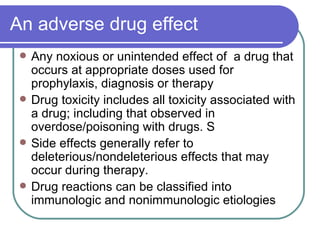
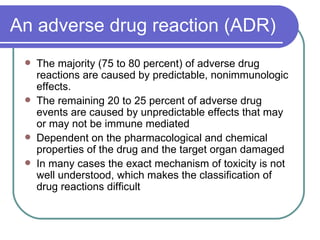
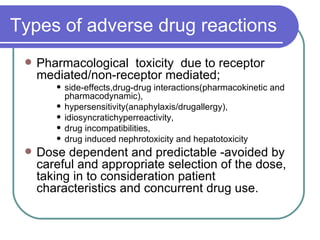
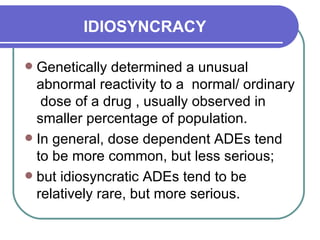
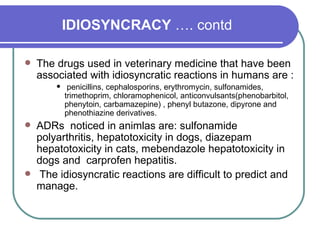
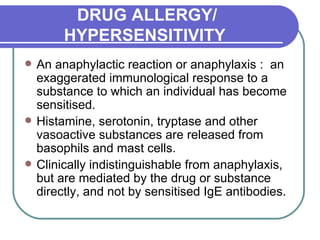
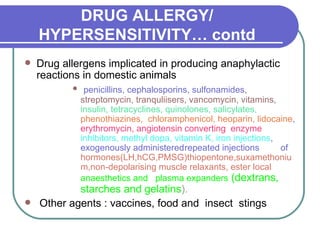
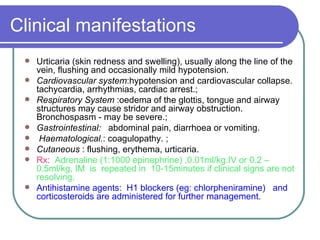
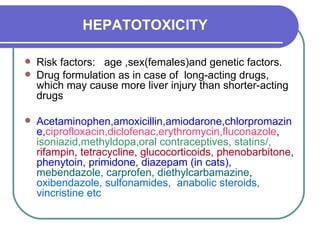
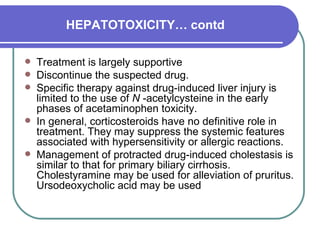
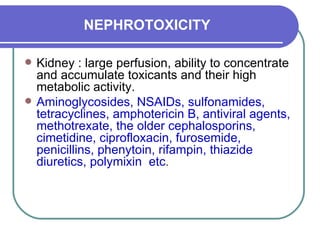
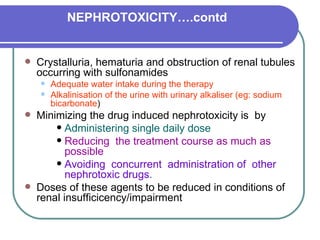
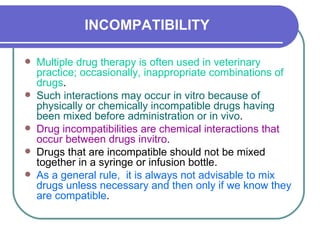
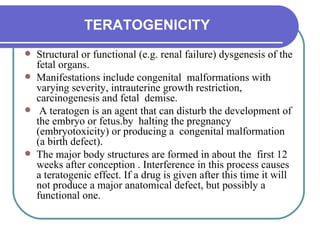
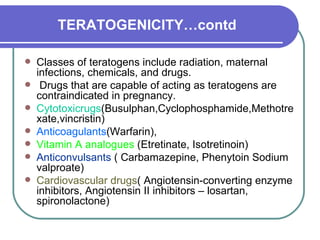
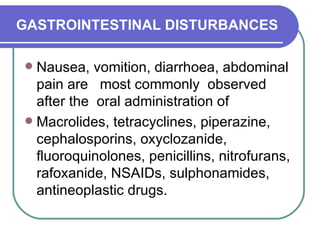
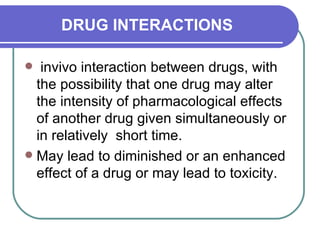
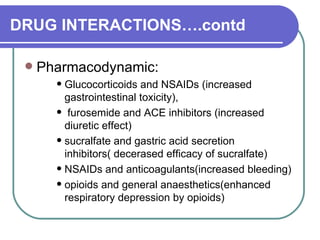
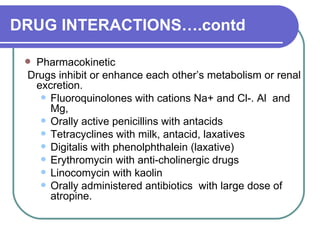
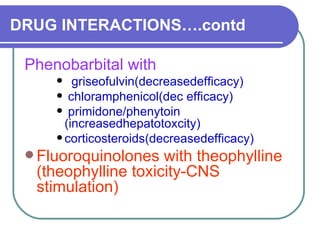
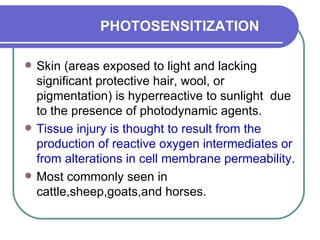
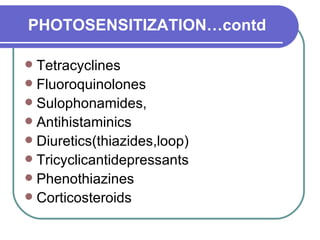
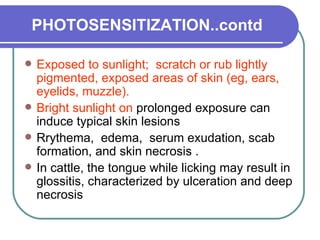
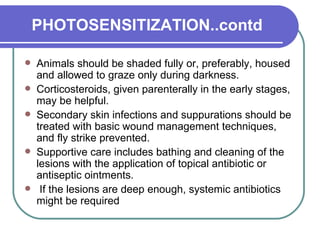
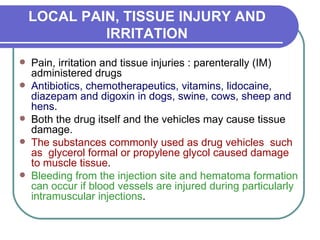
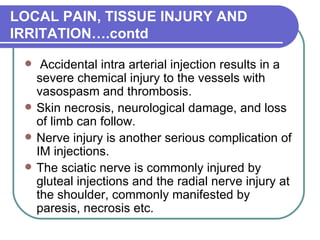
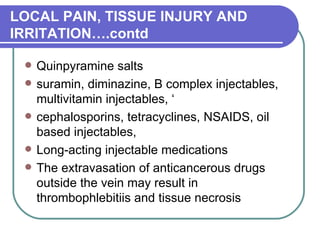
This document summarizes various types of adverse drug effects including pharmacological toxicity, idiosyncratic reactions, drug allergies, hepatotoxicity, nephrotoxicity, drug interactions, photosensitization, and local pain and tissue injuries. It discusses the mechanisms, clinical signs, and management of these adverse effects for different drug classes in veterinary medicine. Risk factors, treatment approaches, and ways to minimize adverse reactions are also covered.