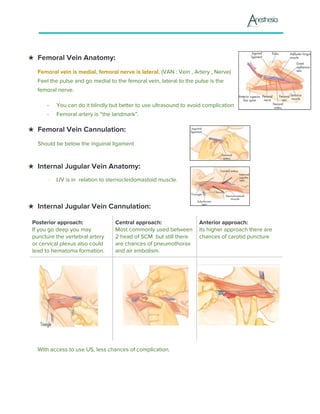
This document provides information on vascular access, including peripheral and central venous access. It discusses indications for different types of catheters, anatomical considerations, universal precautions, procedures for peripheral IV insertion, and potential complications. Central venous access involves greater risks but can be necessary for certain indications like administration of irritant fluids or long-term access. Proper technique and monitoring are important to prevent complications such as infiltration, infection, and air embolism.