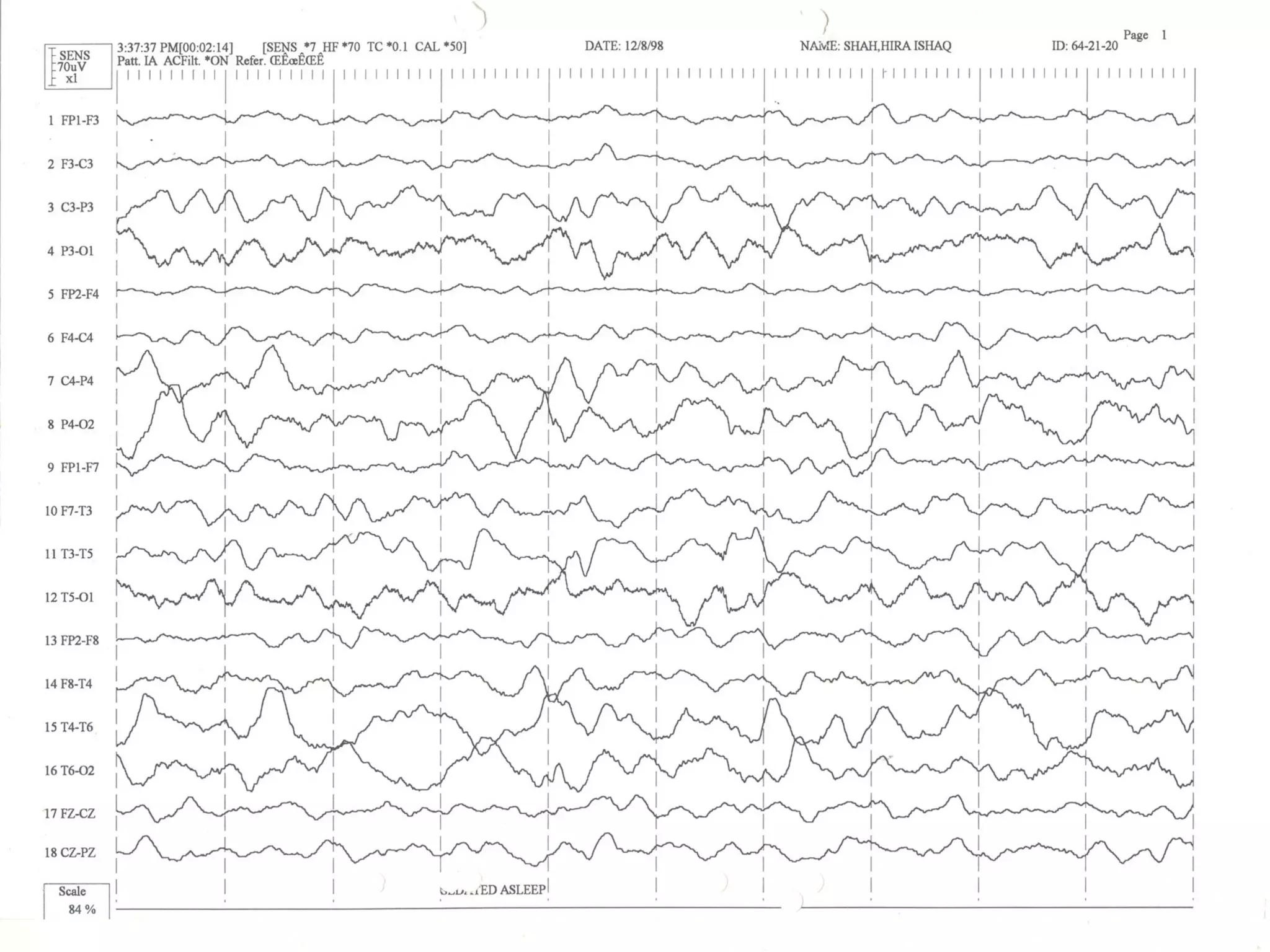
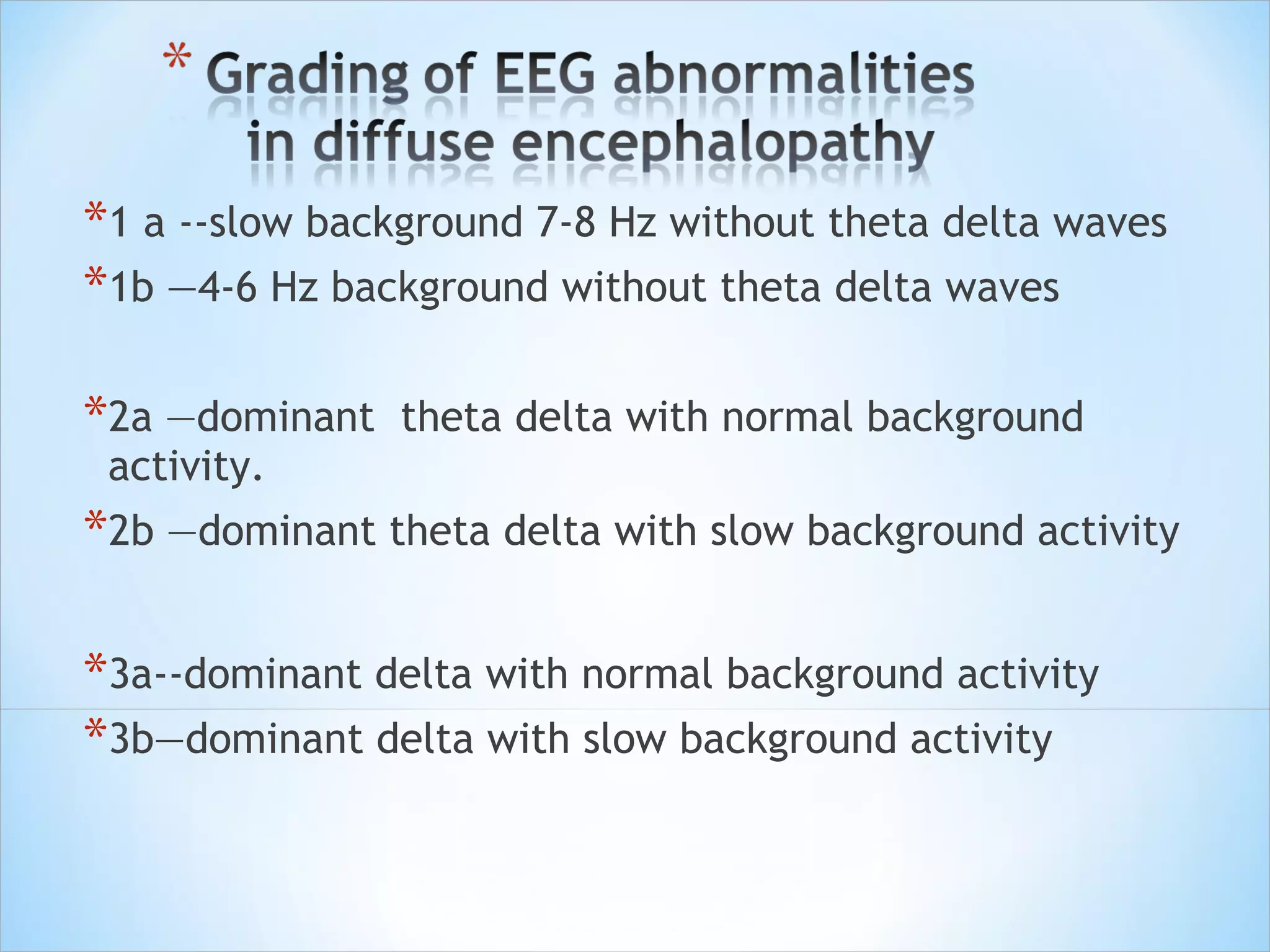
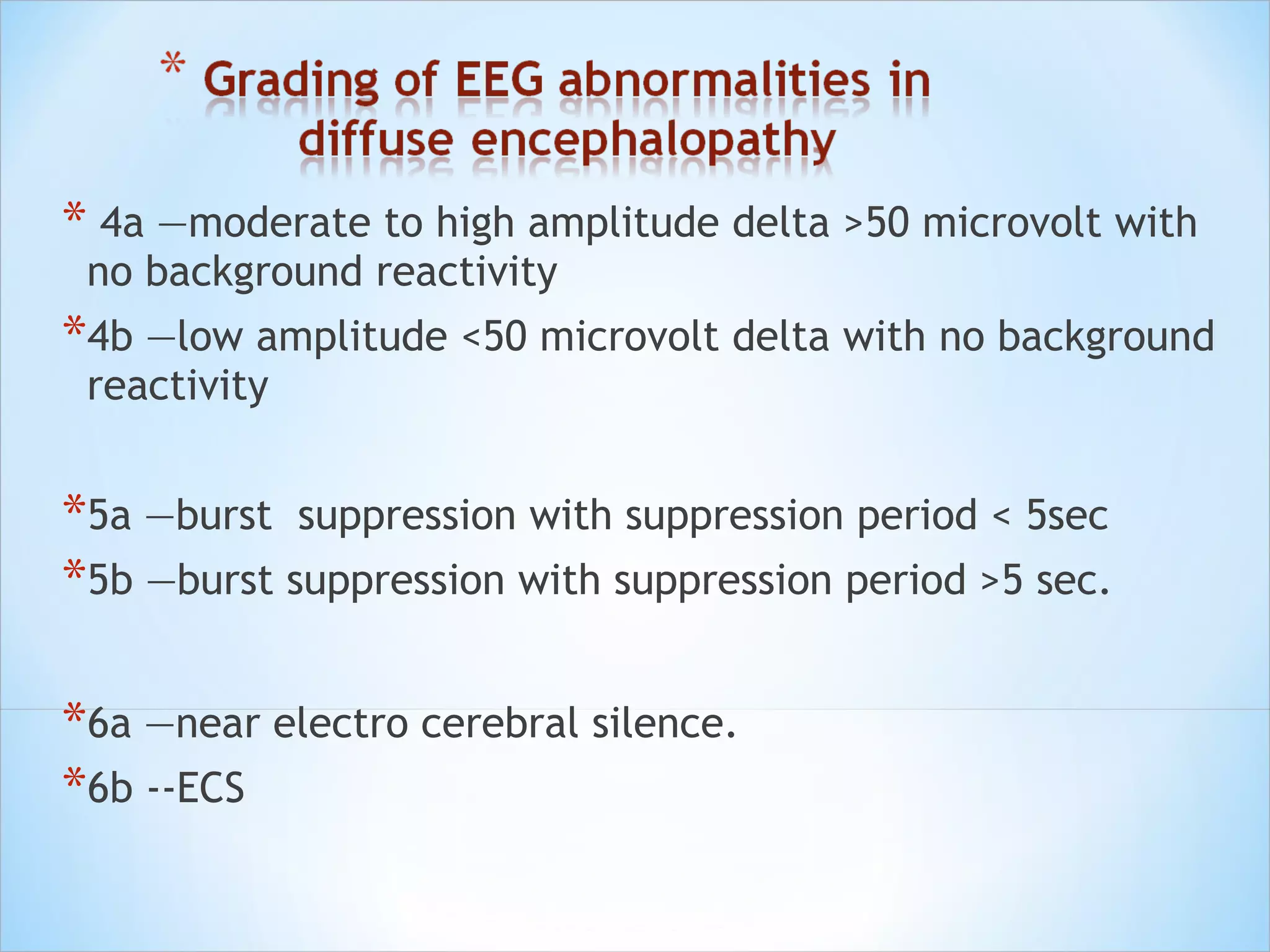
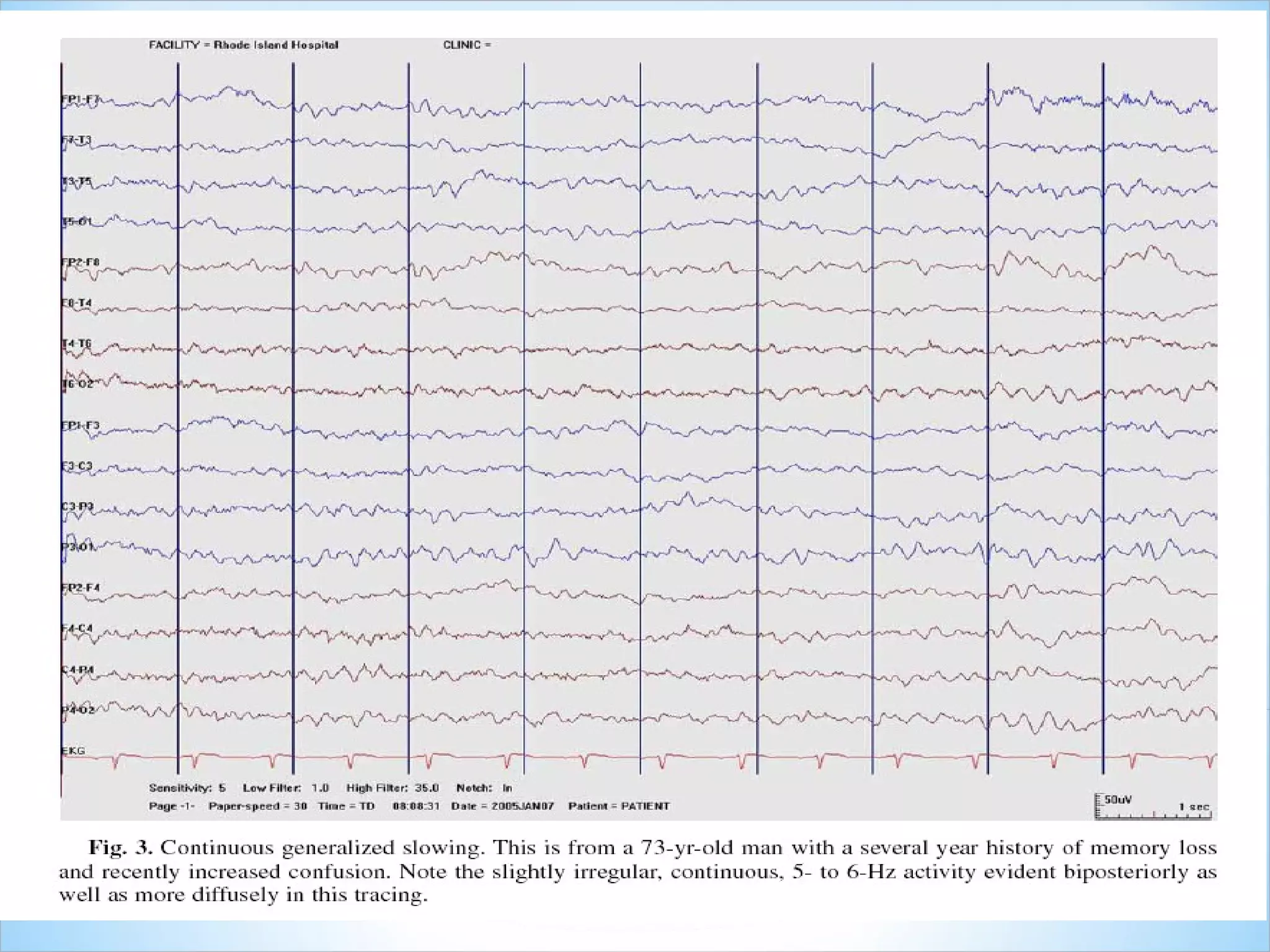
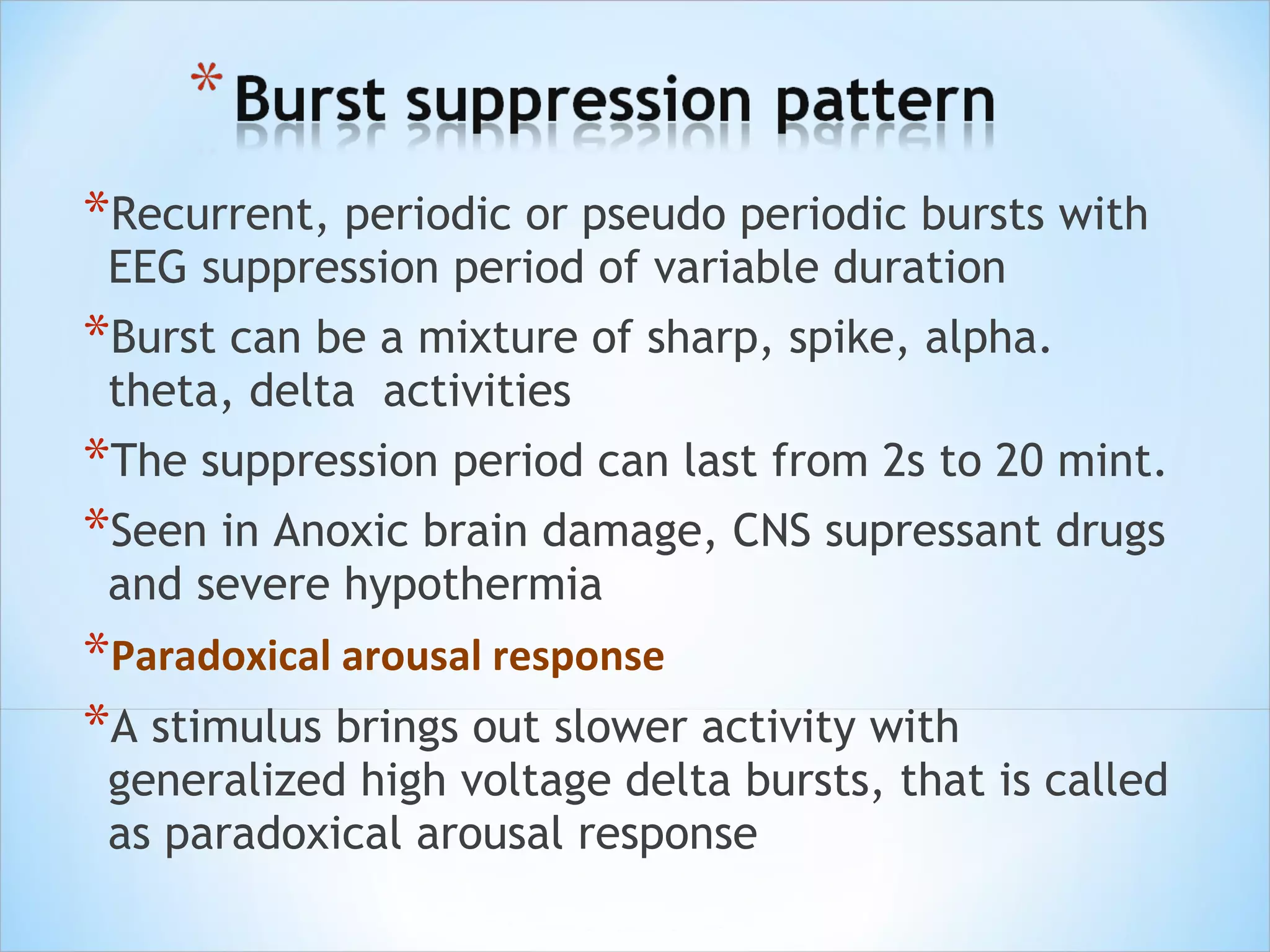
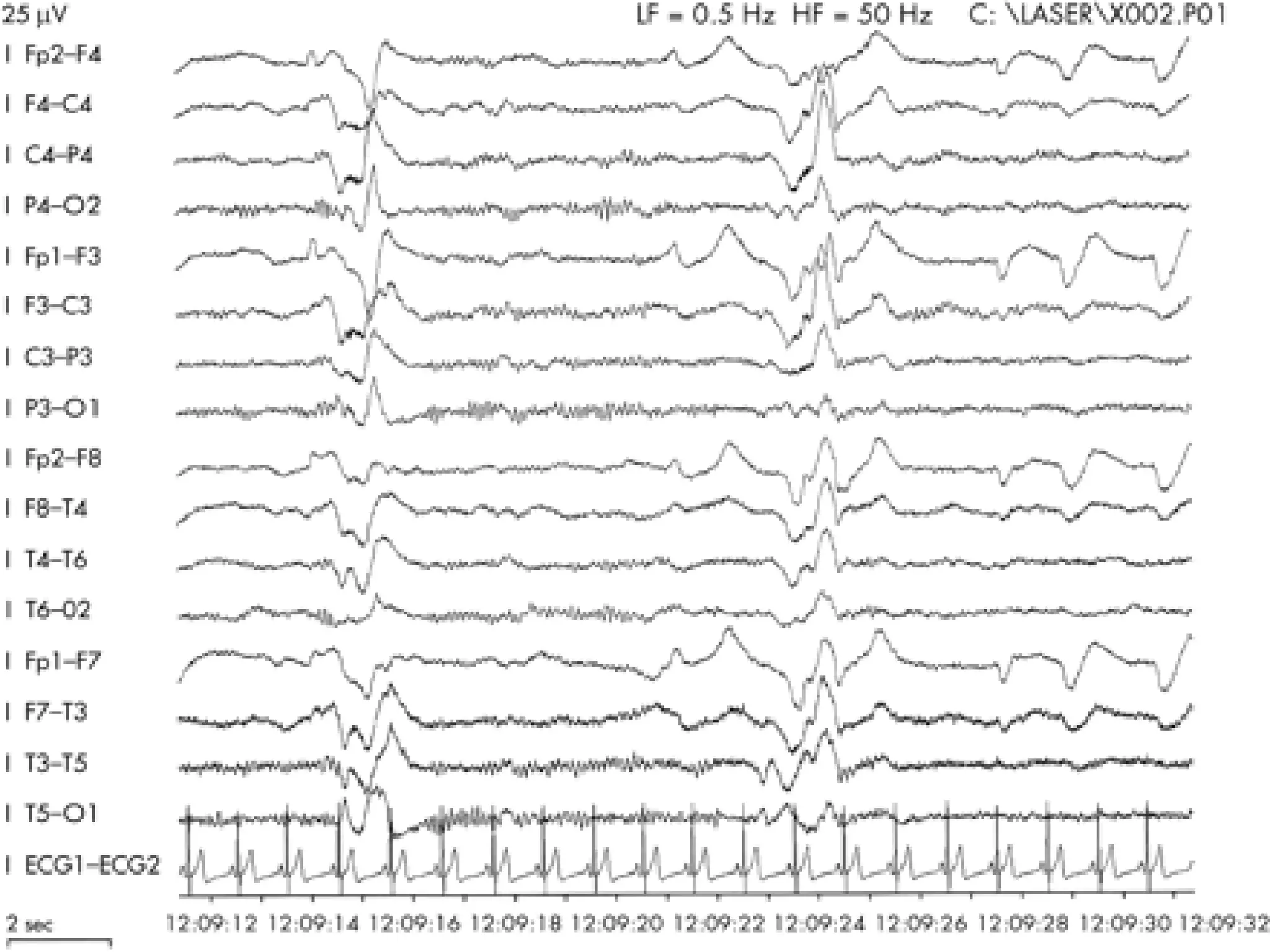
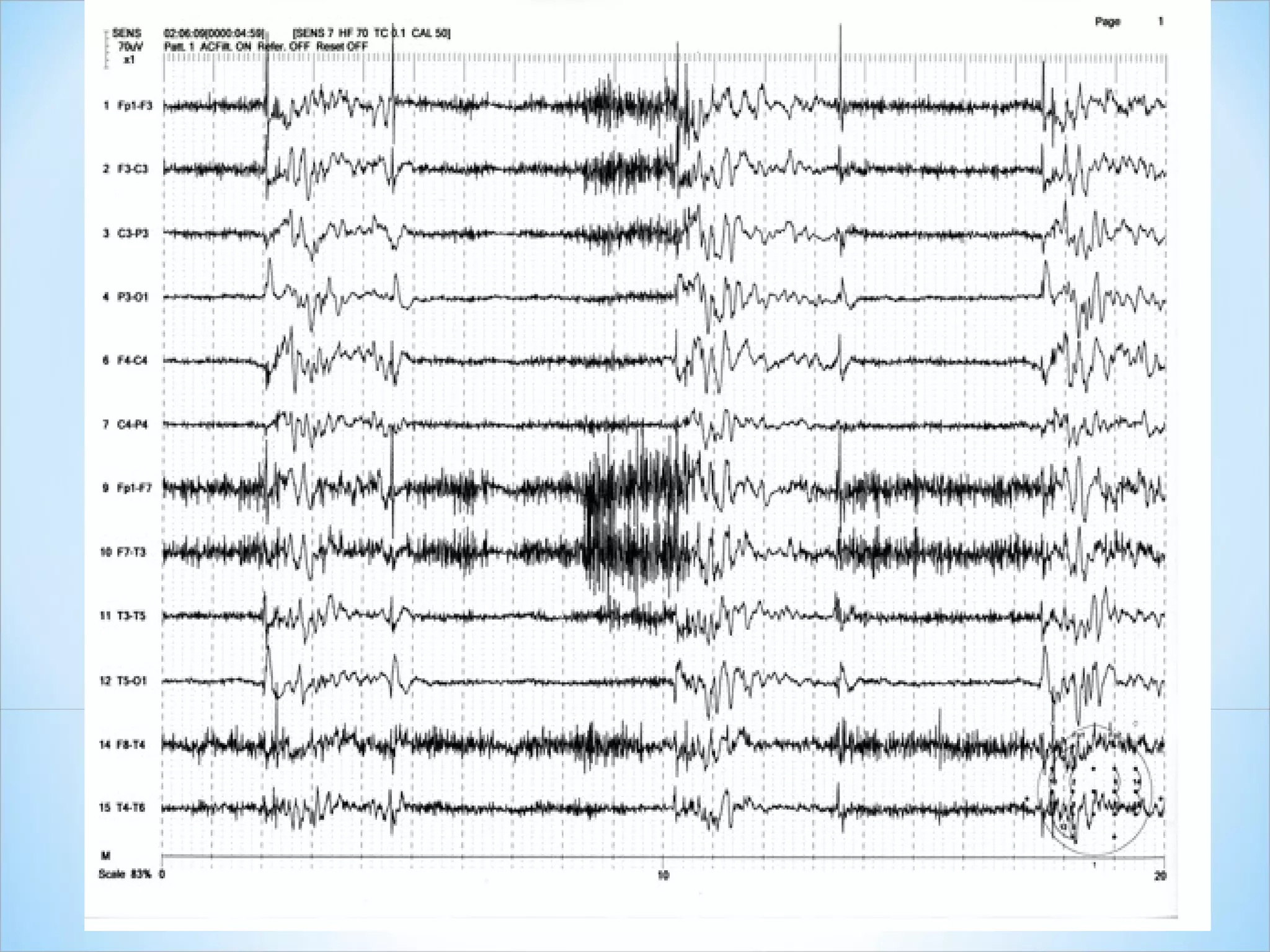
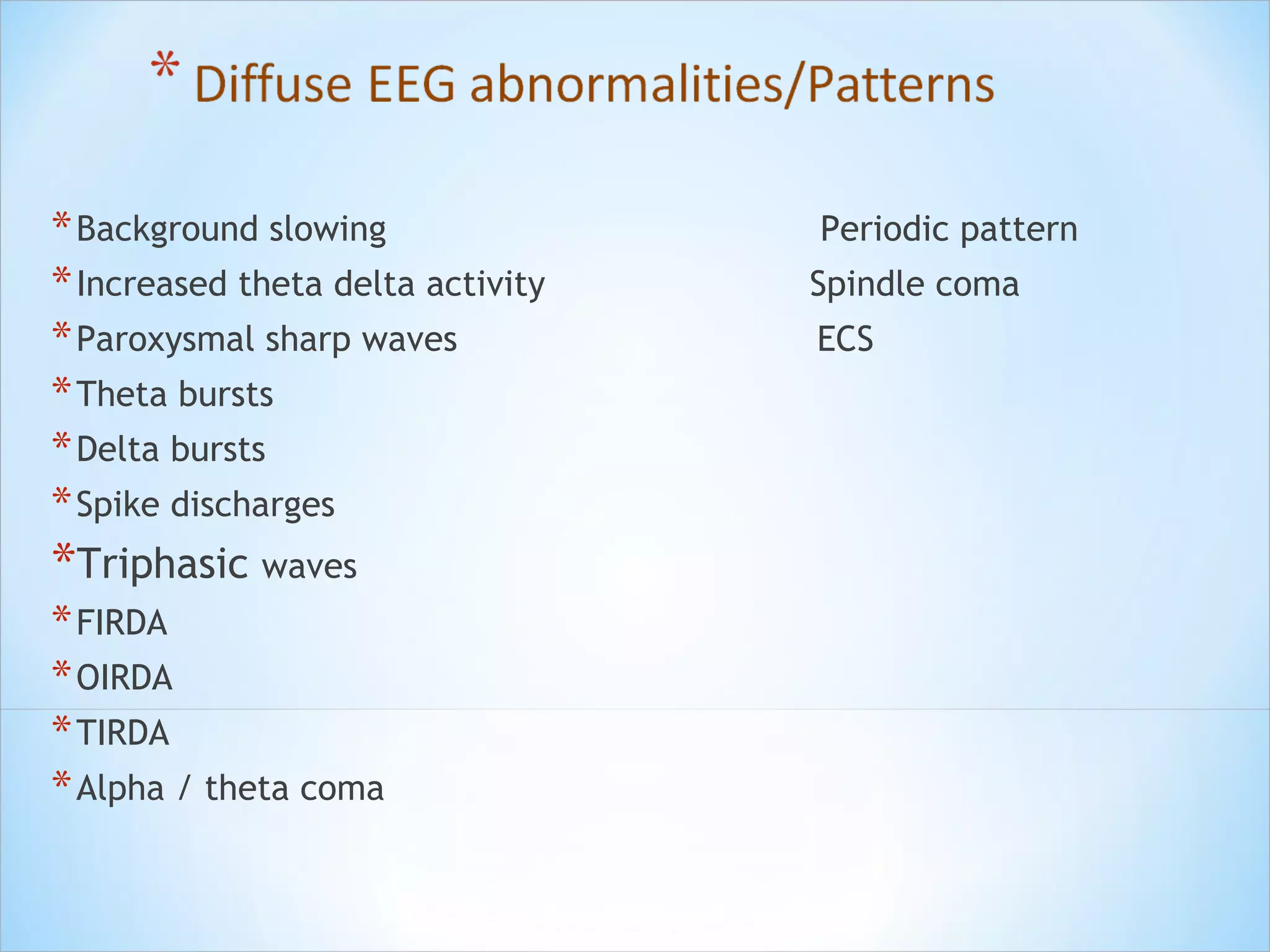
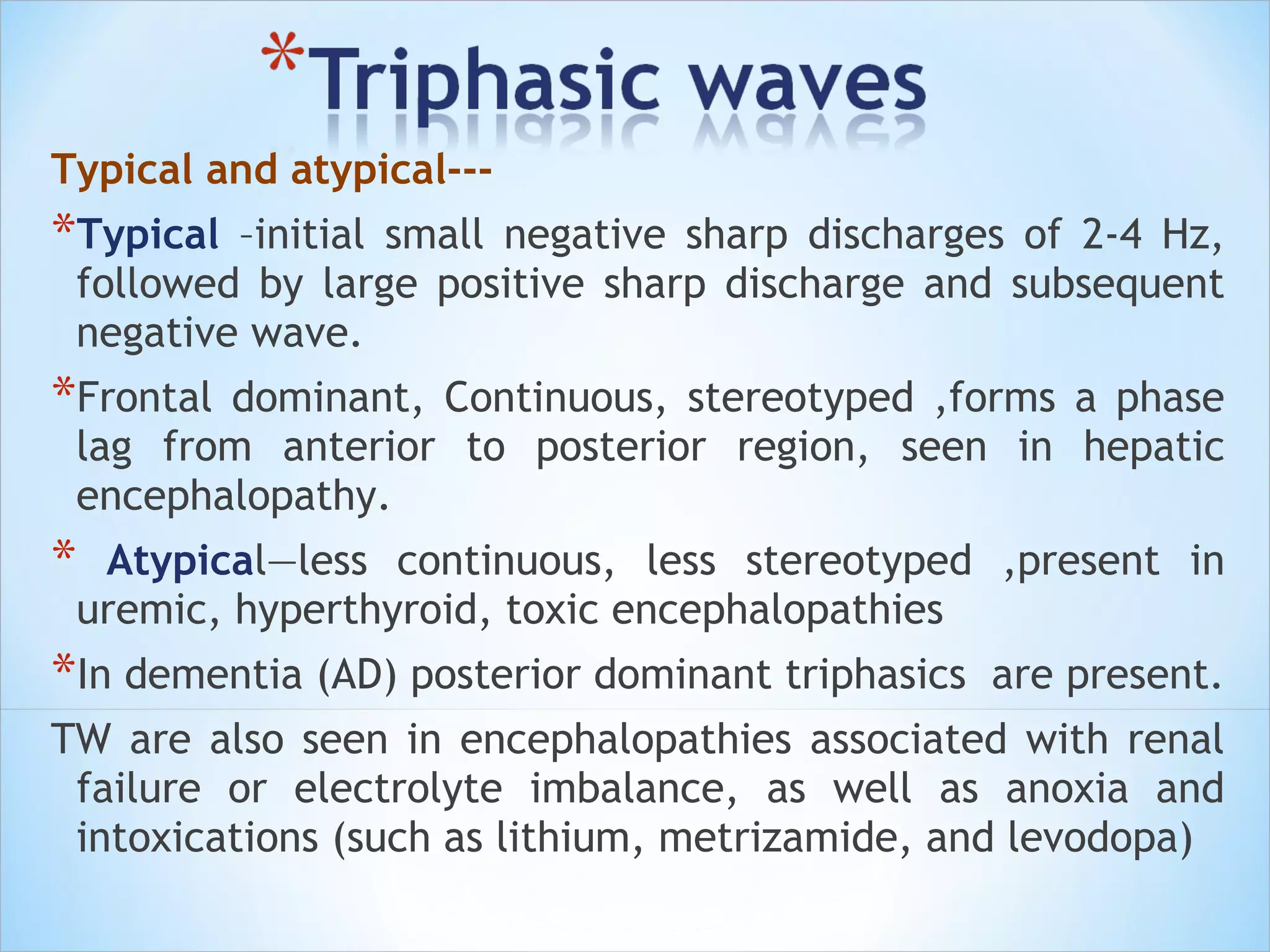
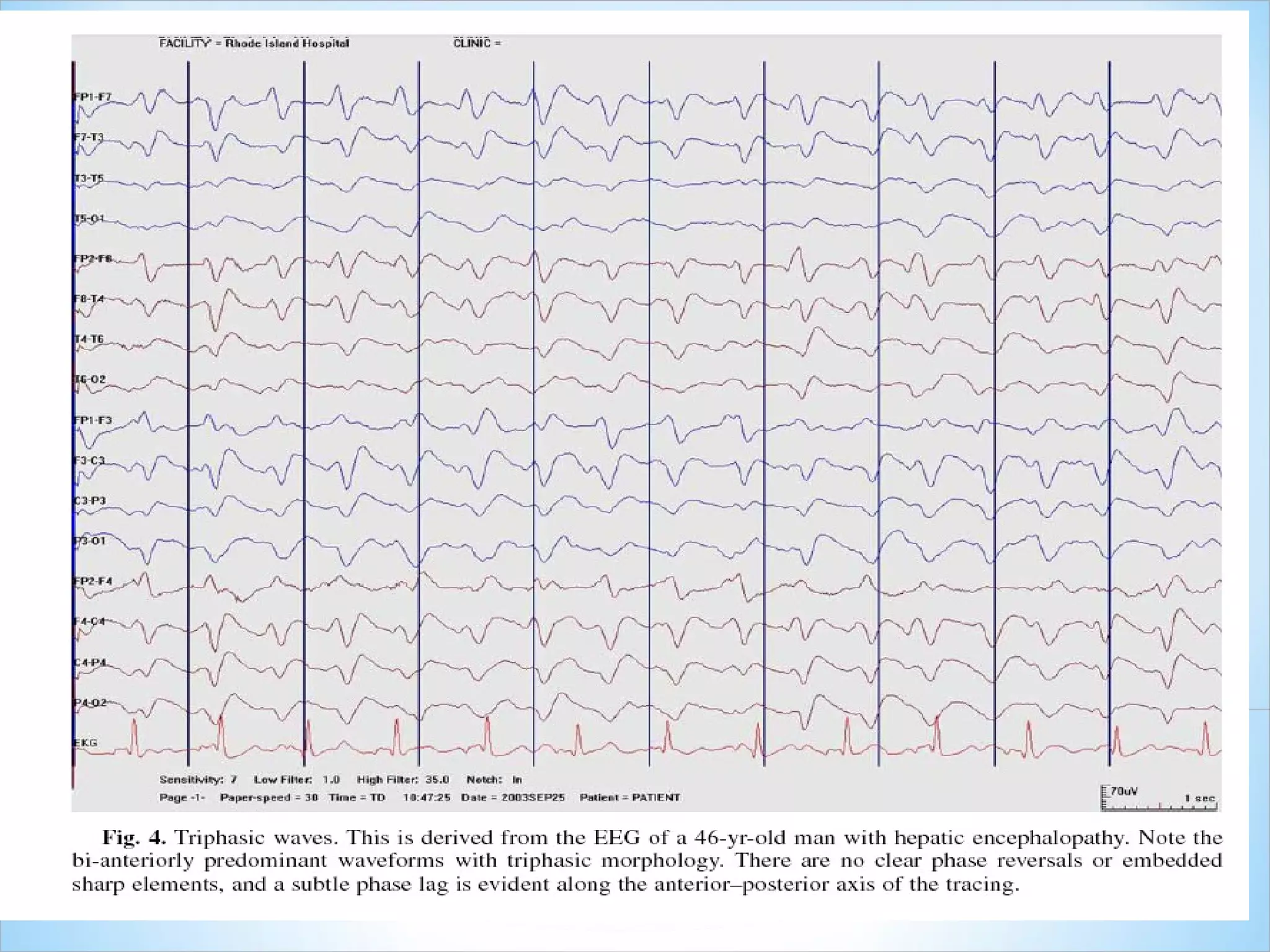
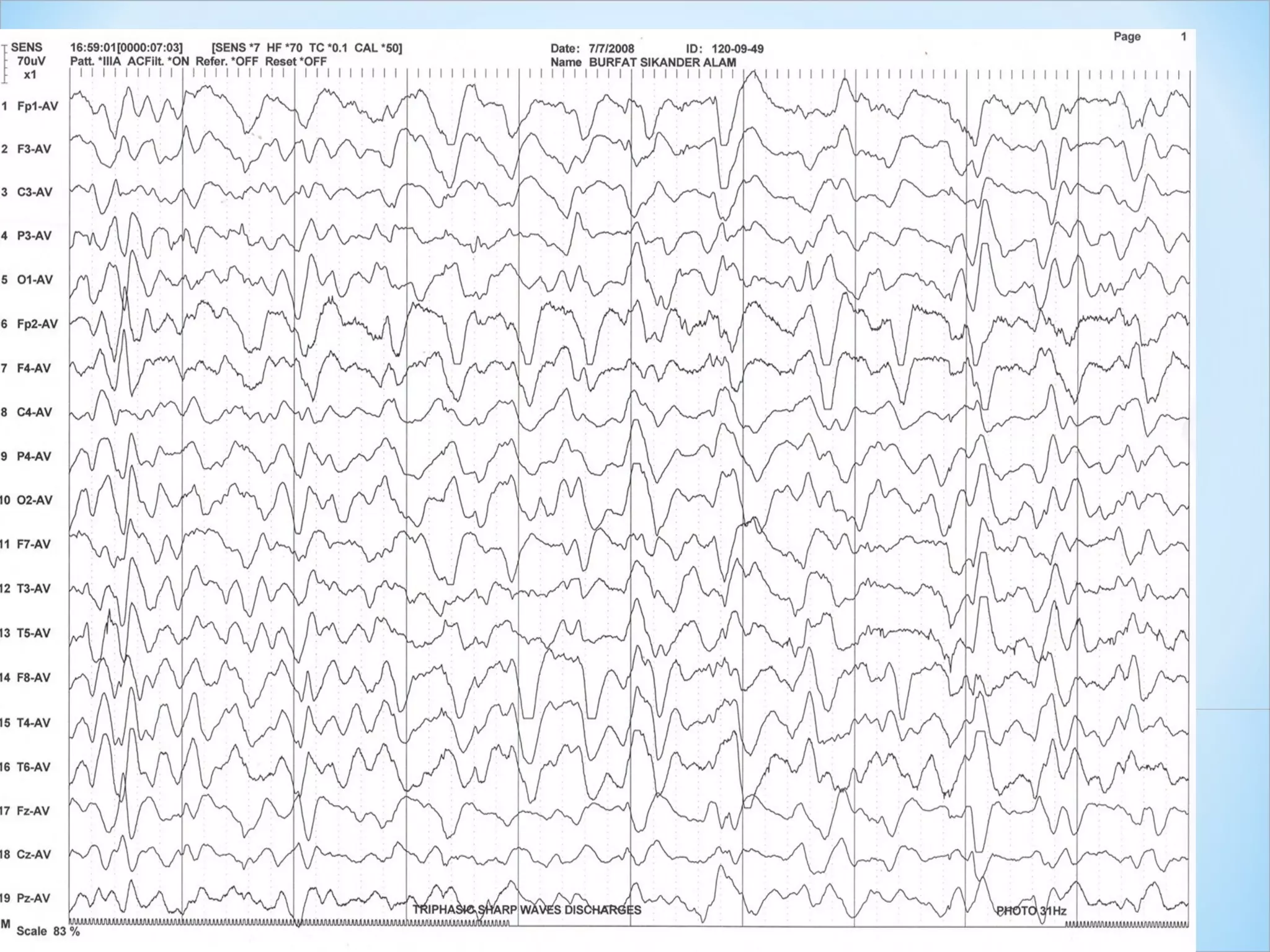
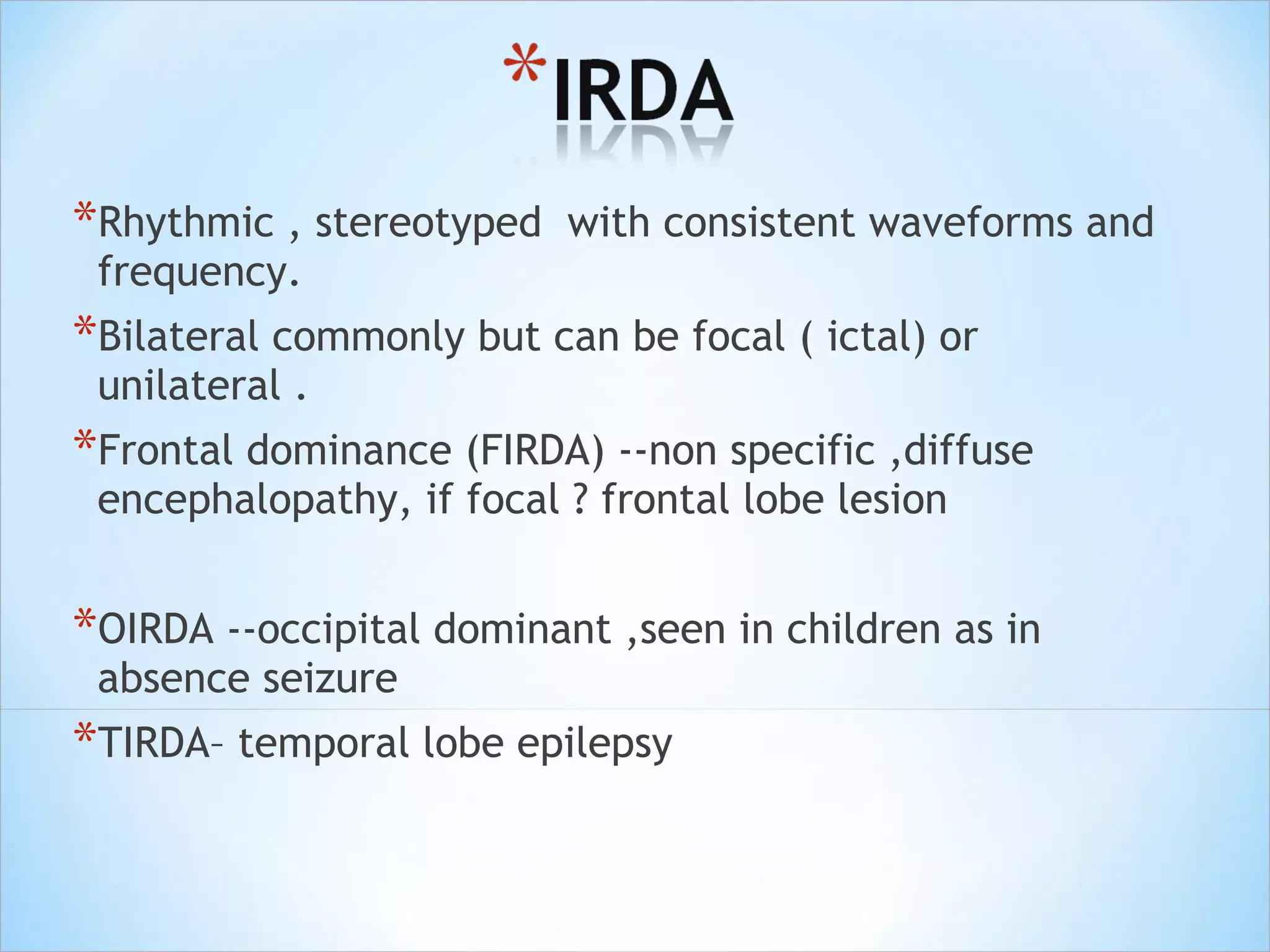
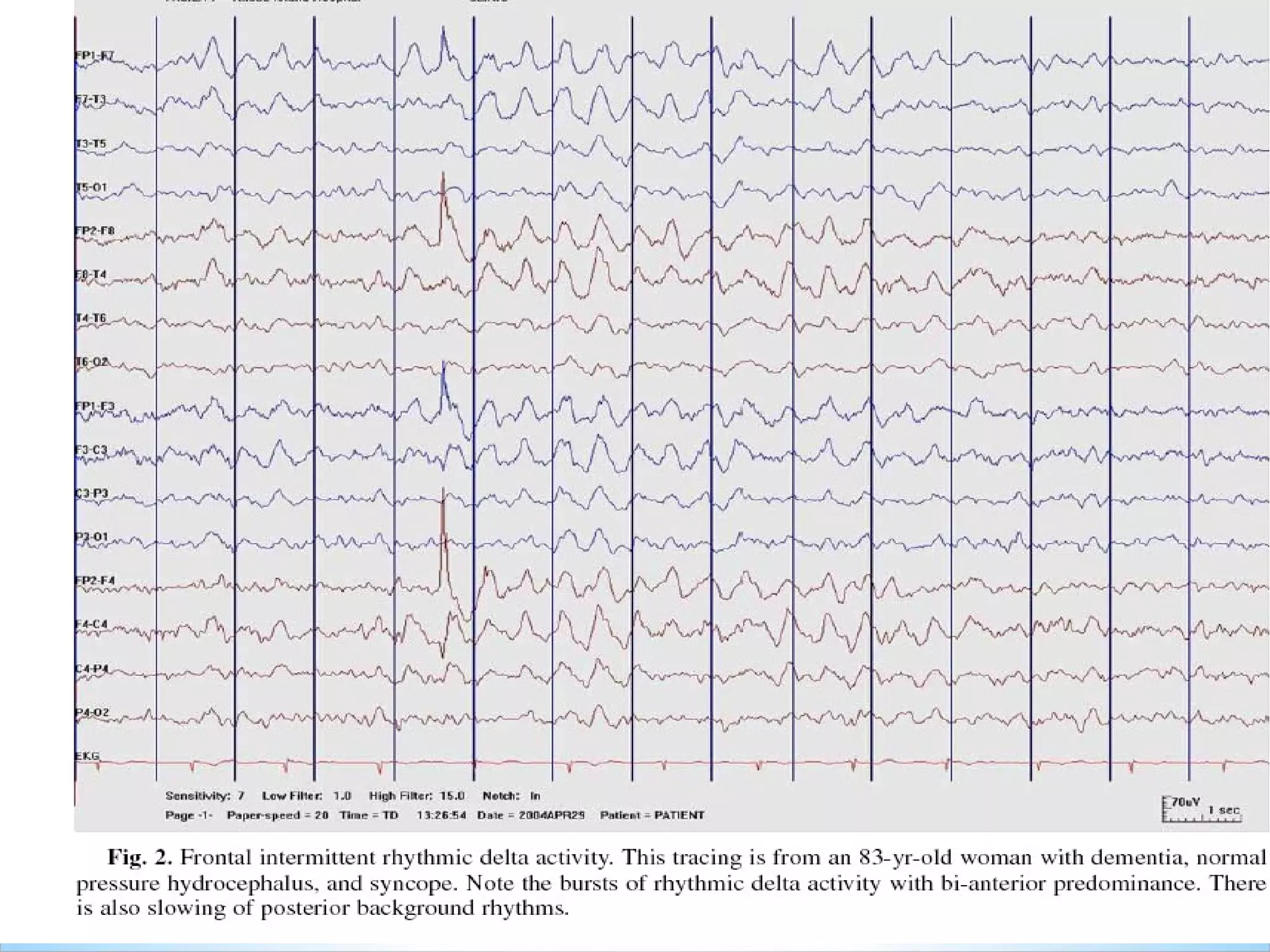
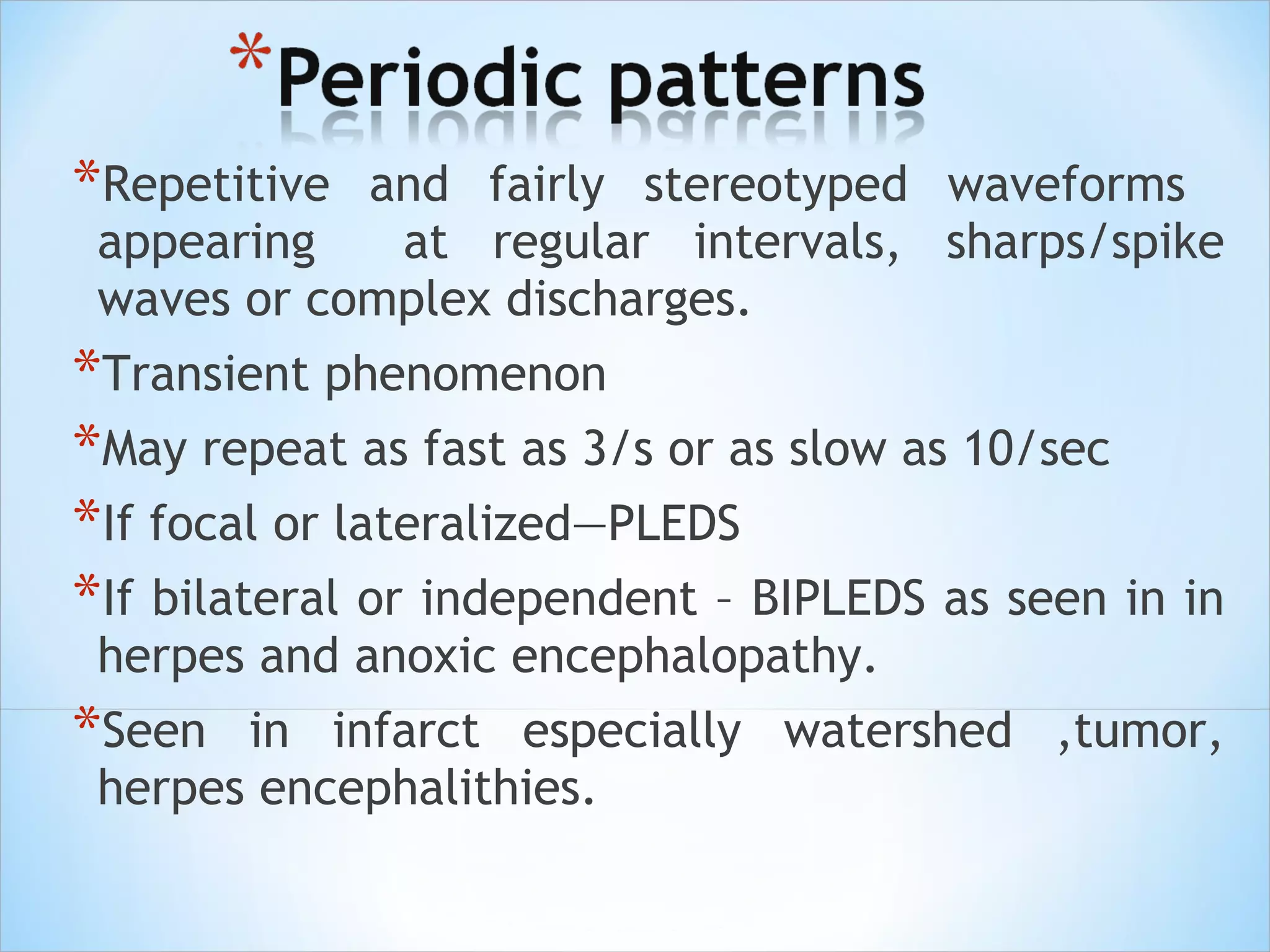
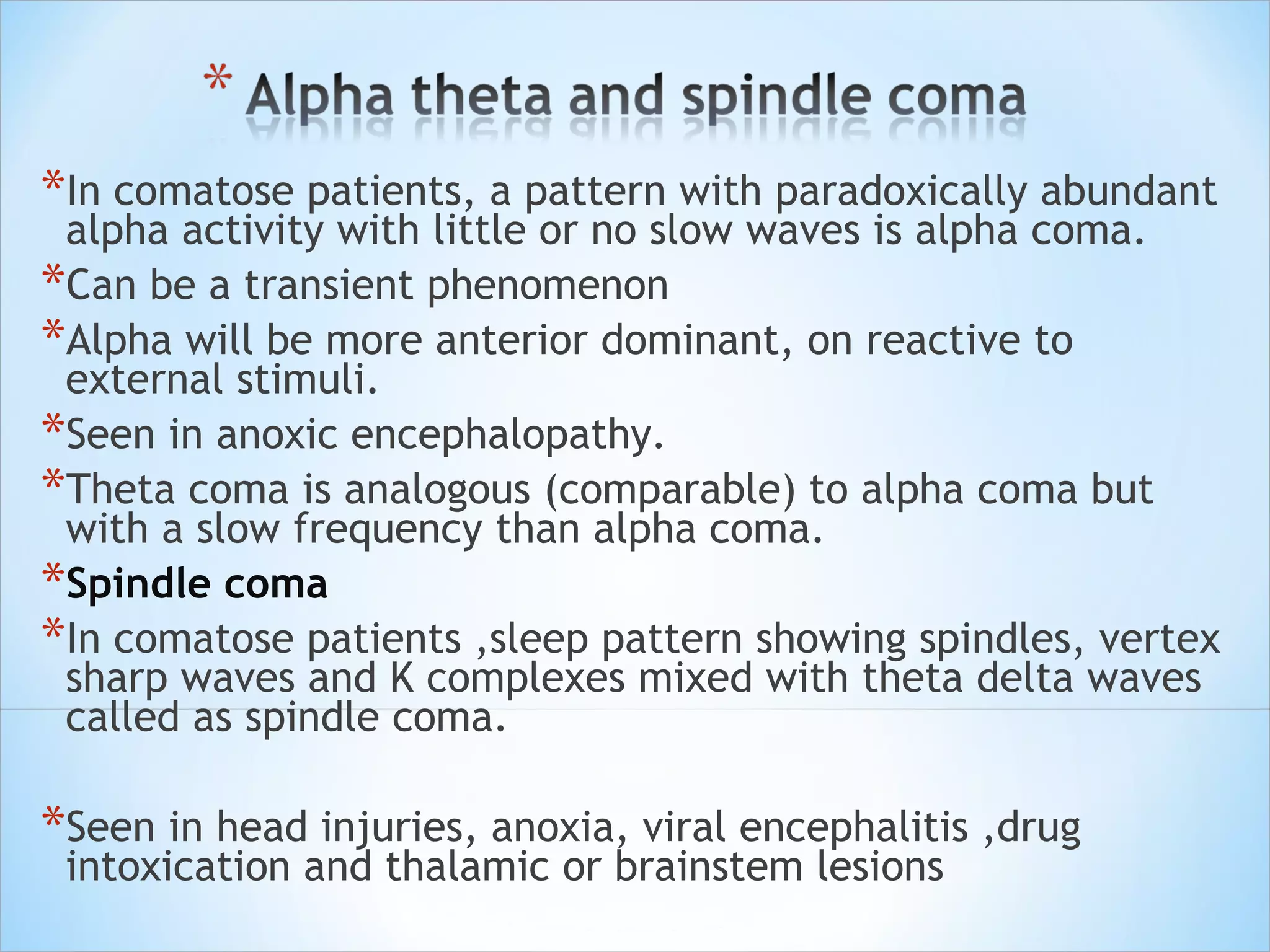
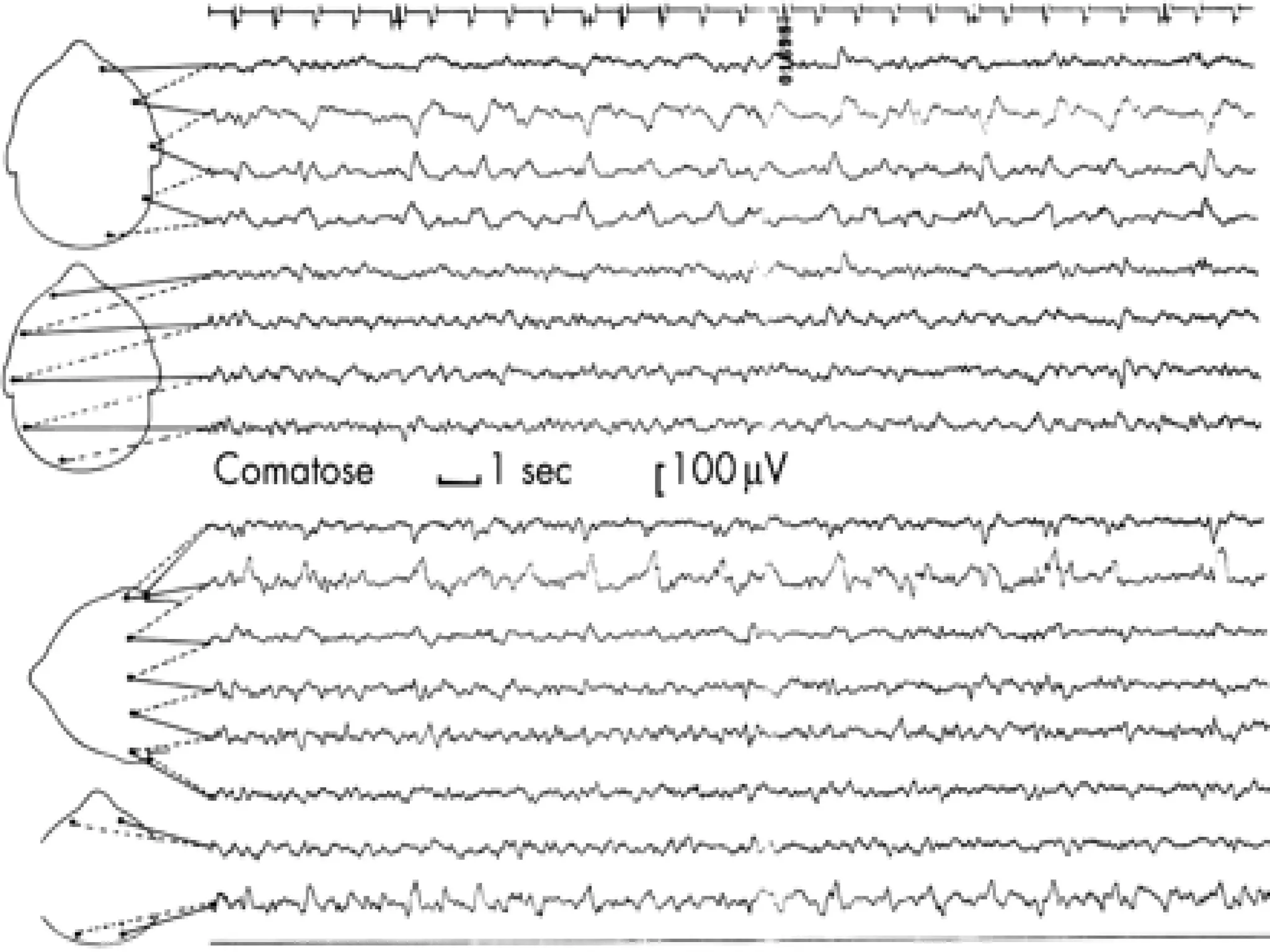
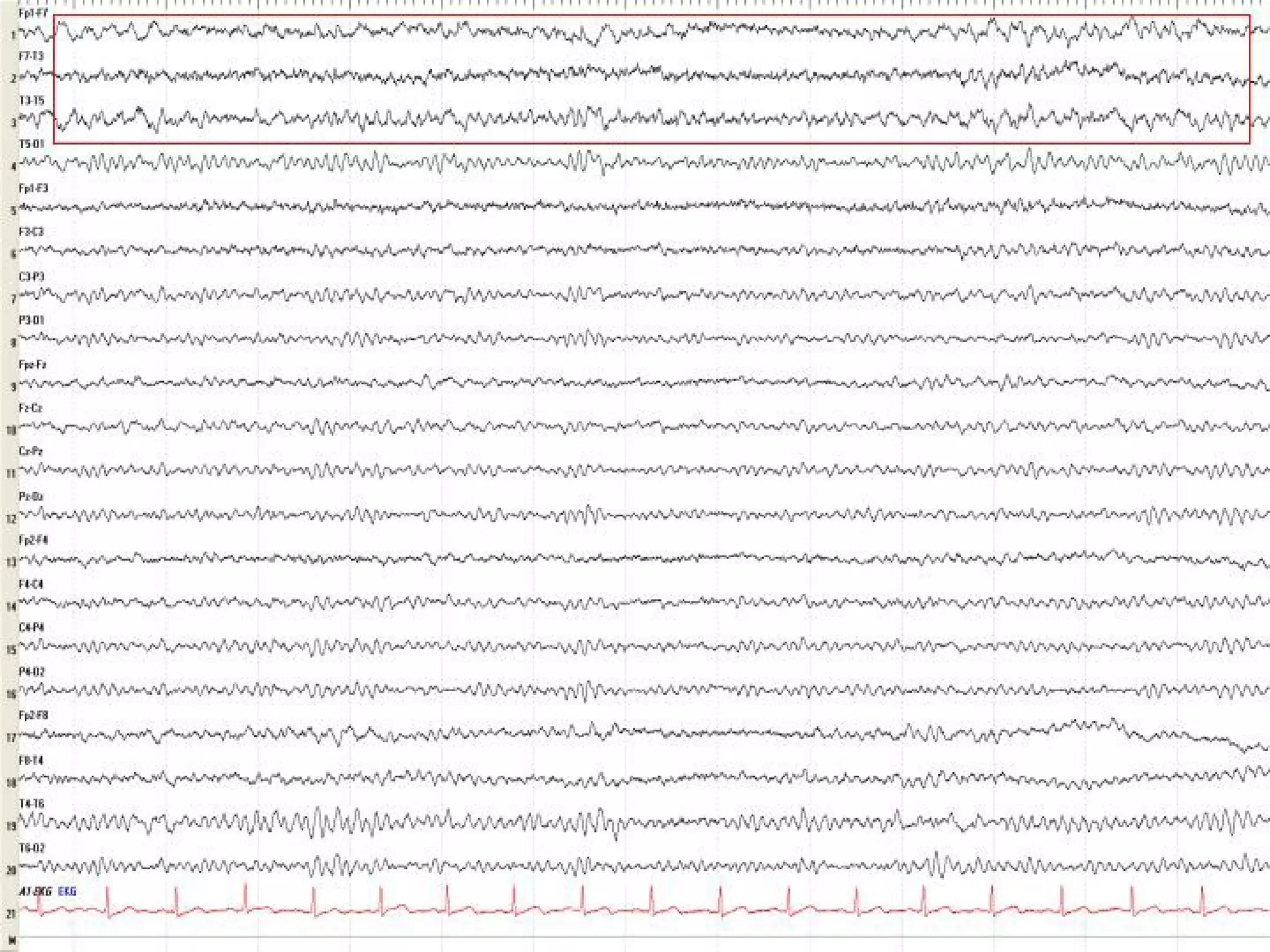
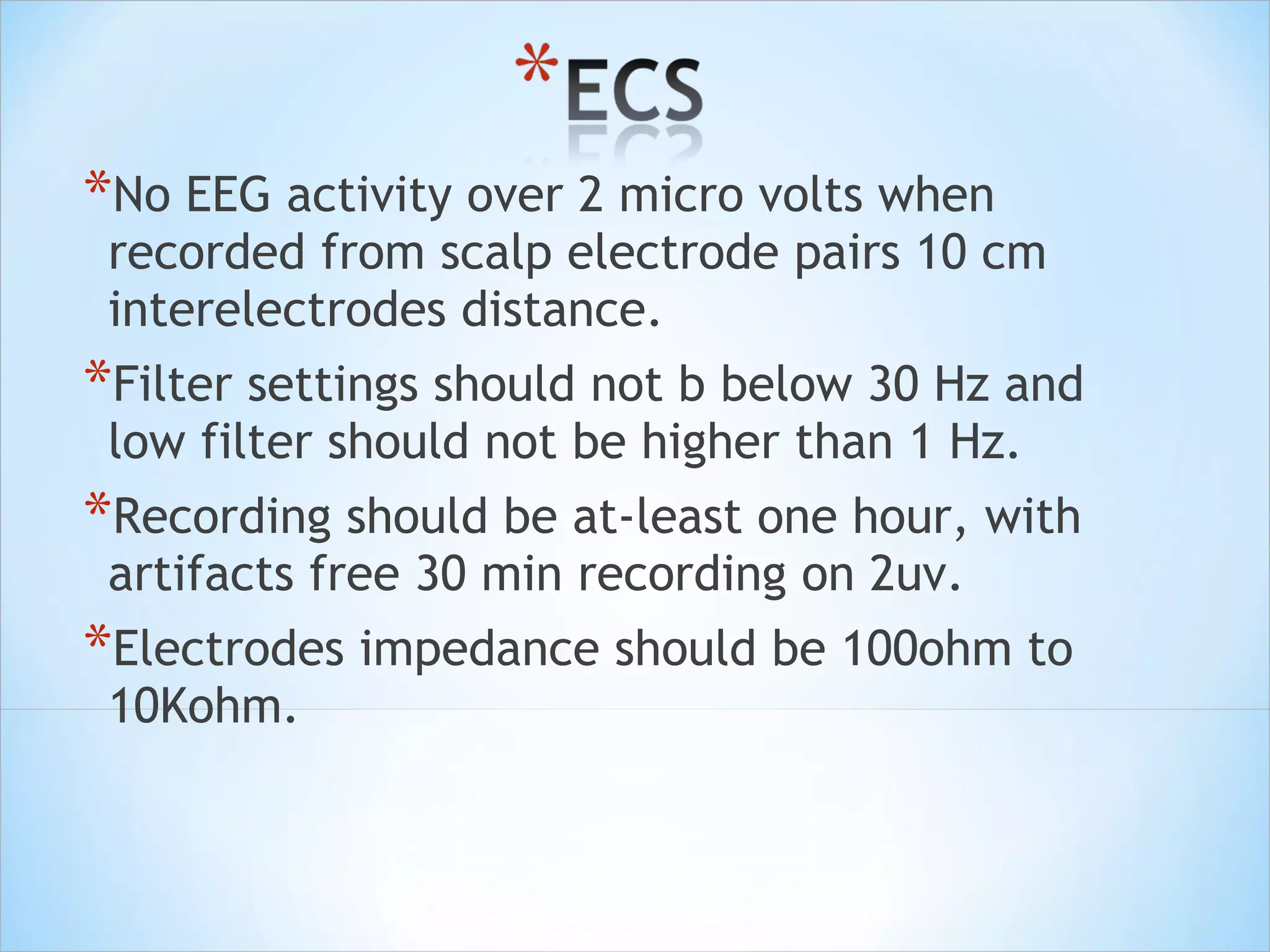
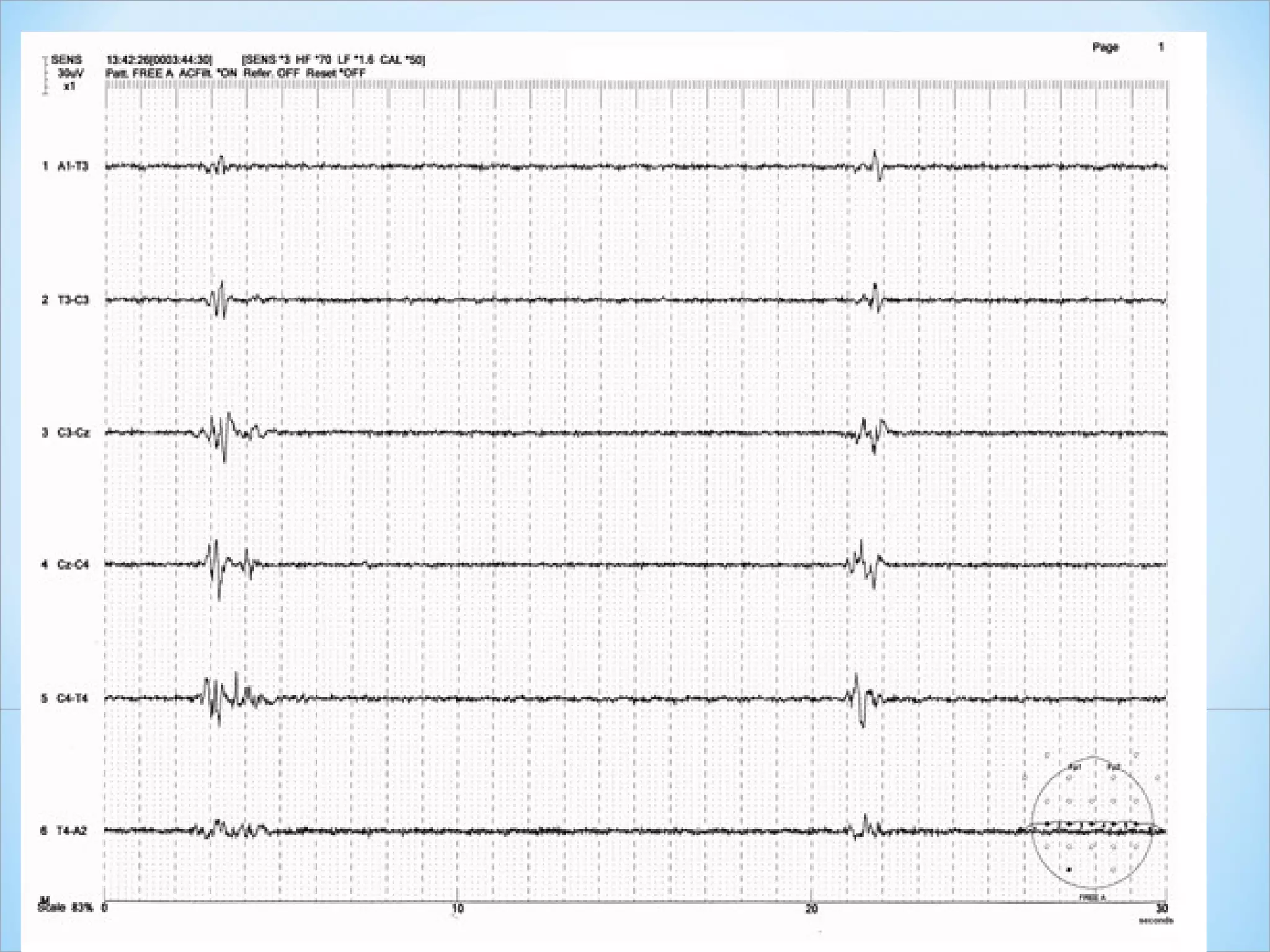
This document discusses encephalopathy and summarizes key points about its causes, features on EEG, and types. Encephalopathy is defined as altered brain function resulting in impaired consciousness. It can be caused by metabolic, toxic, infectious, hepatic or other issues. On EEG, encephalopathy typically shows generalized slowing and reduced reactivity. Specific patterns like triphasic waves indicate metabolic encephalopathy. The document outlines different types of encephalopathy and their associated EEG findings to help evaluate severity and guide treatment.