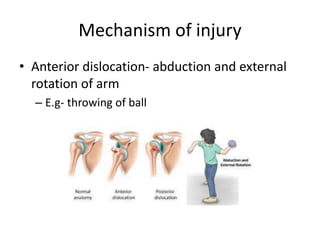
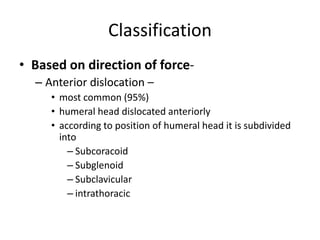
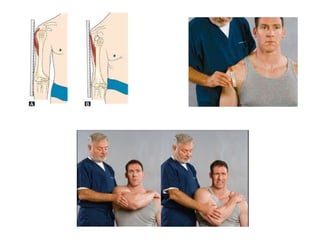
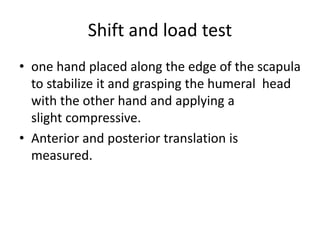
This document discusses anterior recurrent shoulder dislocation. It begins with an introduction stating that the shoulder is one of the most unstable joints and anterior dislocation is the most common type, affecting around 2% of the population. It then covers the anatomy and stabilizing structures of the shoulder joint. It describes the mechanism of injury as anterior dislocation occurring during abduction and external rotation. Classification, risk factors, pathoanatomy, clinical features, investigations, and various surgical and non-surgical treatment options are discussed. Common procedures mentioned include Bankart repair, Laterjet procedure, and remplissage.