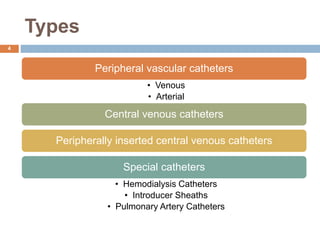
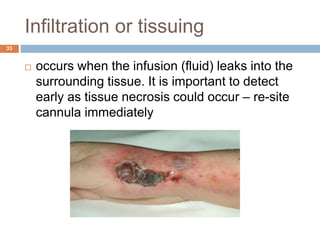
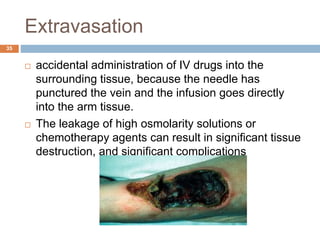
An intracatheter is a plastic tube inserted into a blood vessel. They were first used in 1929 when a surgeon inserted a catheter into his own heart. There are several types including peripheral, central venous, and pulmonary artery catheters. They are made of biocompatible polymers like polyurethane and silicone. Size is determined by gauge or French units, with smaller gauges and French sizes indicating thinner catheters. Complications can include infection, infiltration of fluids, thrombosis, and air embolism. Larger central venous catheters are often needed for critically ill patients requiring multiple therapies.