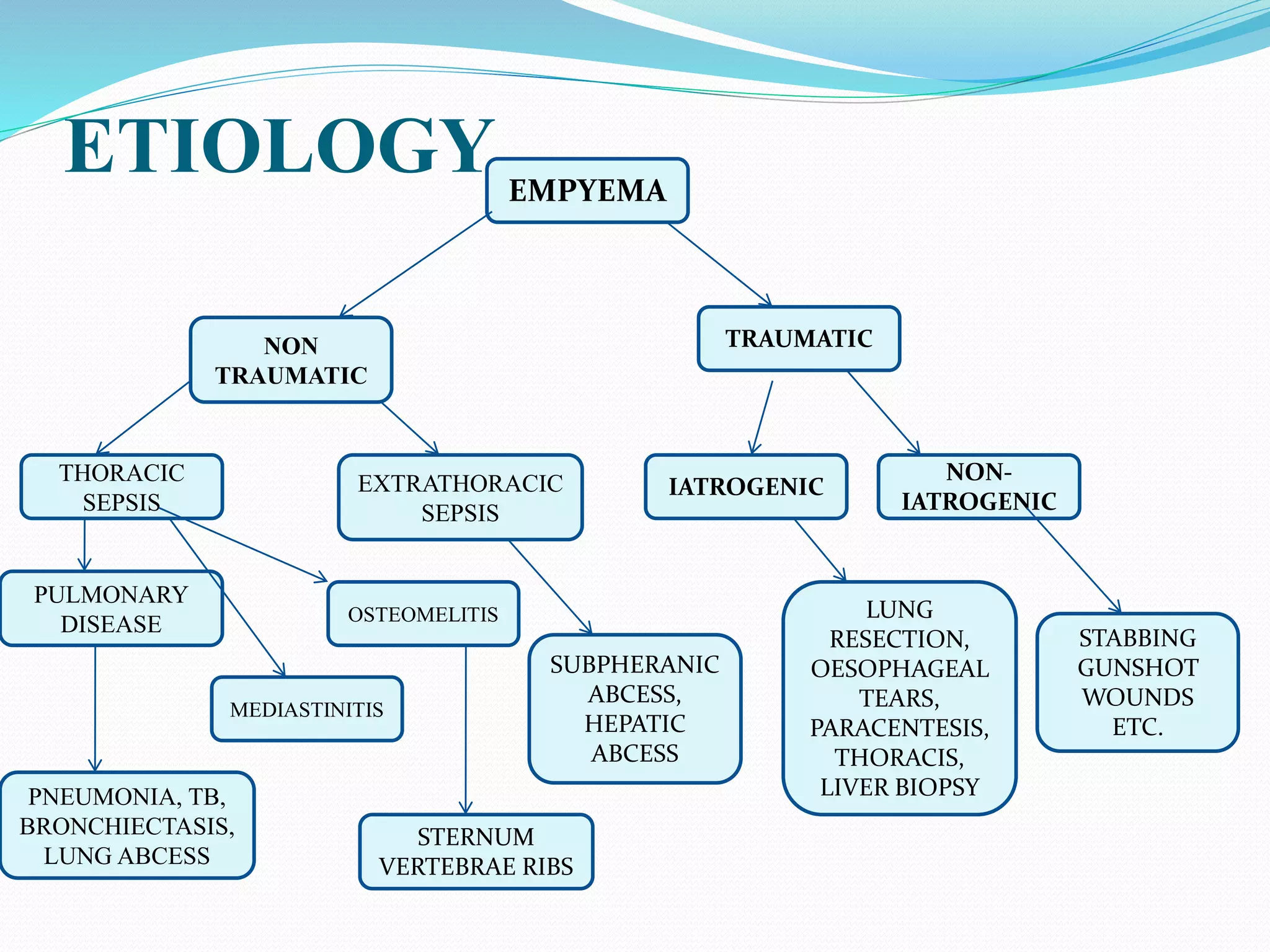
This document defines empyema as the accumulation of pus in the pleural cavity. It is most commonly caused by pneumonia or other lung infections. Key symptoms include fever, chest pain, and cough. Diagnosis involves chest x-ray and thoracentesis. Treatment involves antibiotics, chest tube placement to drain pus, and sometimes fibrinolytics or surgery. Goals are to treat the infection, drain the pleural space, and allow lung re-expansion to prevent chronic issues. Physiotherapy after treatment is important for full recovery.