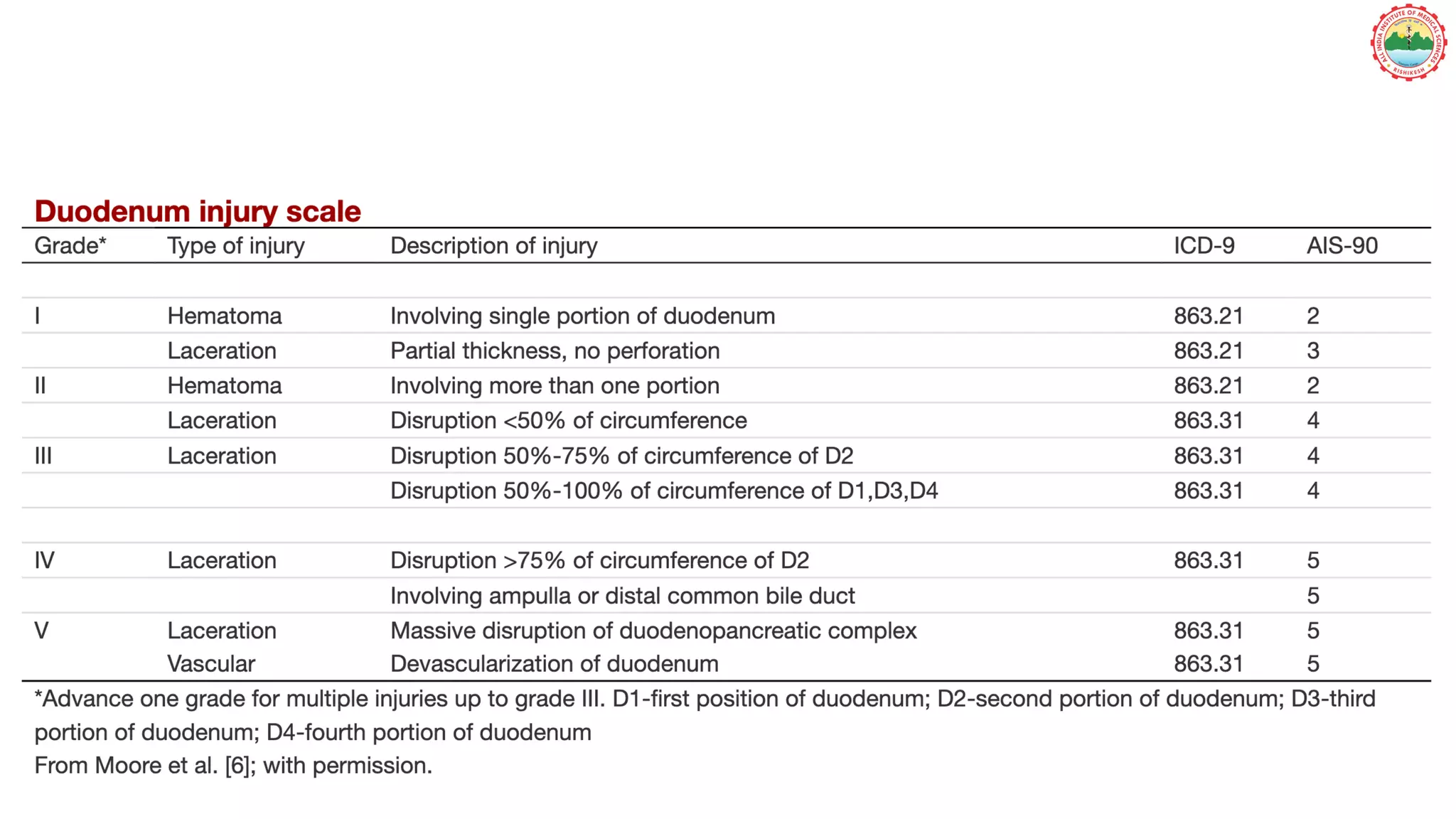
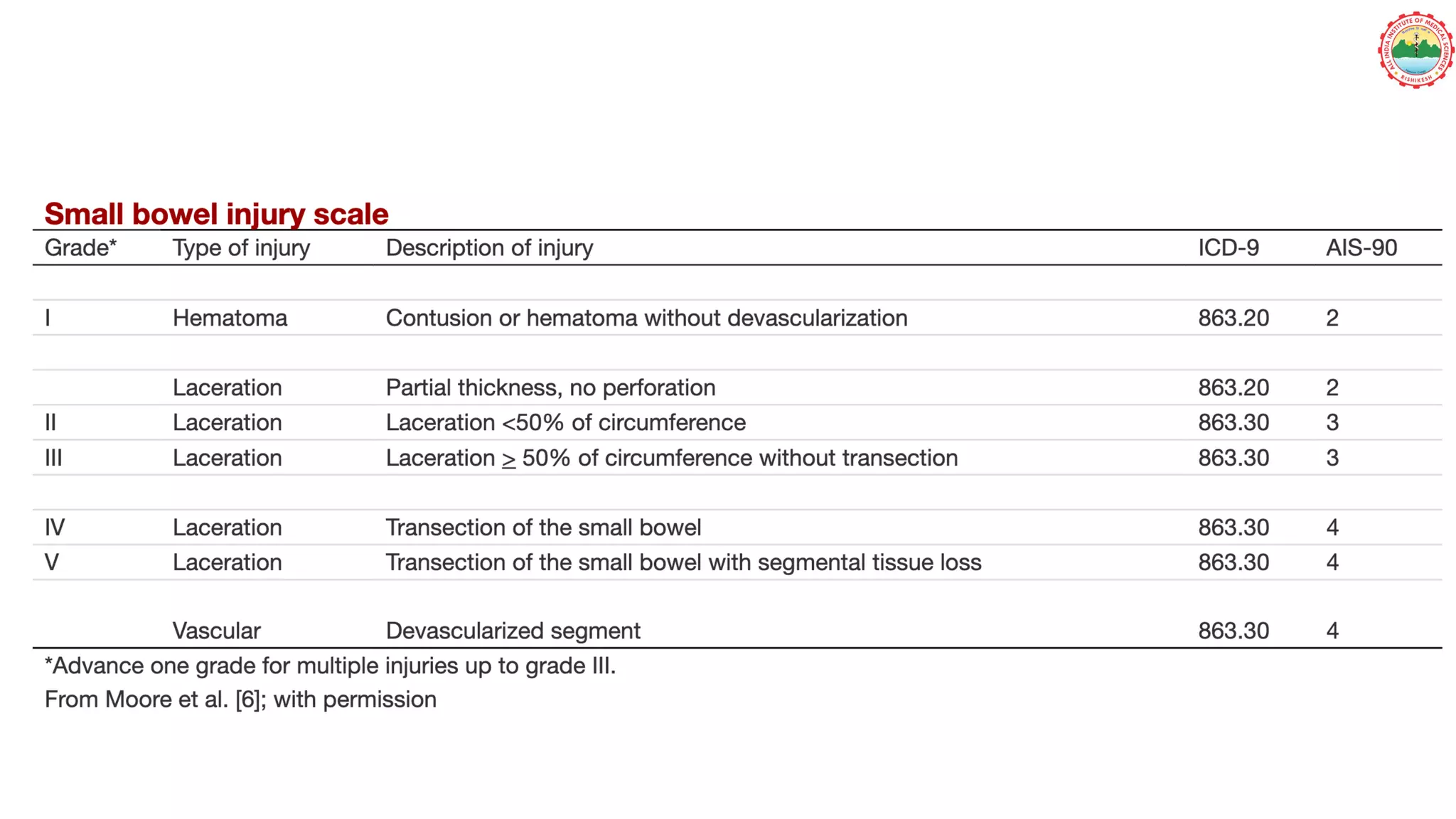
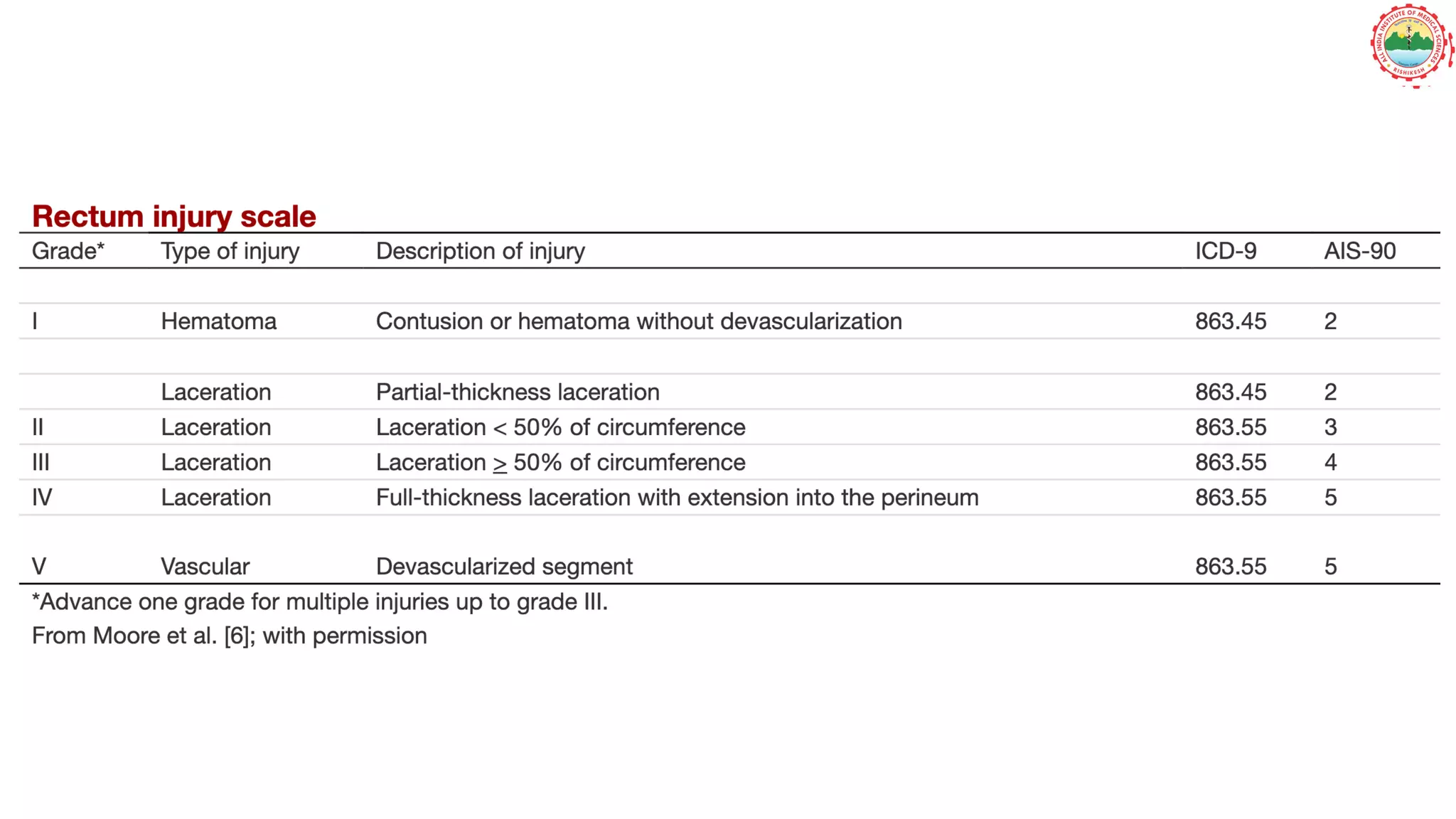
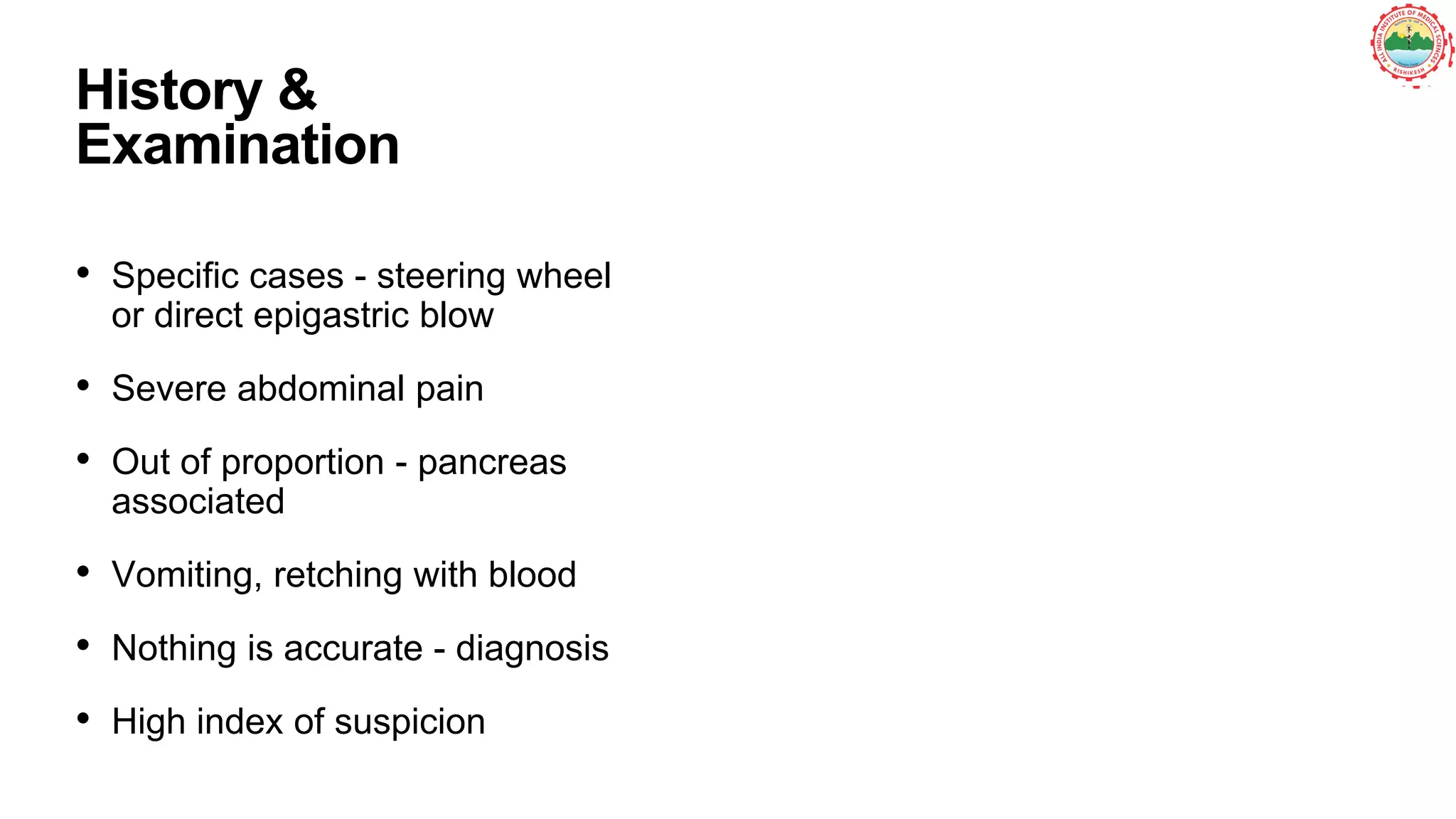
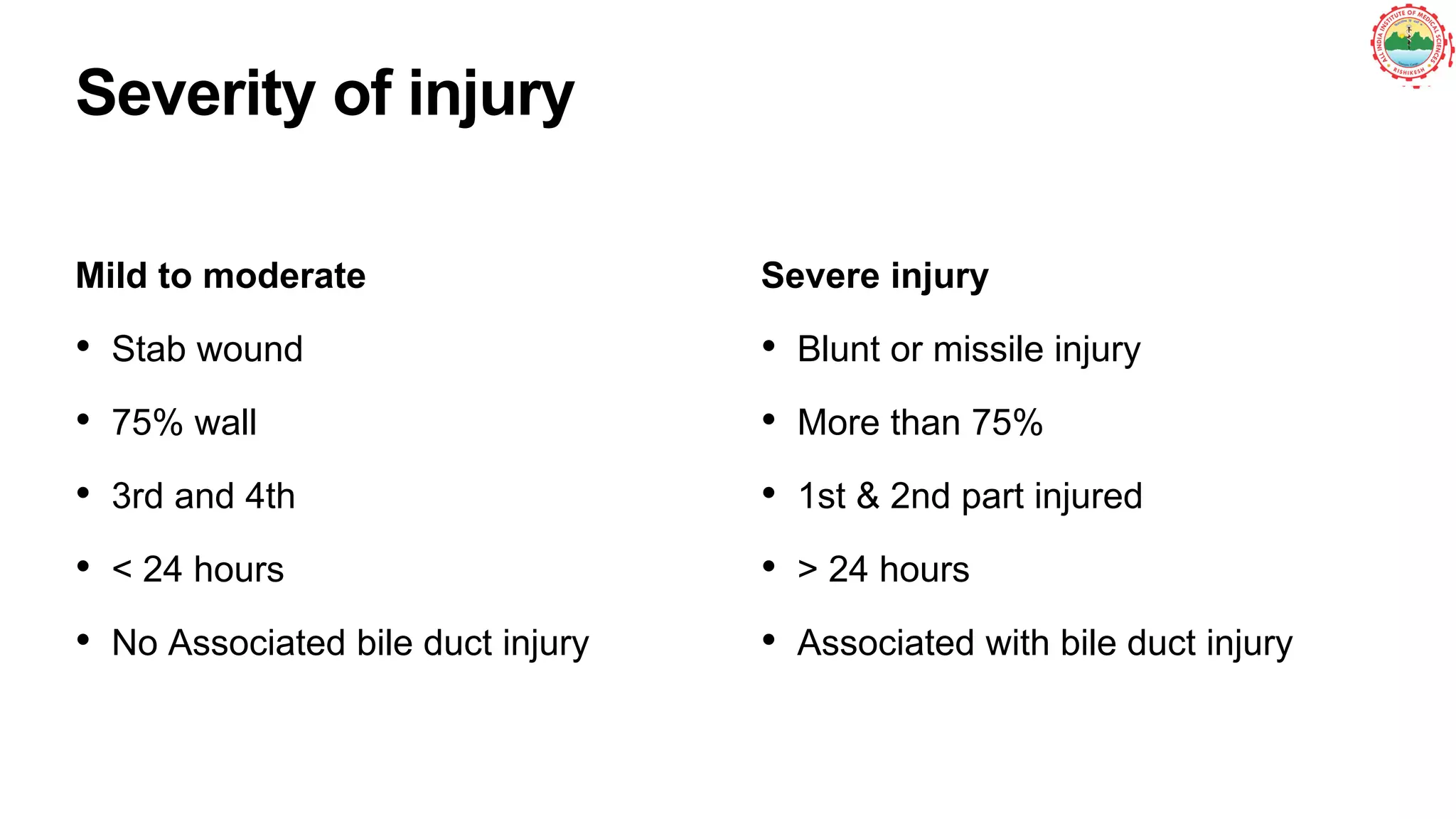
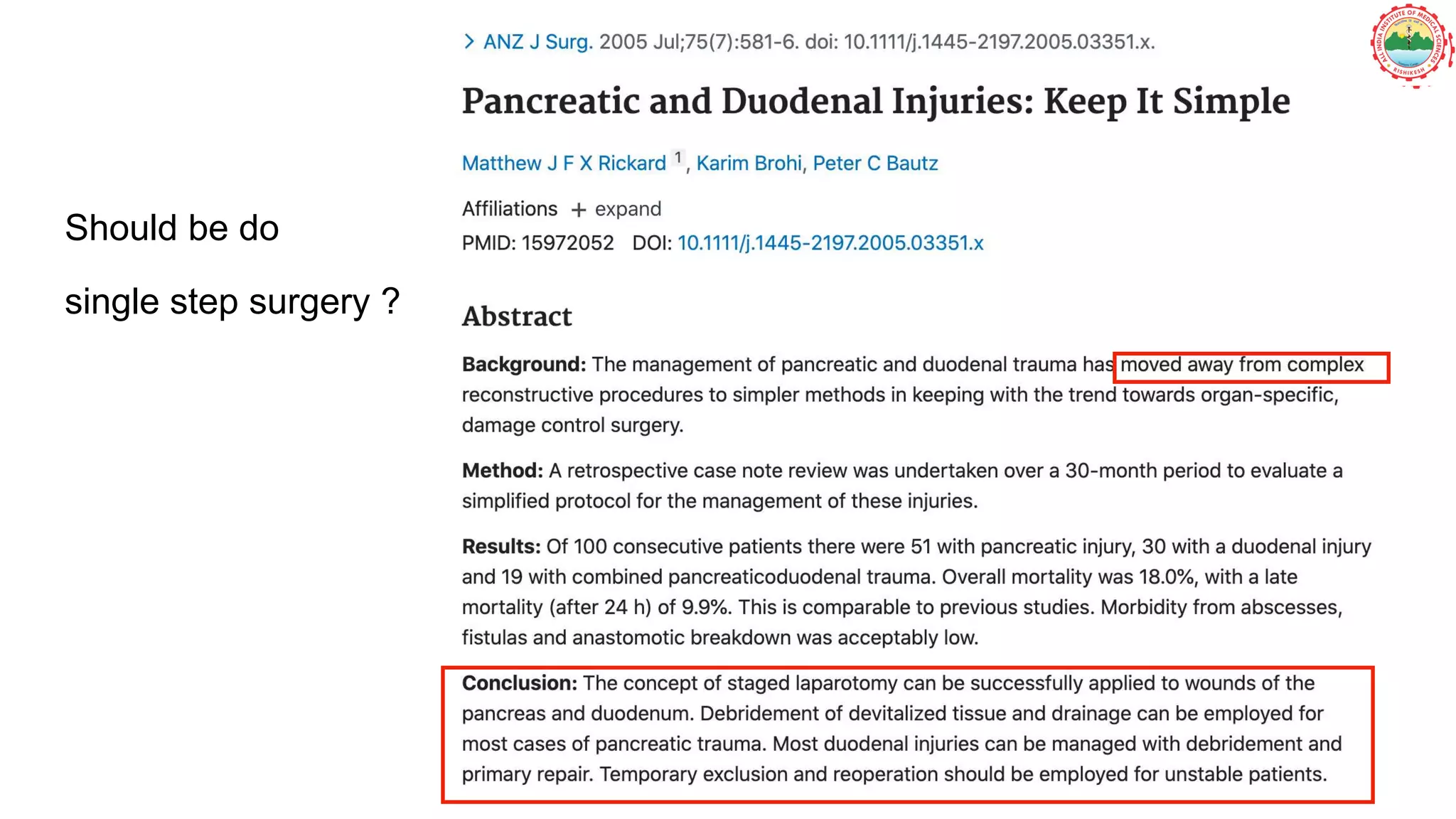
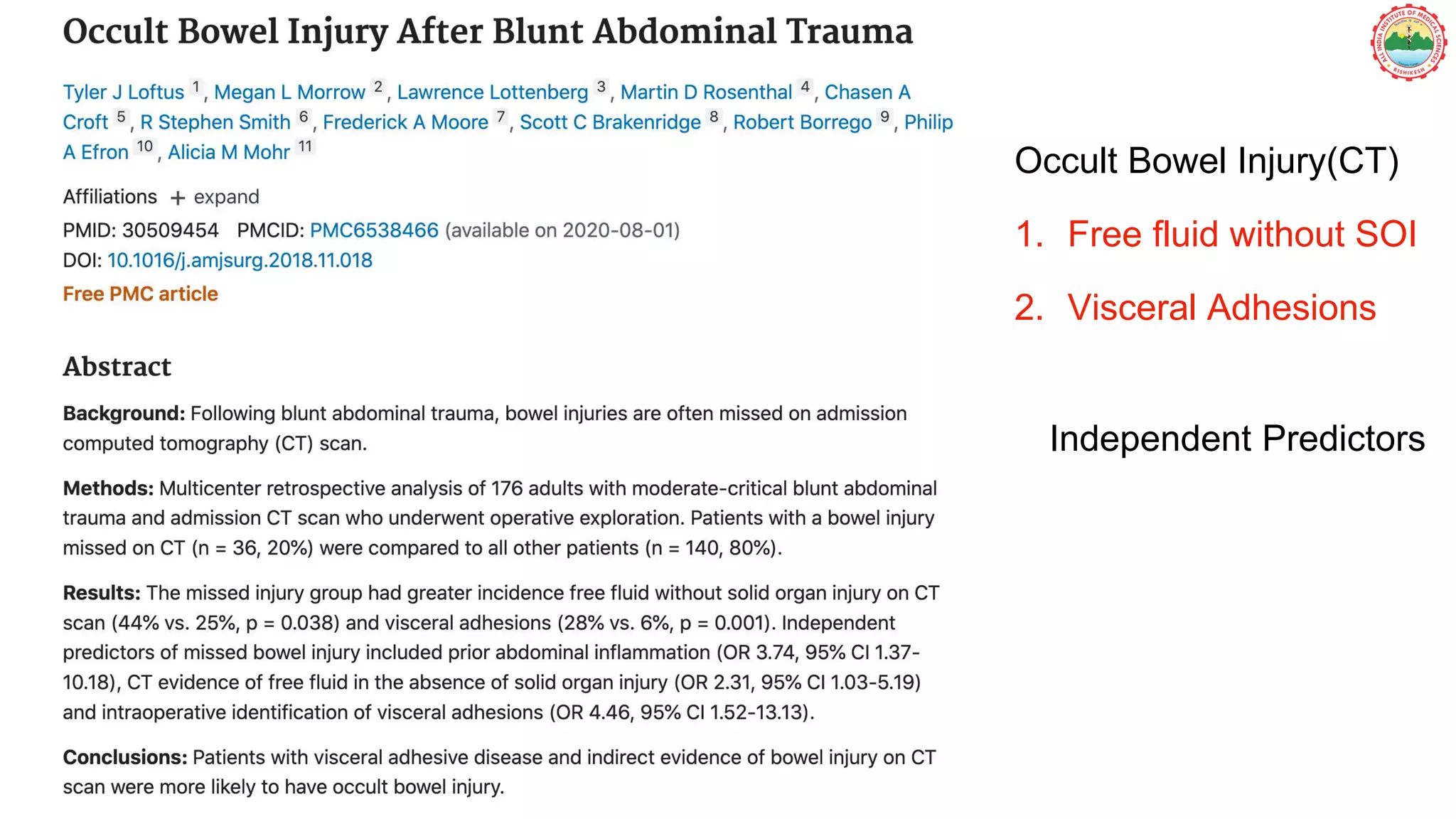
This document discusses the grading and management of bowel injuries, particularly focusing on traumatic bowel injuries caused by blunt or penetrating trauma. It underscores the importance of timely diagnosis using various imaging techniques and the need for careful surgical intervention depending on patient stability. The document also highlights the challenges in identifying mesenteric injuries and the implications of delay on patient outcomes.