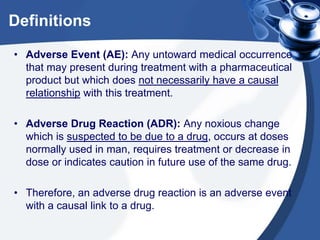
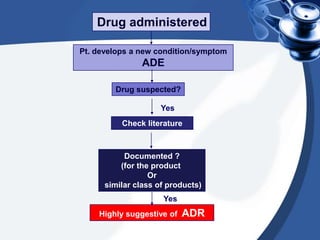
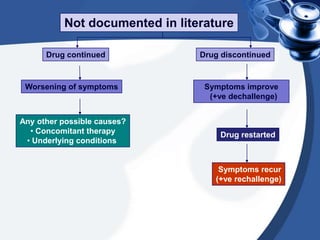
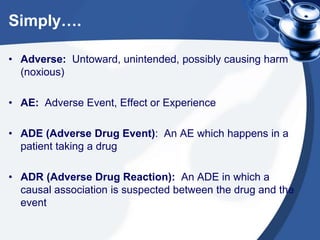
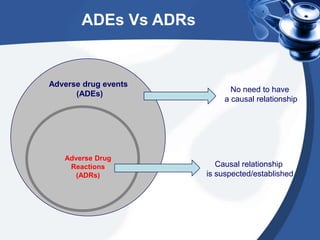
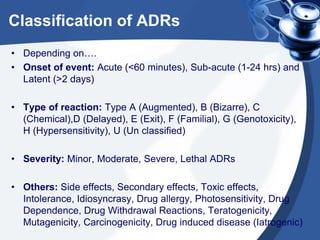
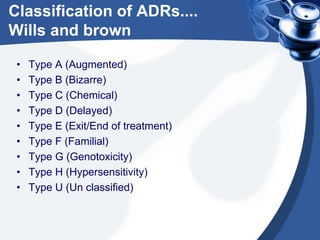
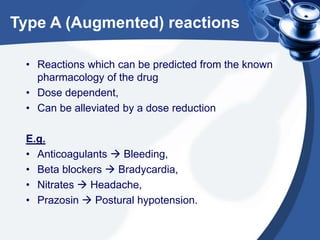
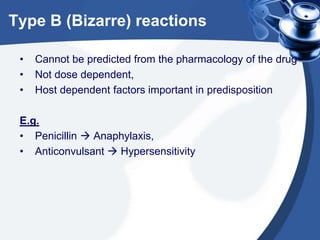
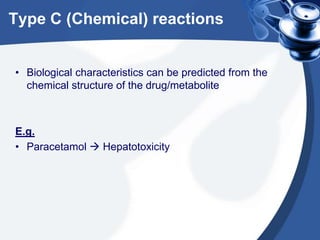
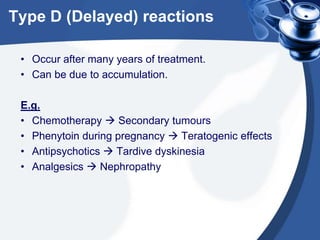
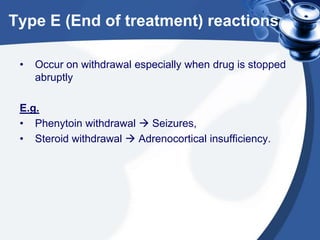
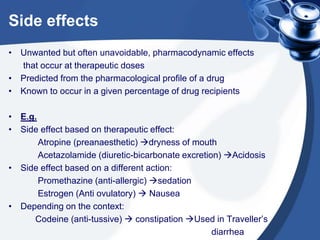
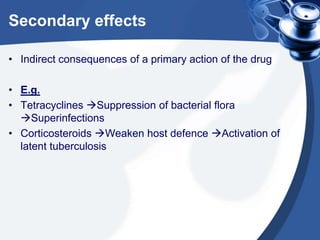
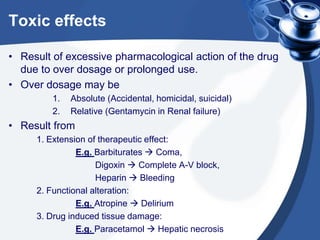
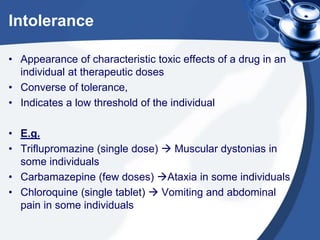
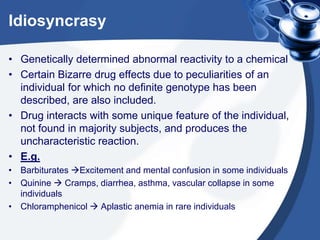
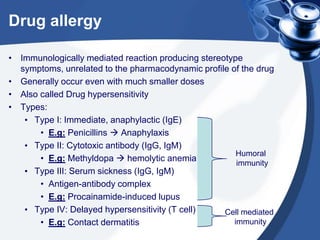
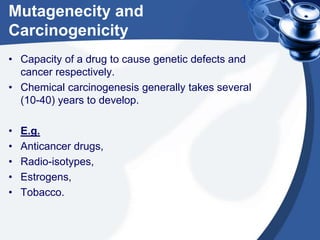
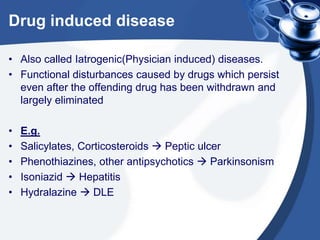
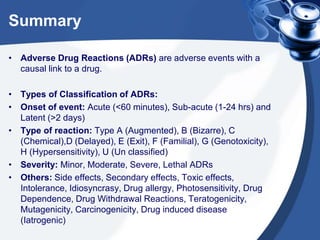
This document provides definitions and classifications of adverse drug reactions (ADRs). It defines key terms like adverse event, adverse drug reaction, and adverse drug event. It then discusses various classification schemes for ADRs based on factors like onset, type of reaction, severity, and more. Different types of ADRs are explained like Type A, B, C reactions as well as side effects, drug dependence, withdrawal reactions and more, along with examples. Overall, the document provides a comprehensive overview of definitions and classifications related to ADRs.