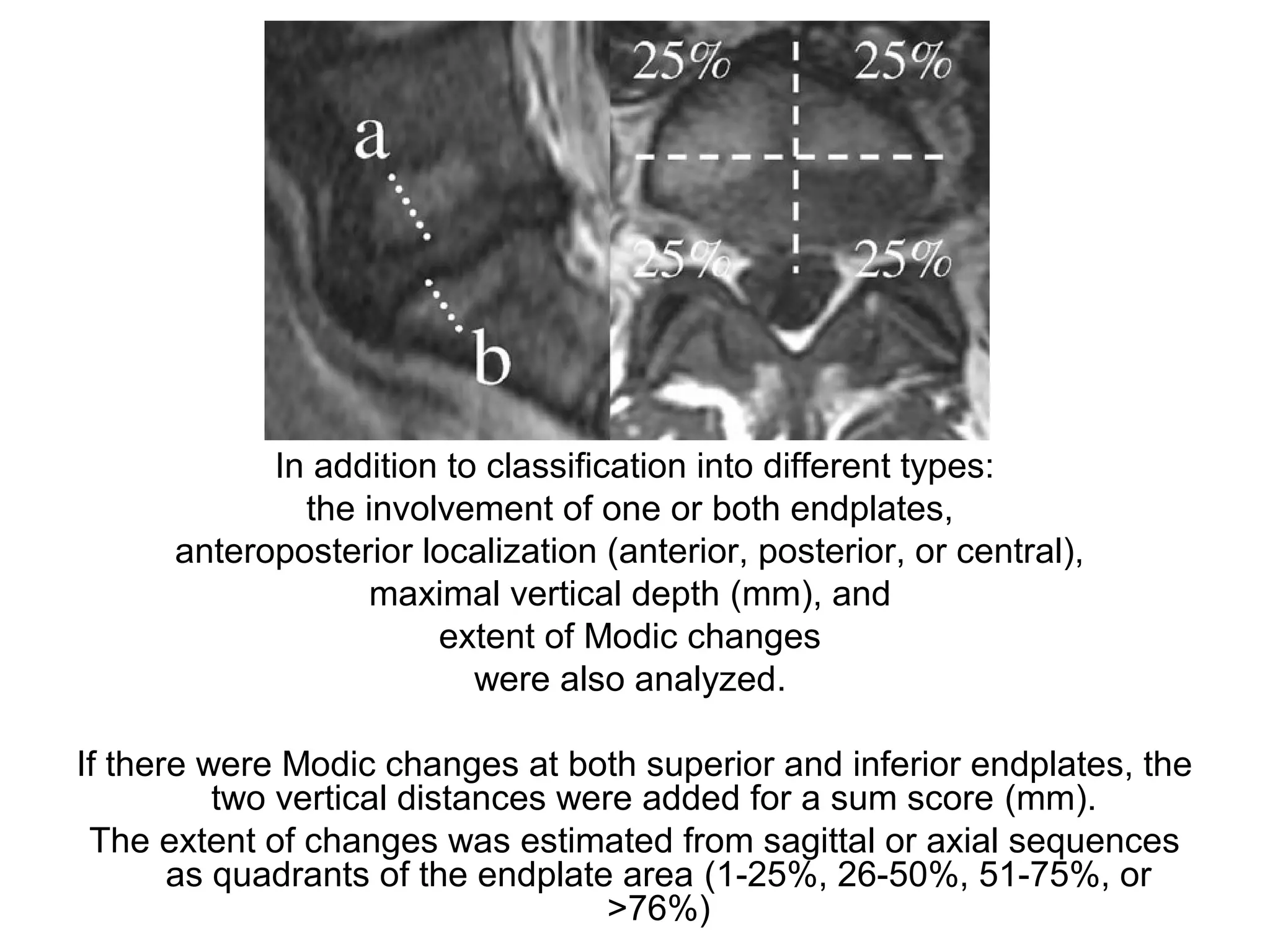
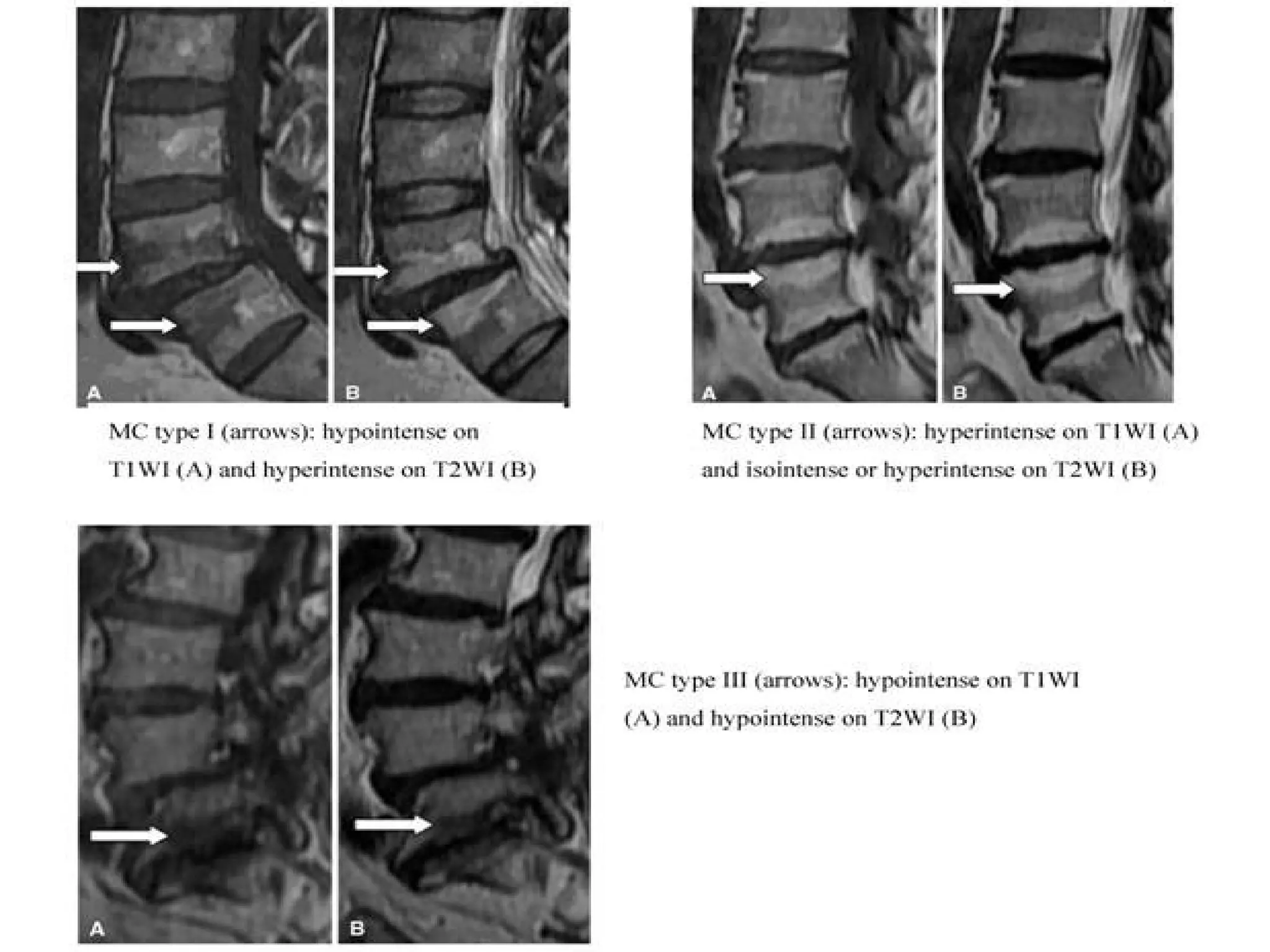
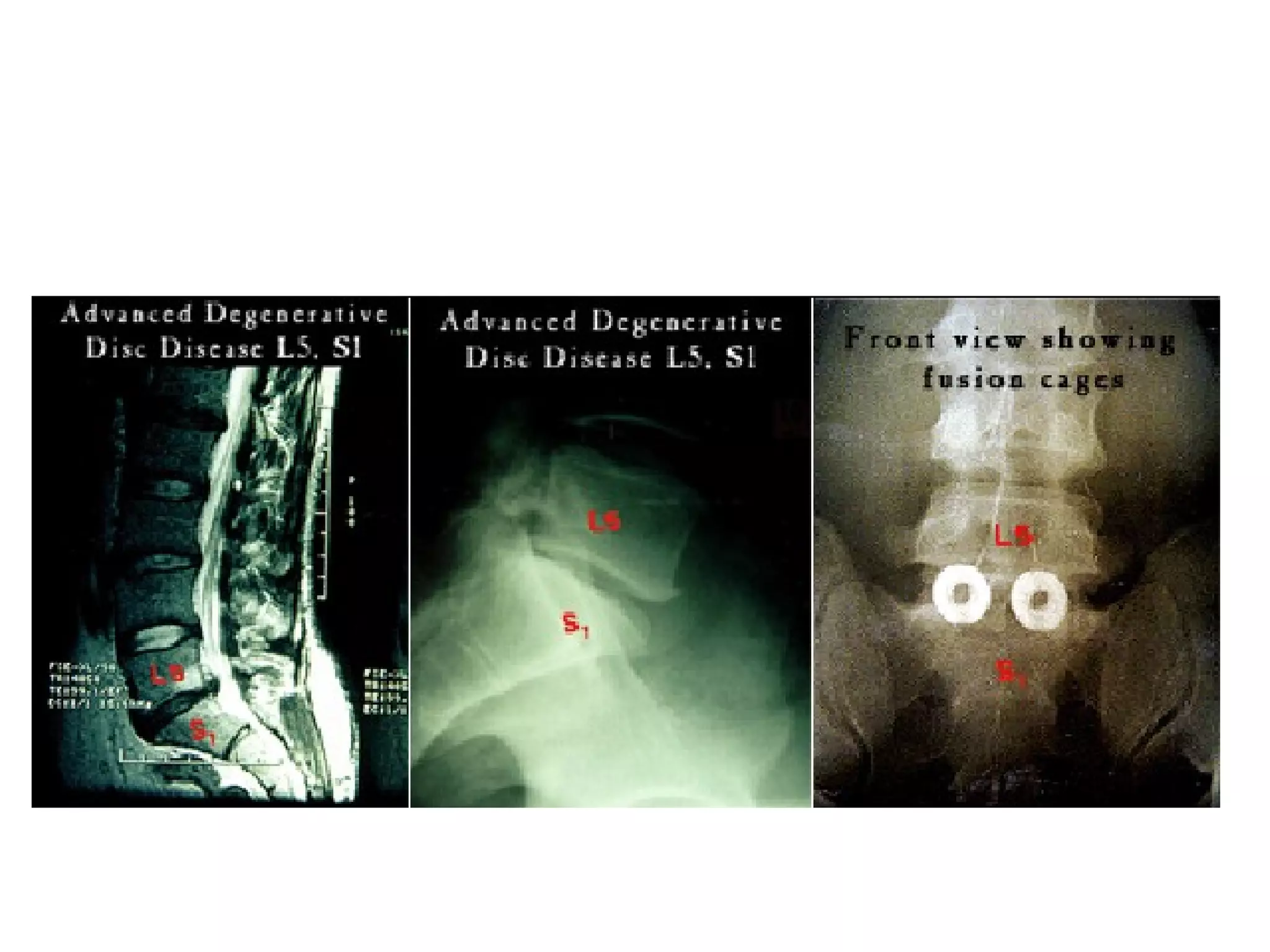
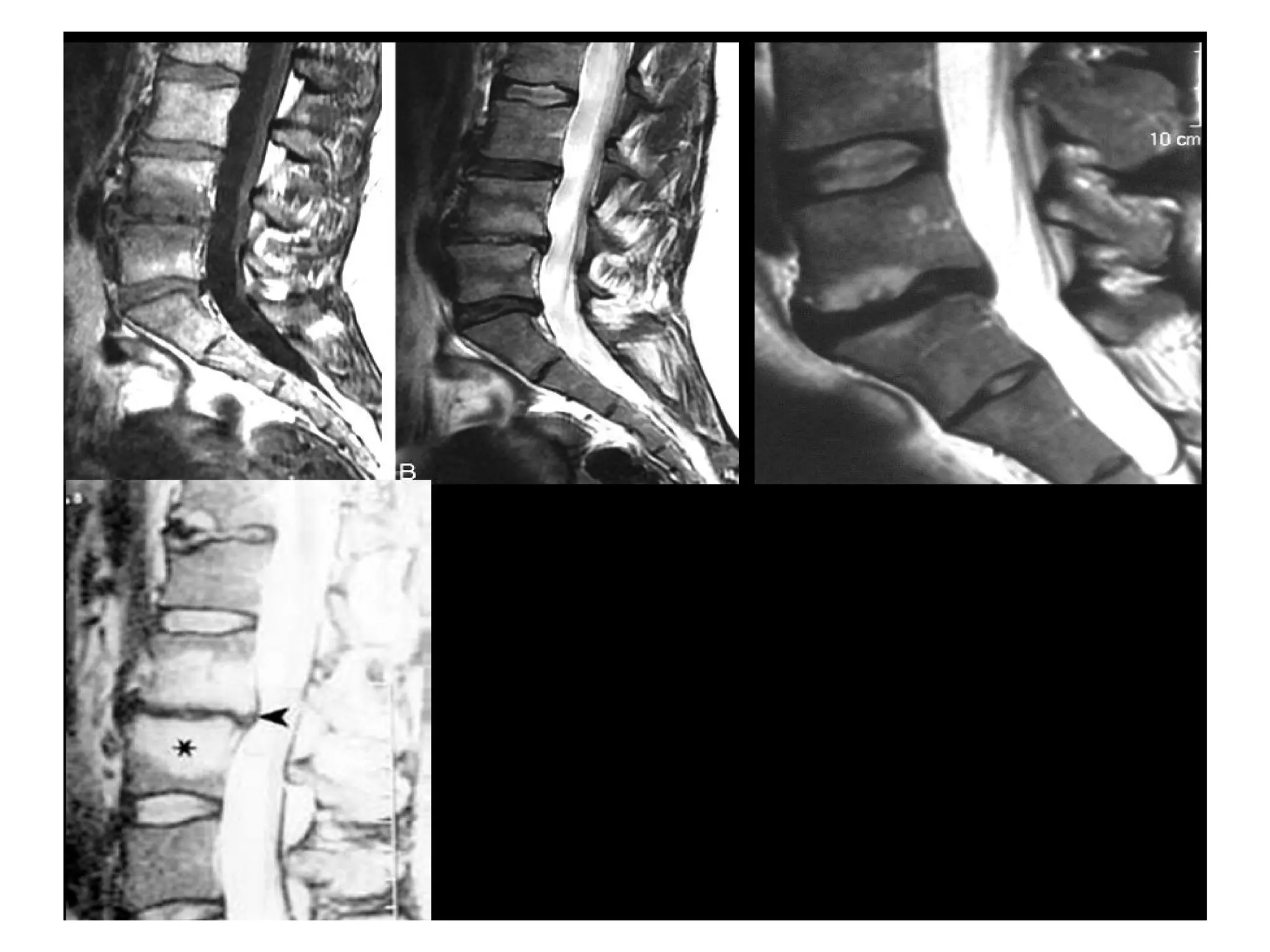
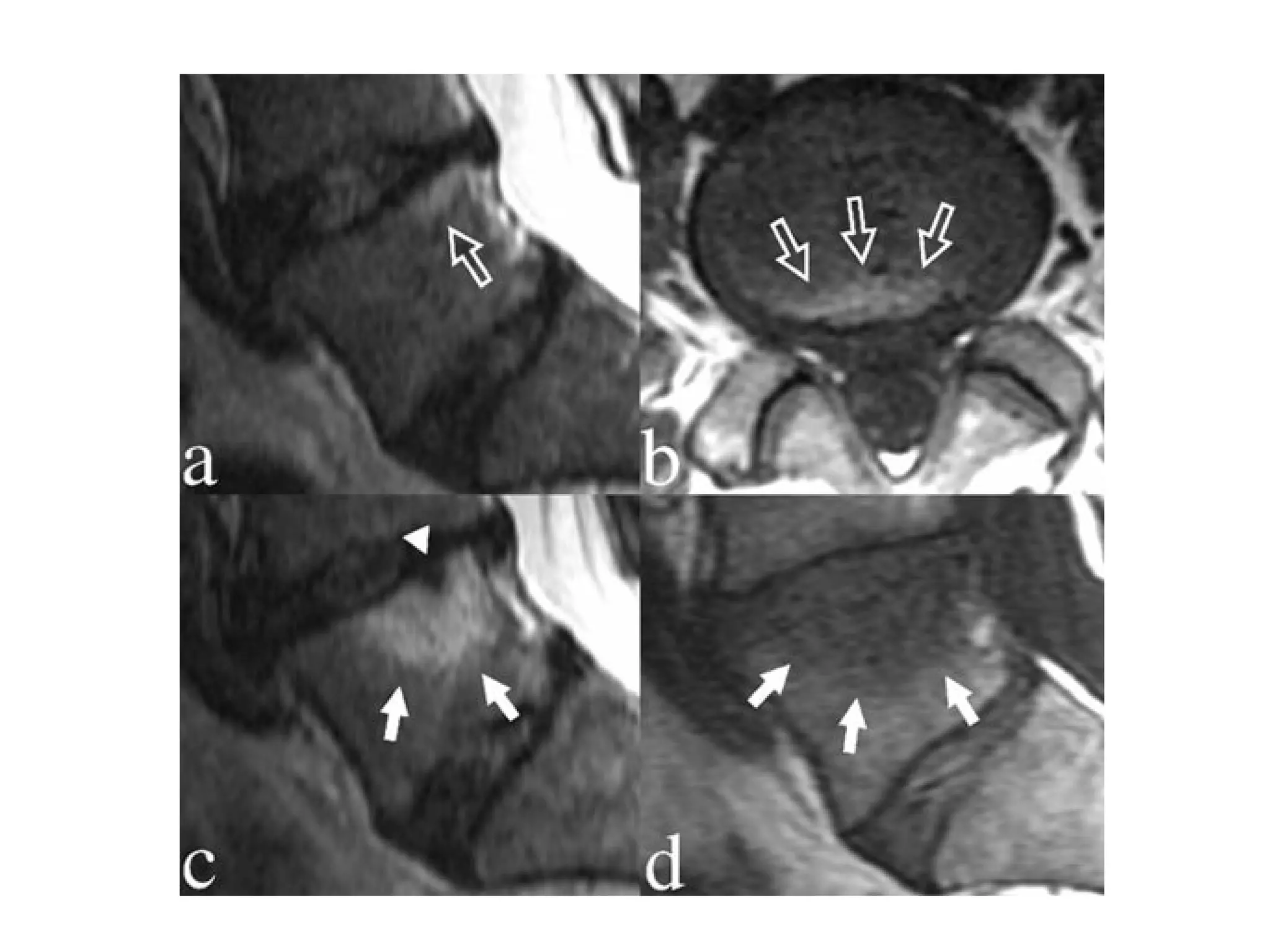
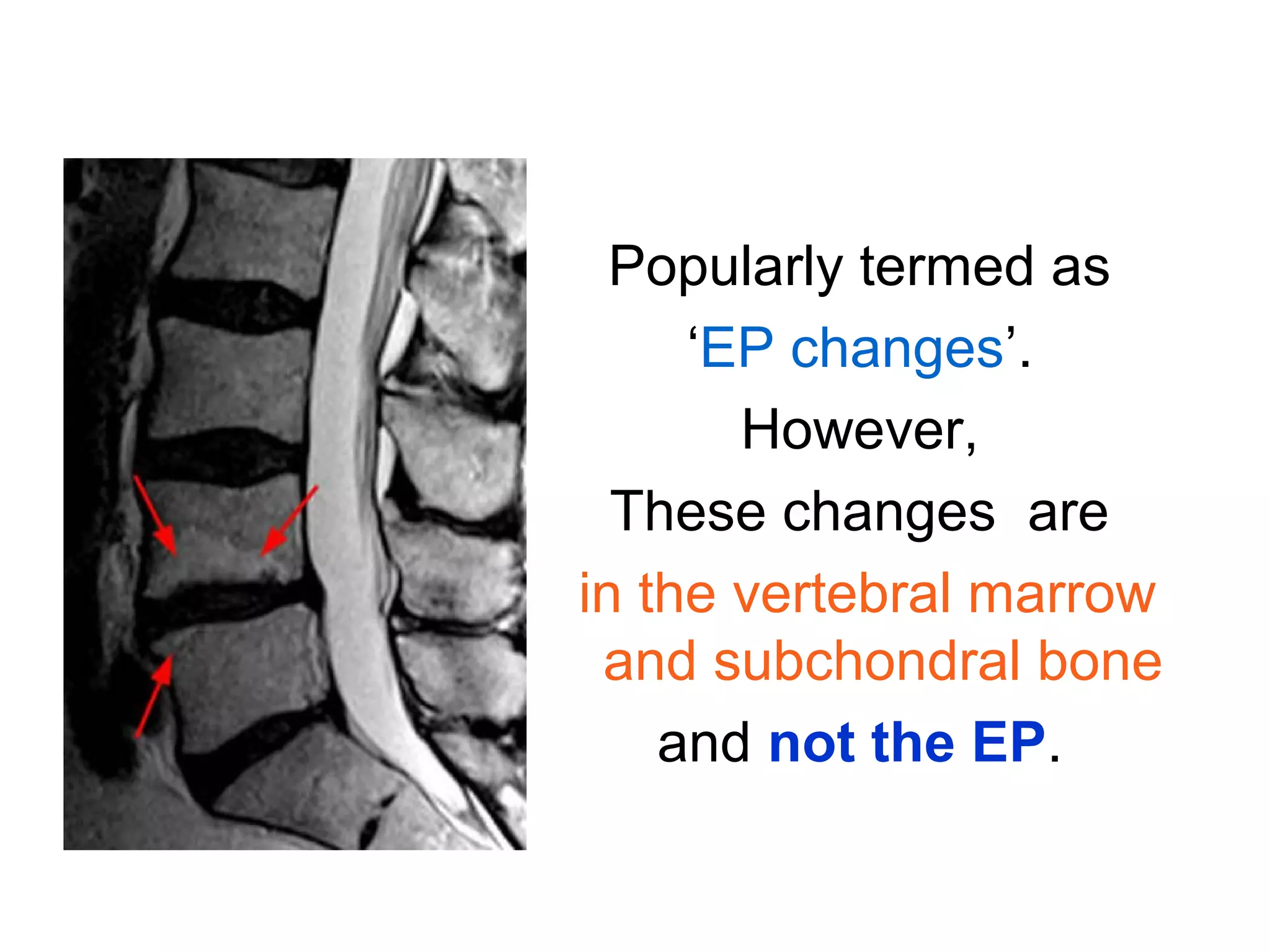
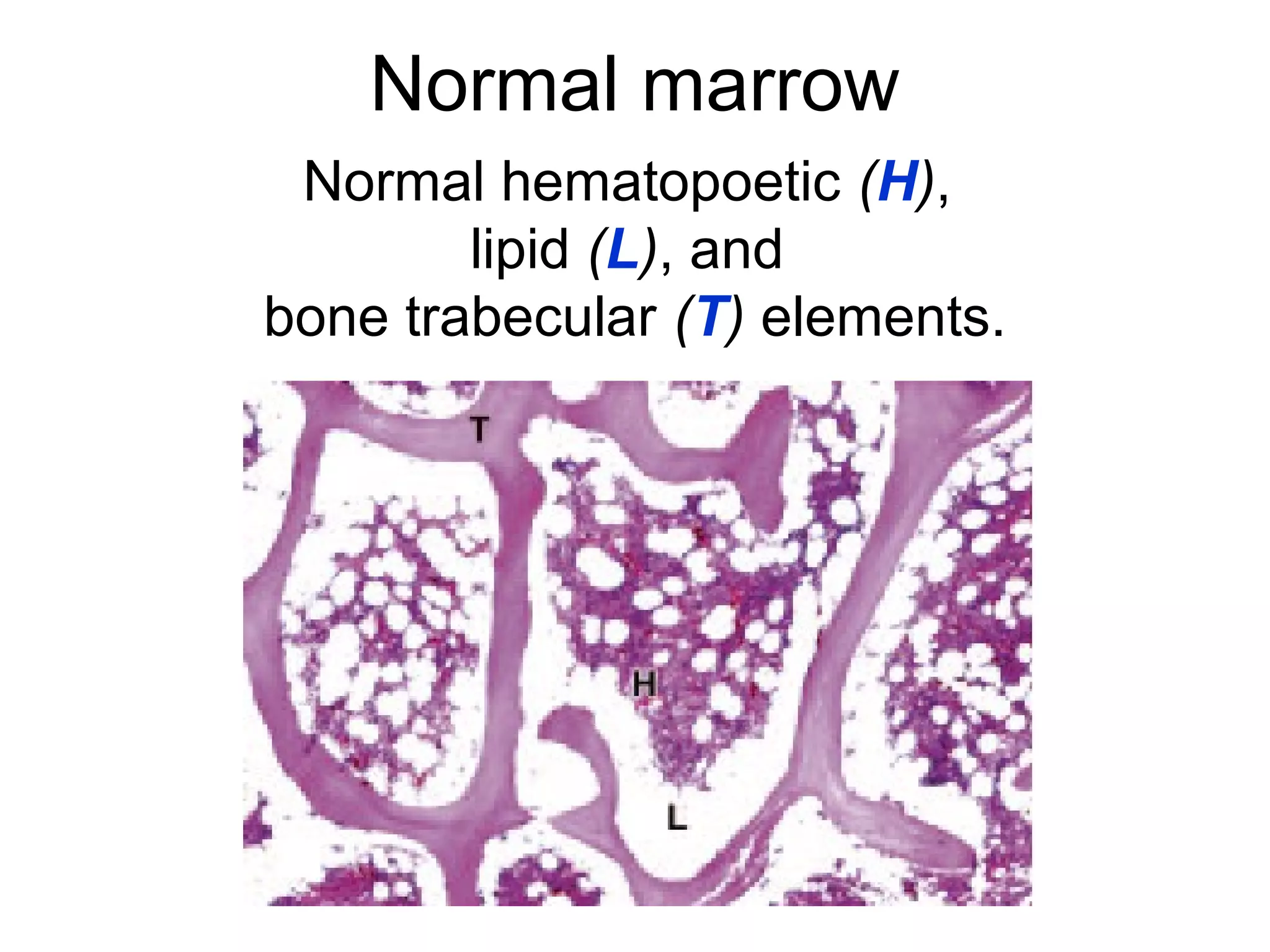
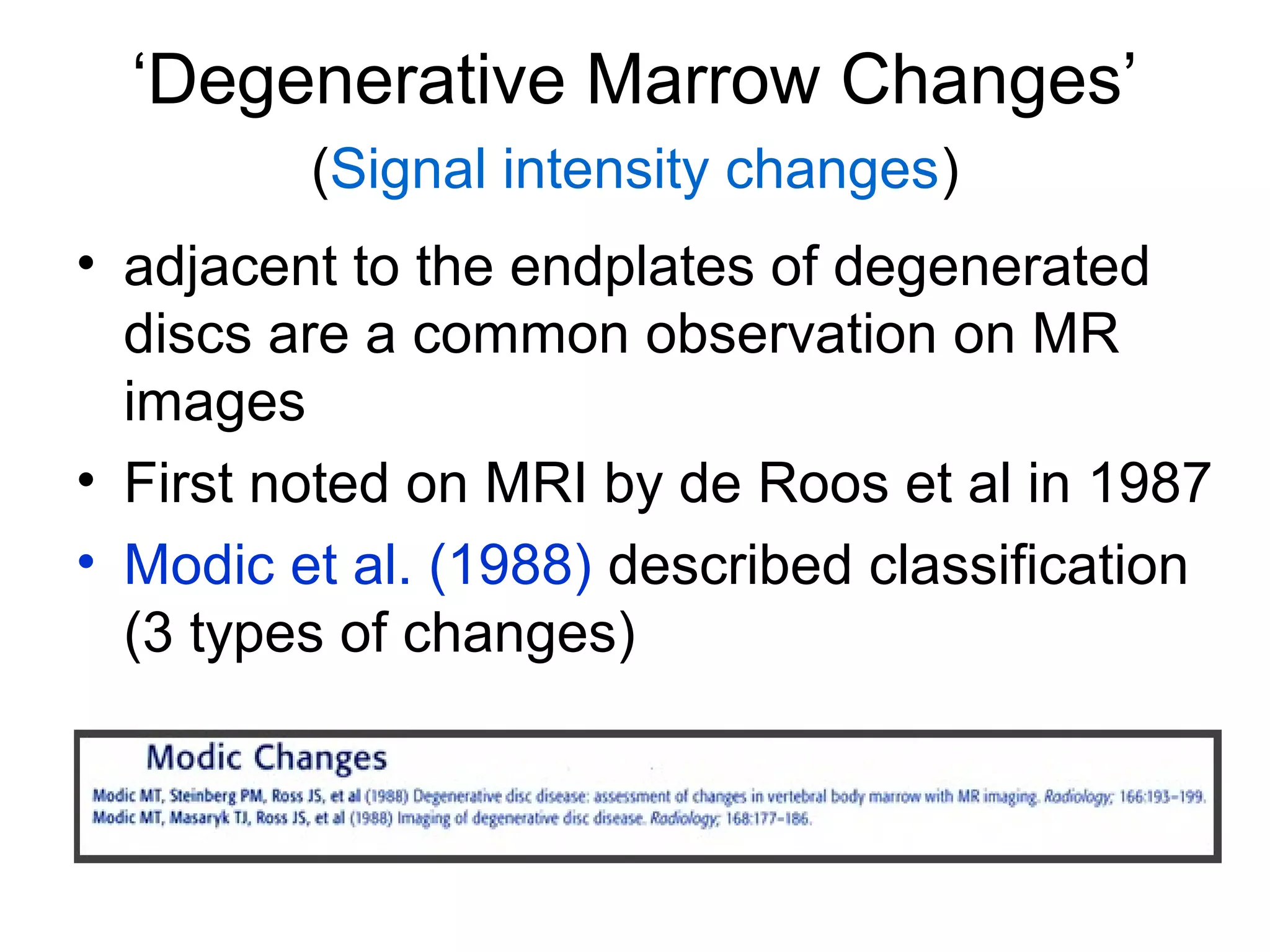
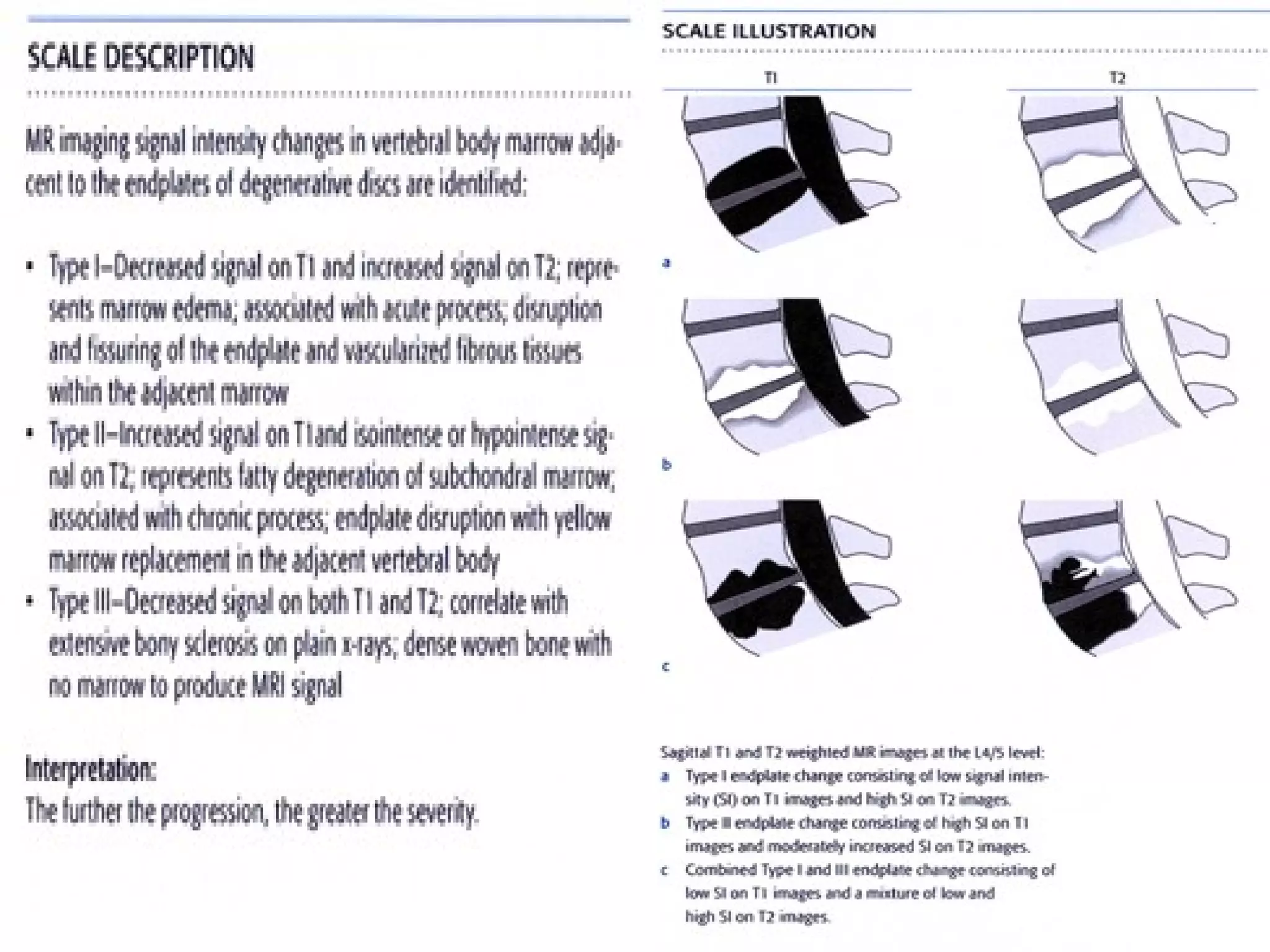
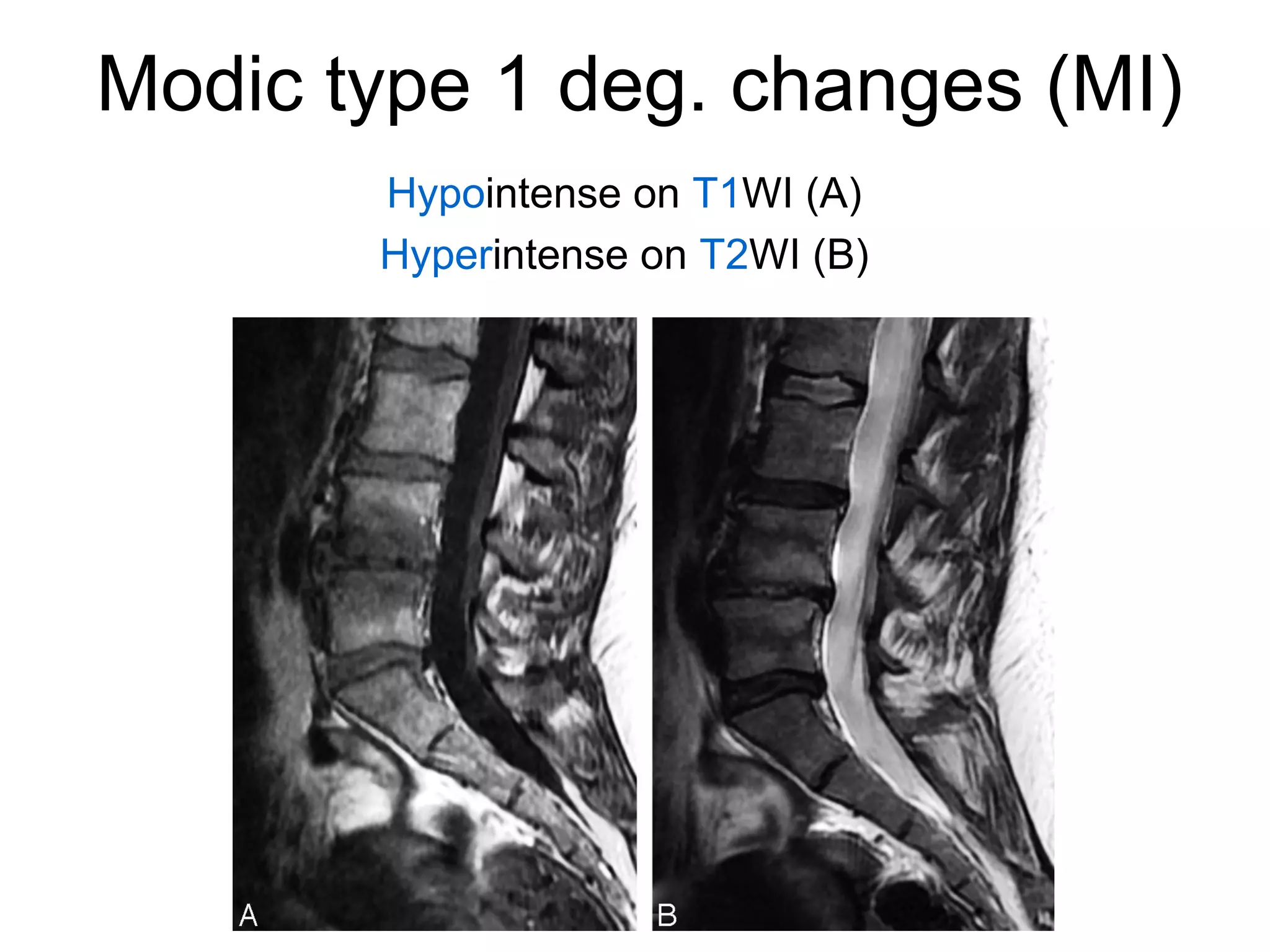
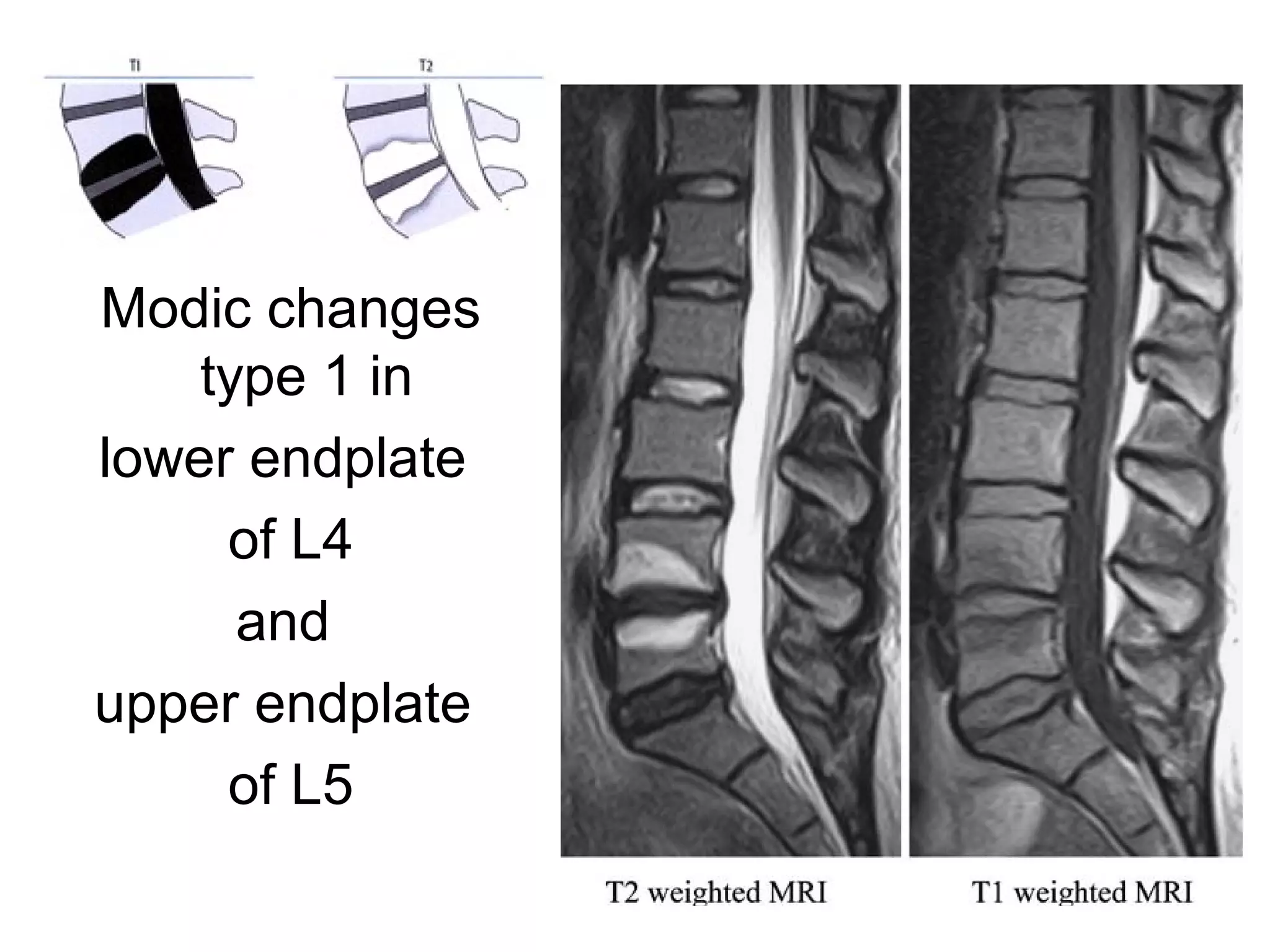
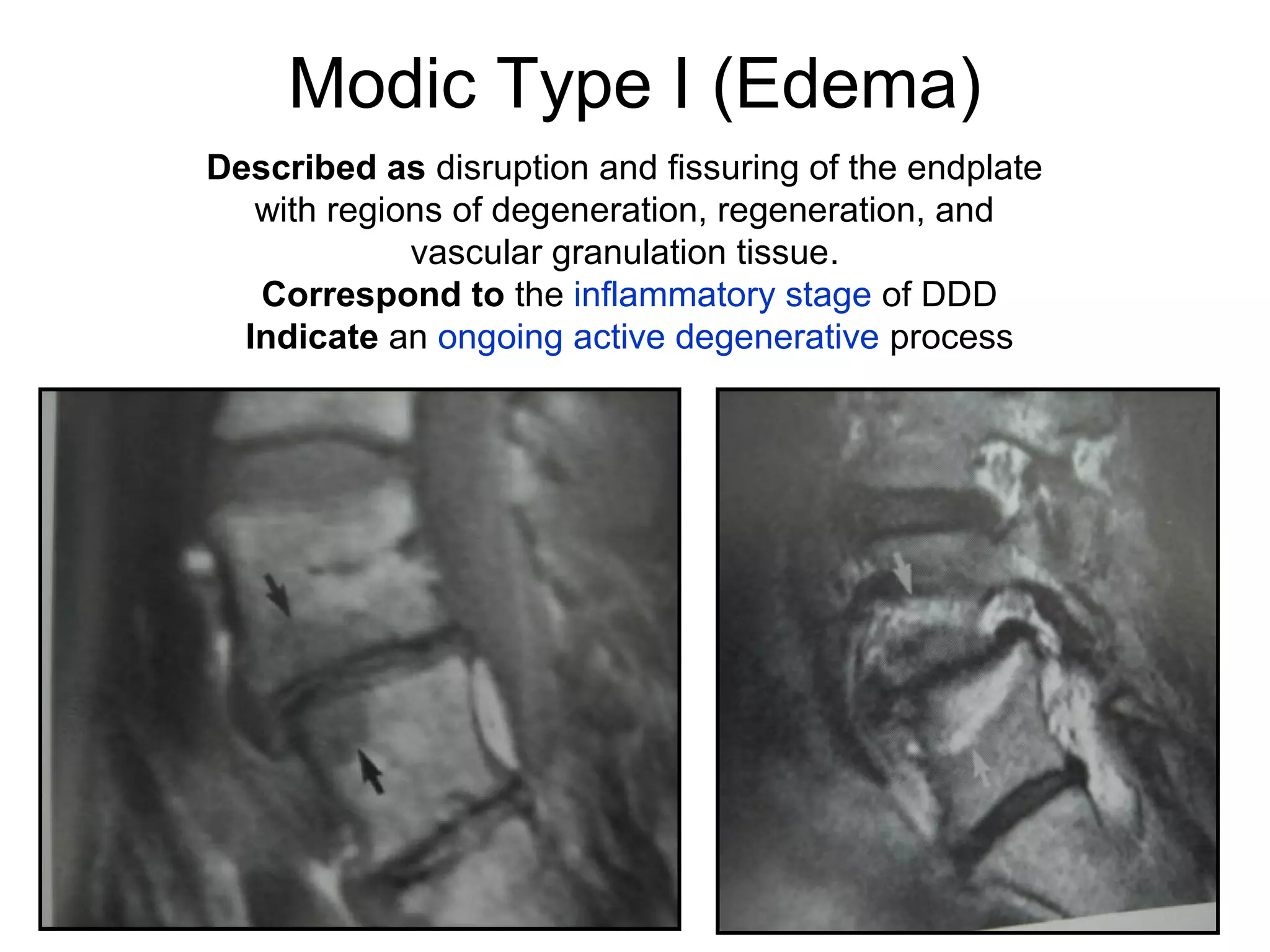
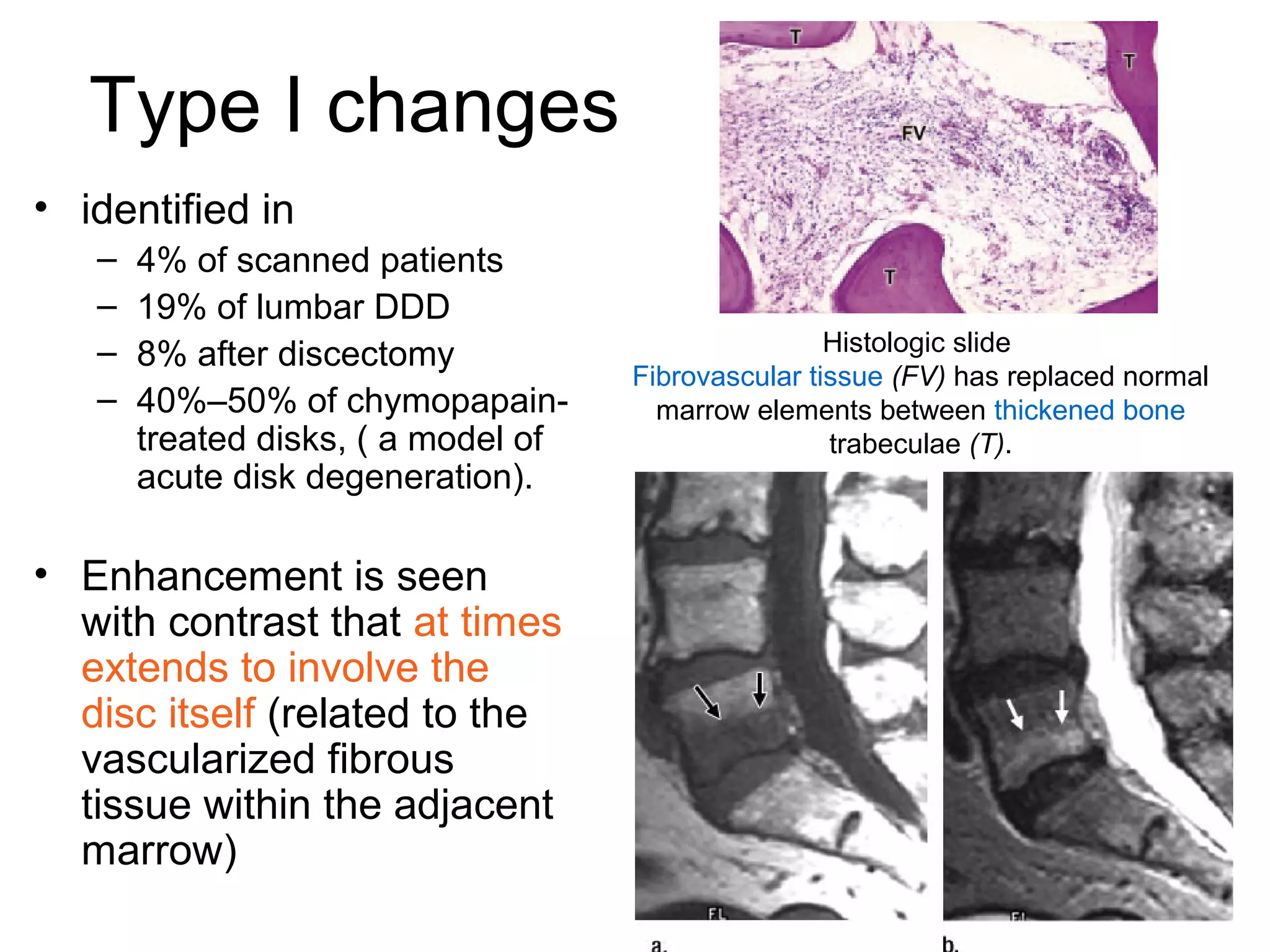
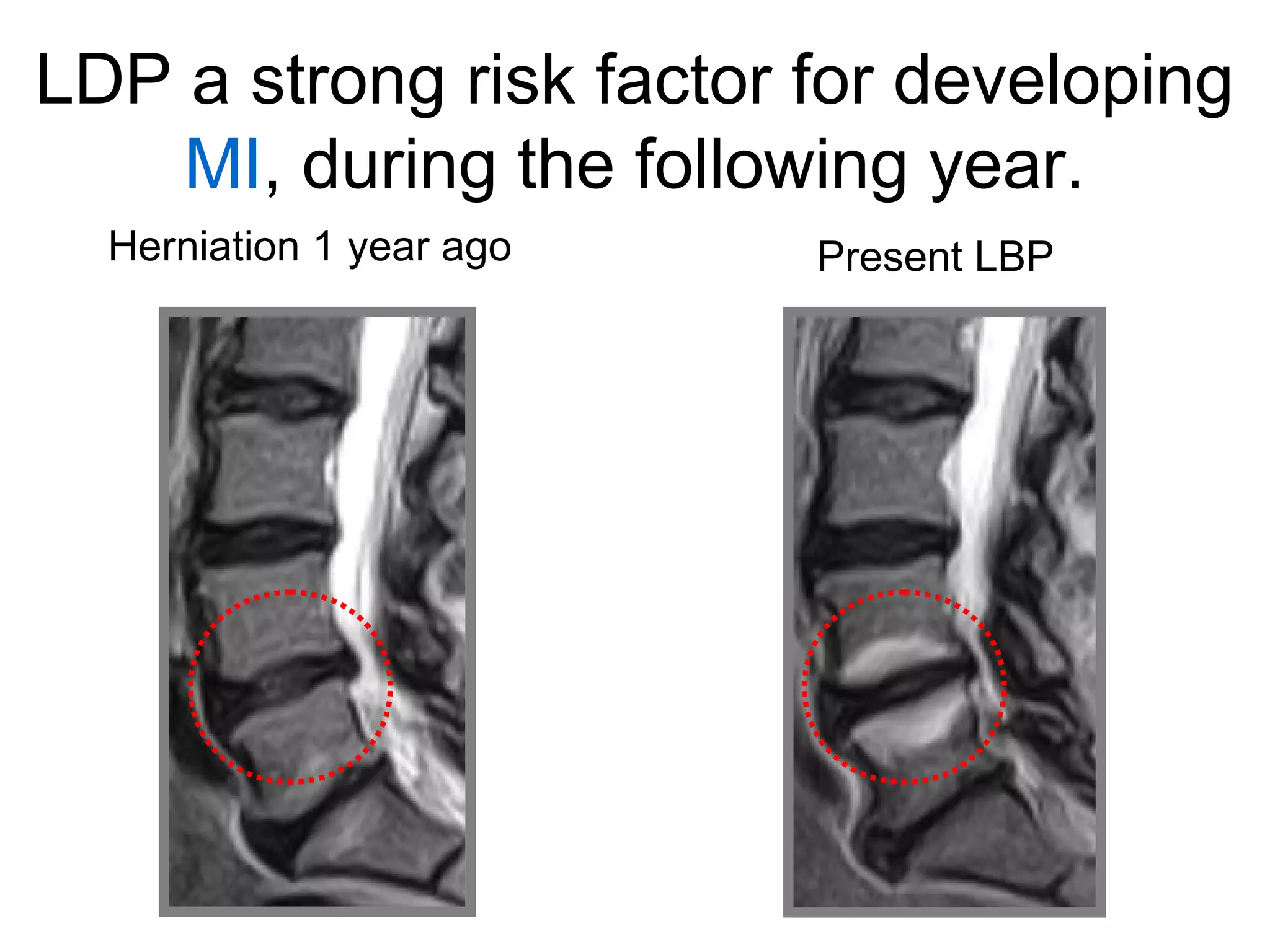
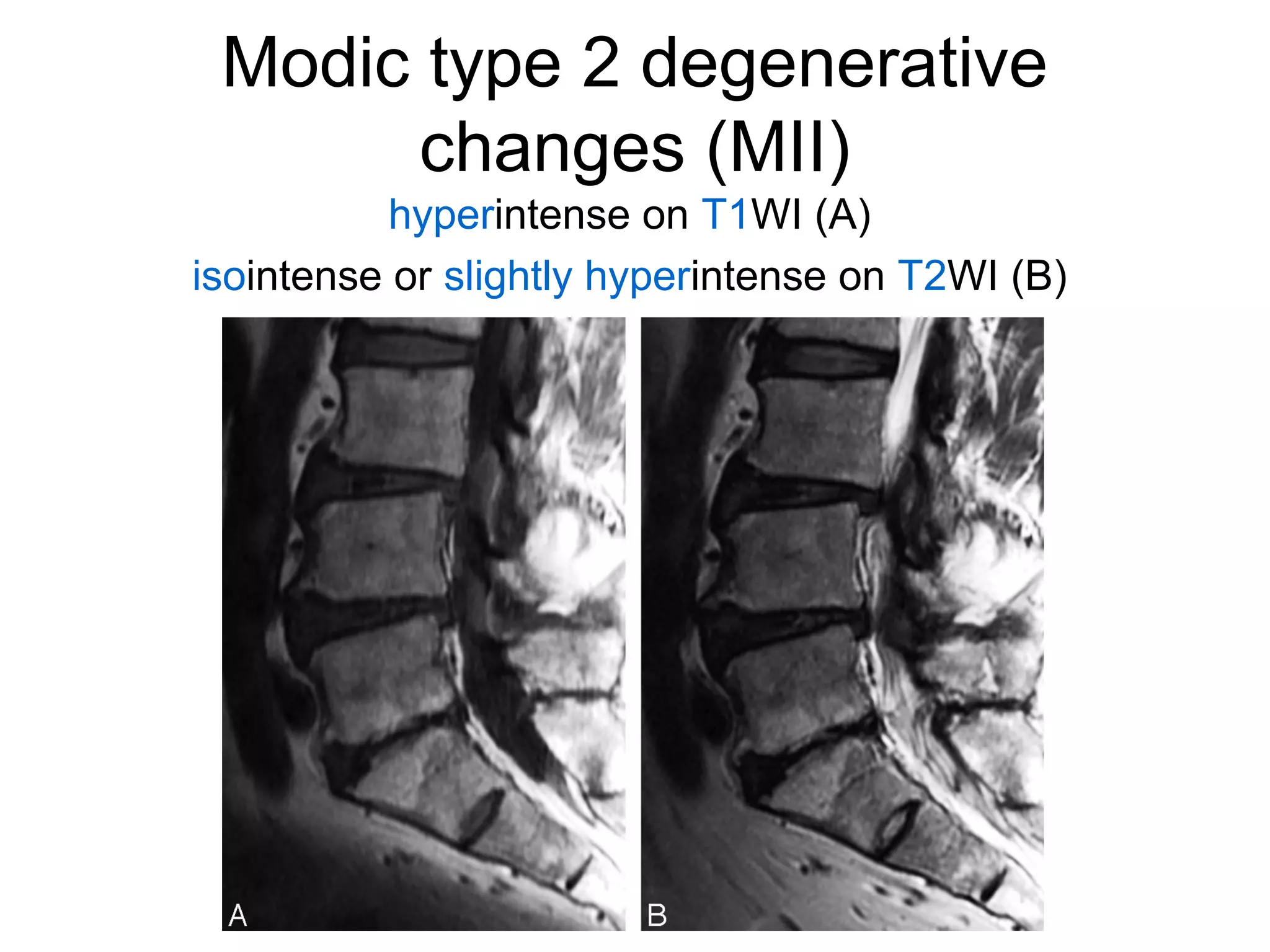
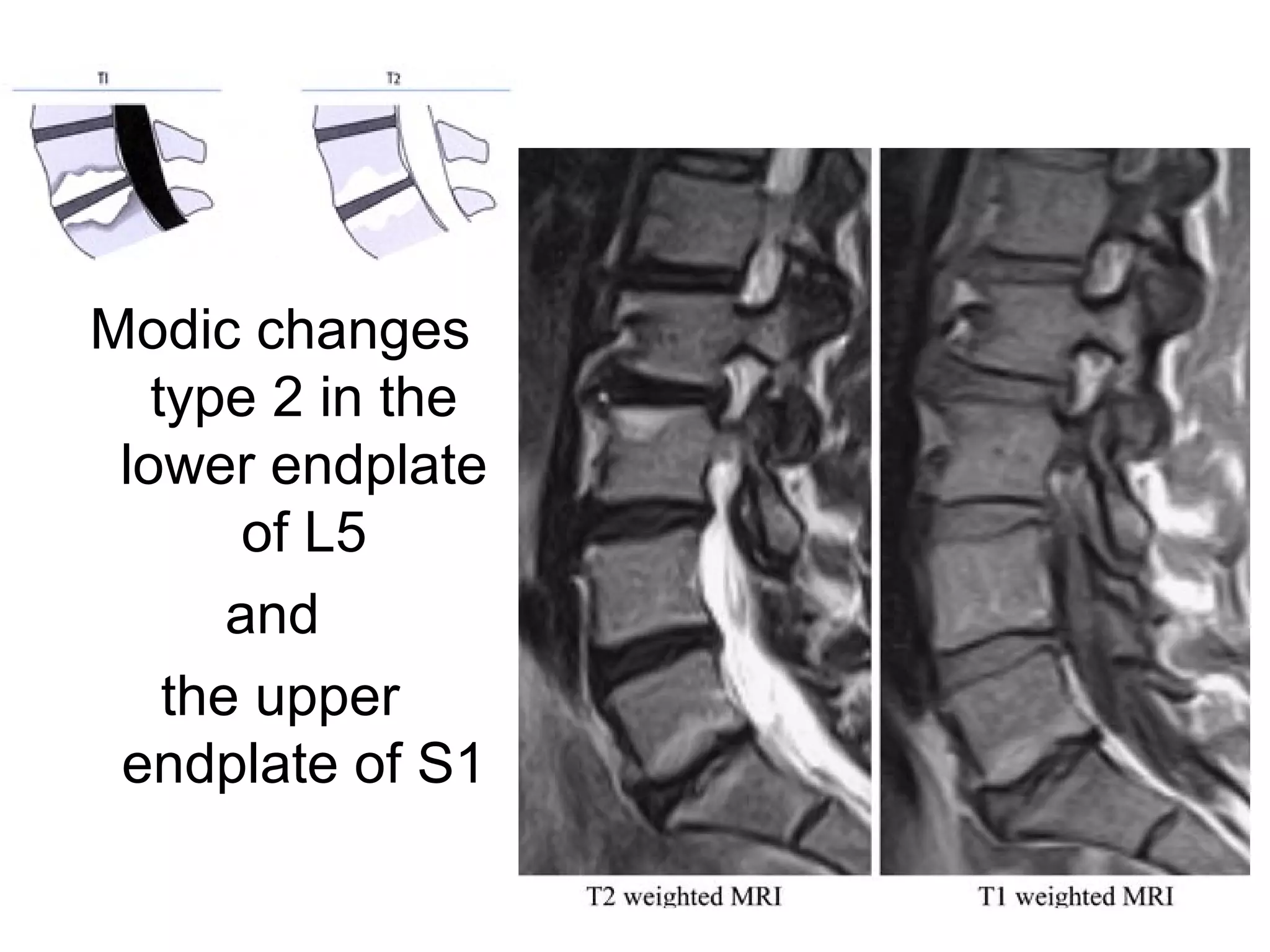
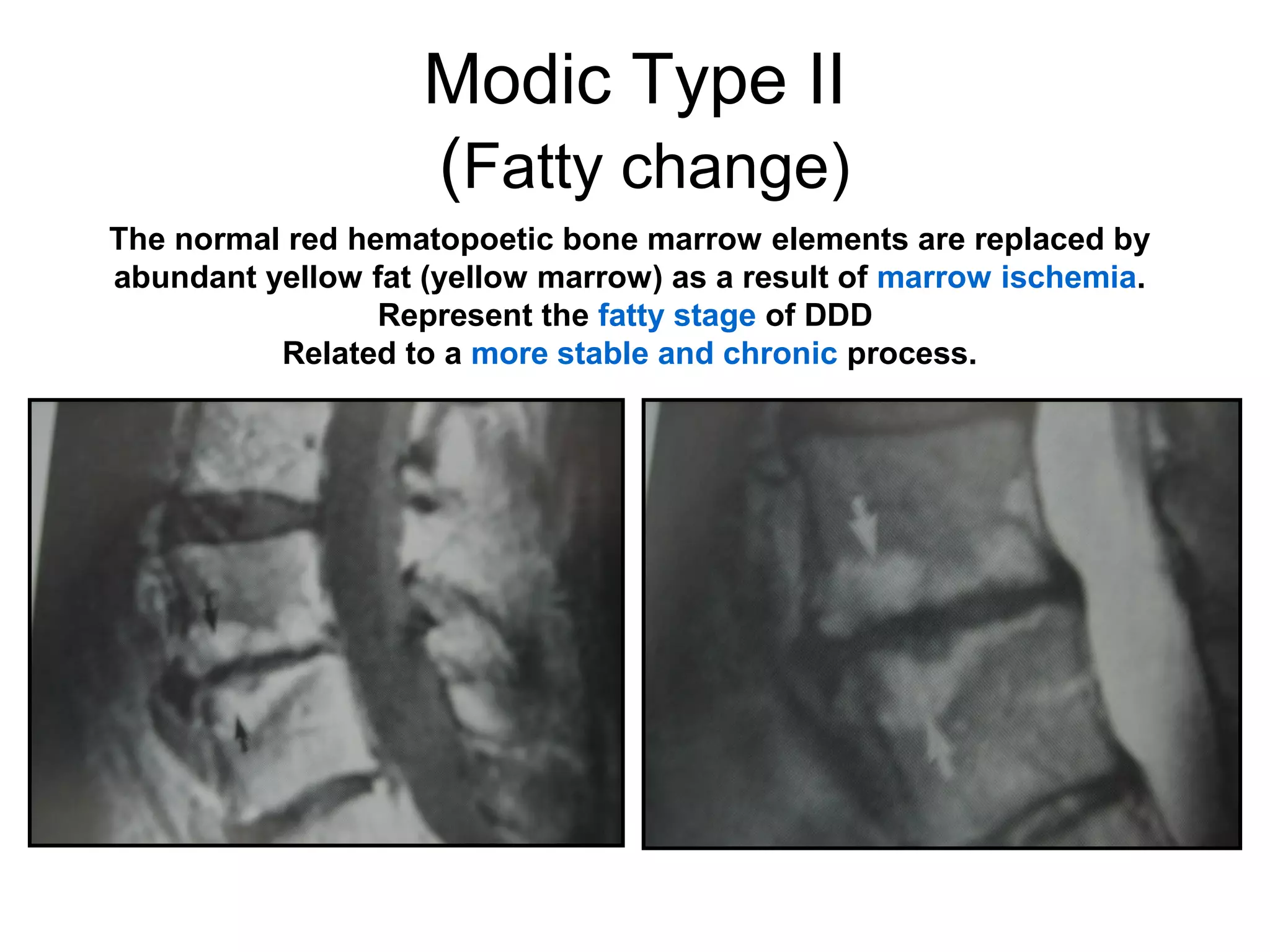
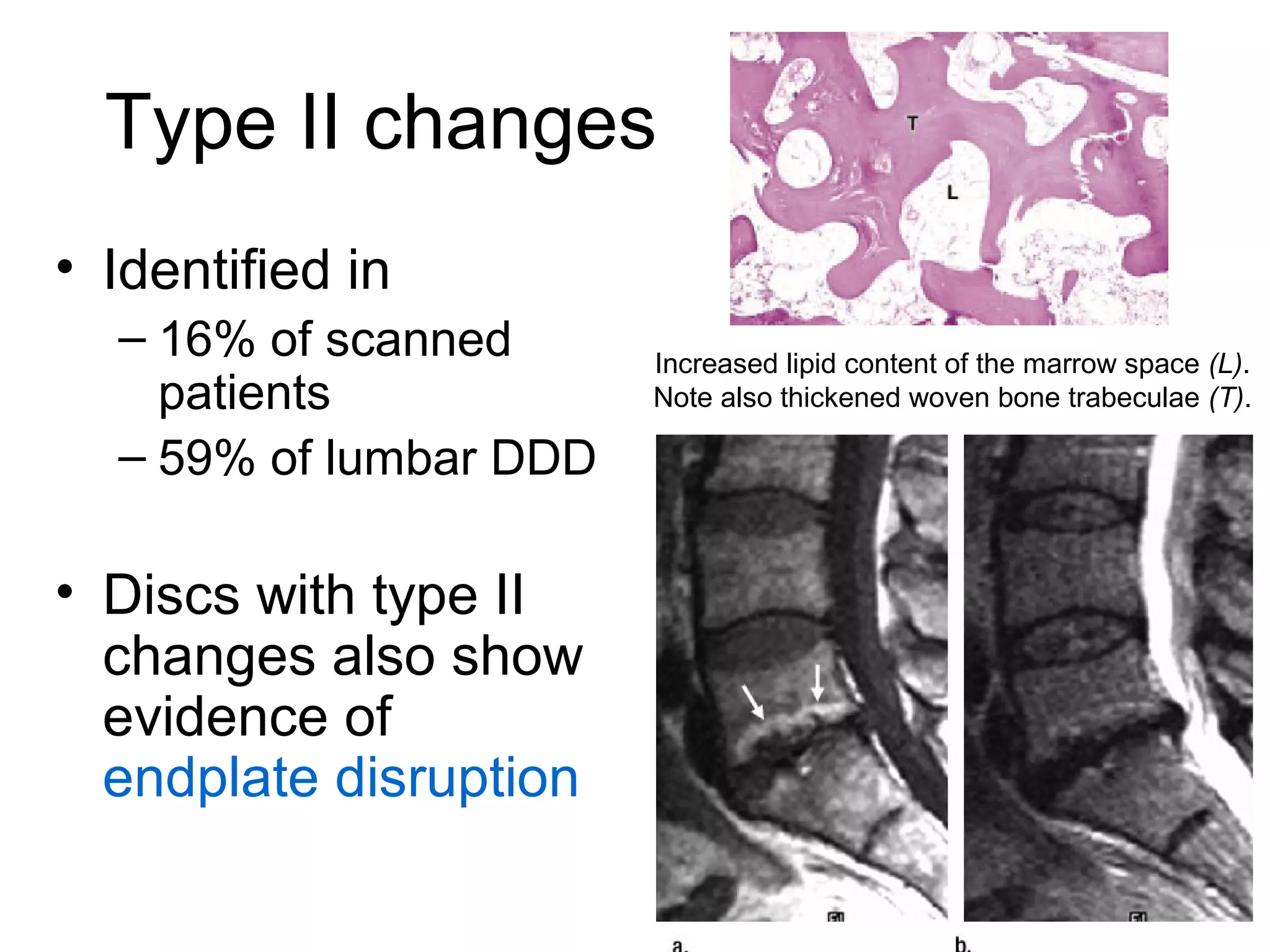
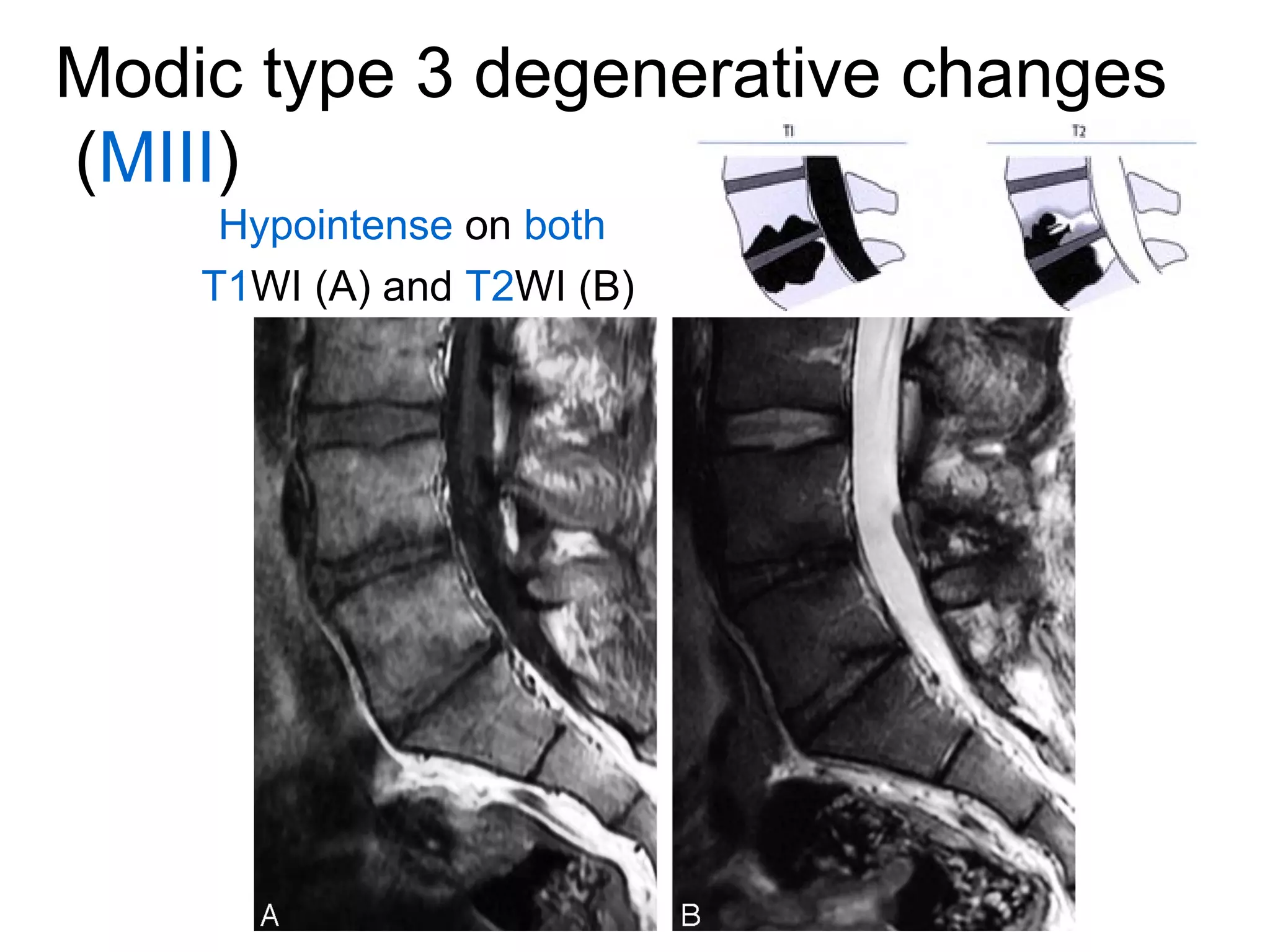
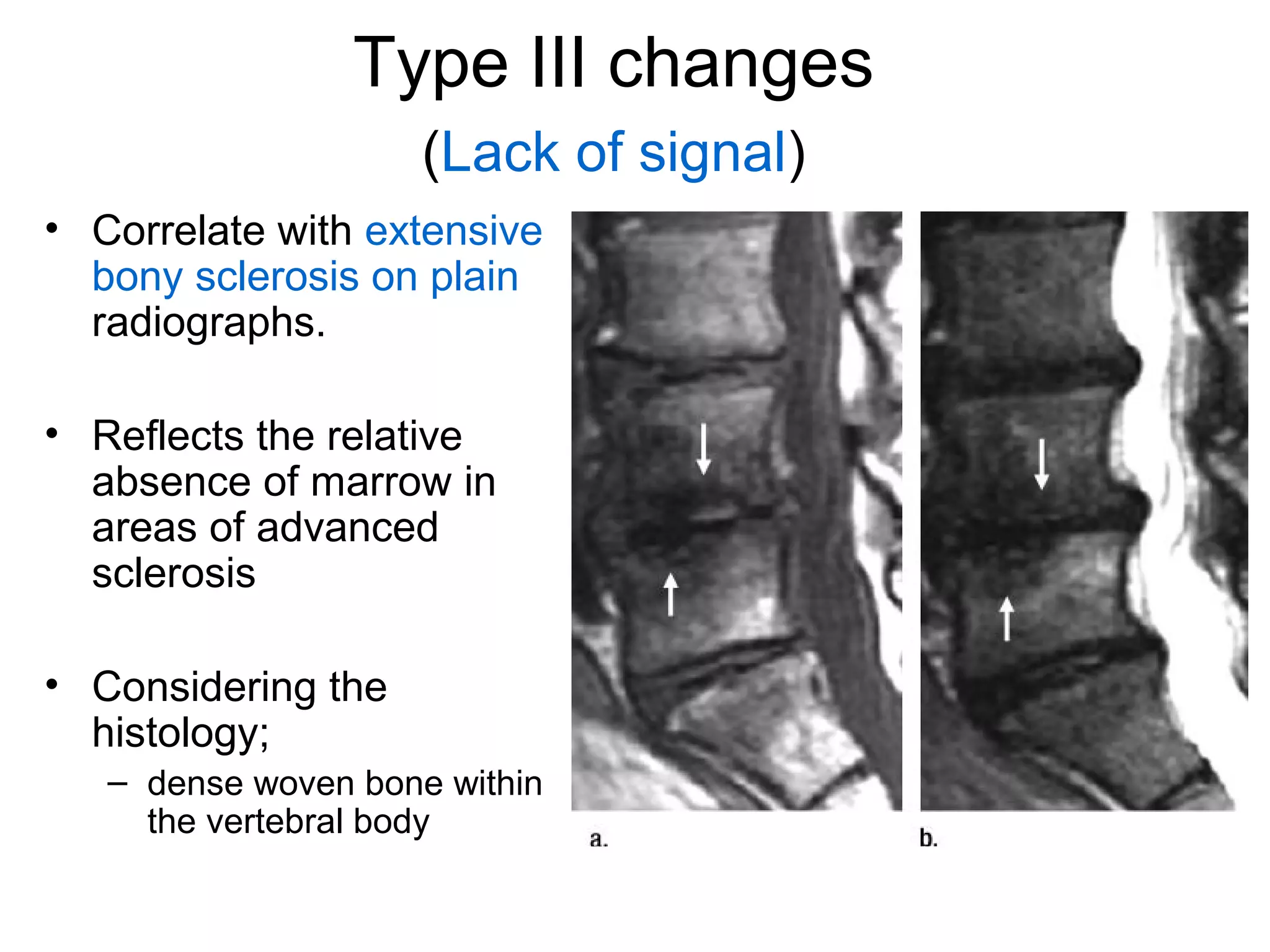
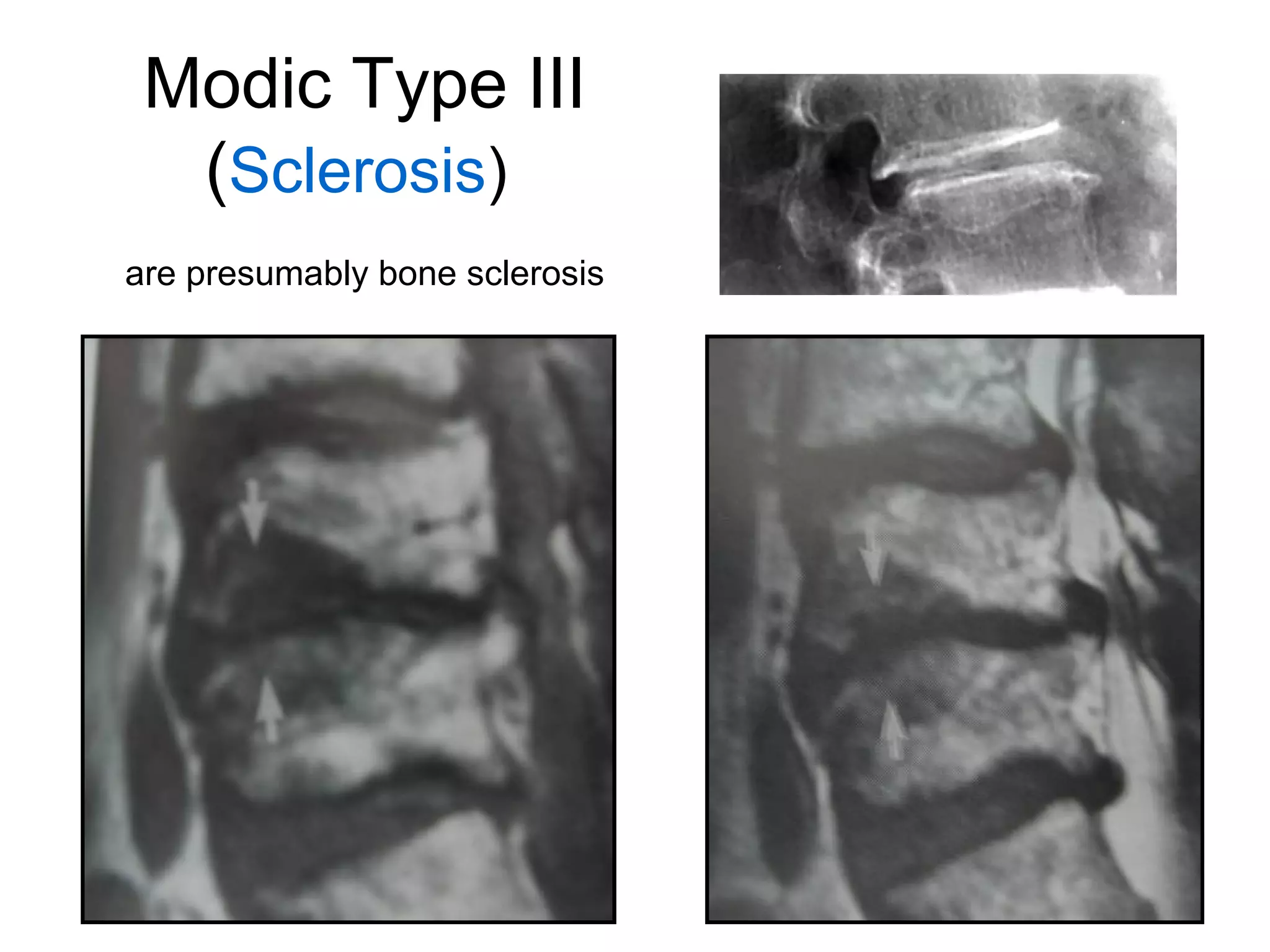
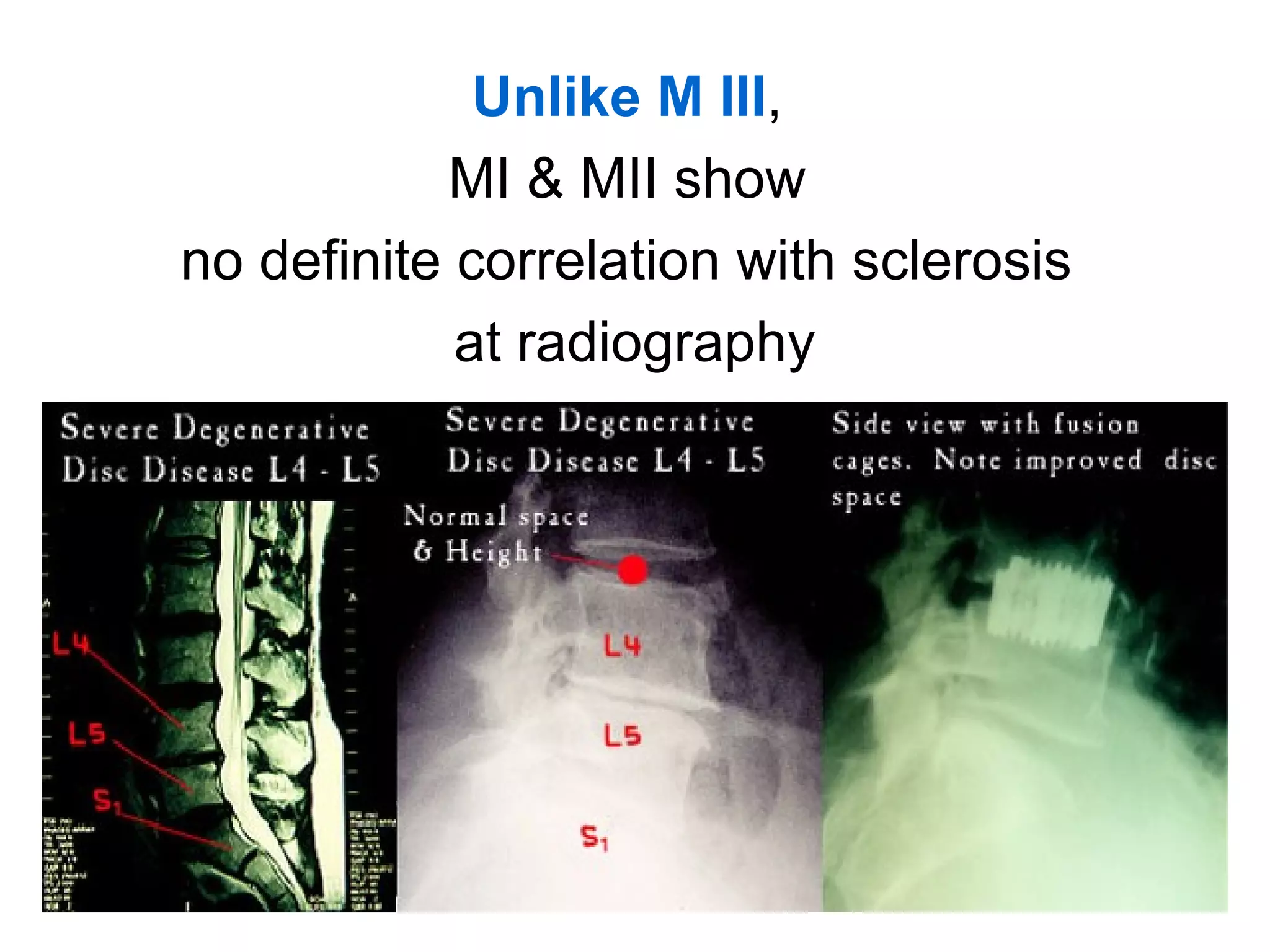
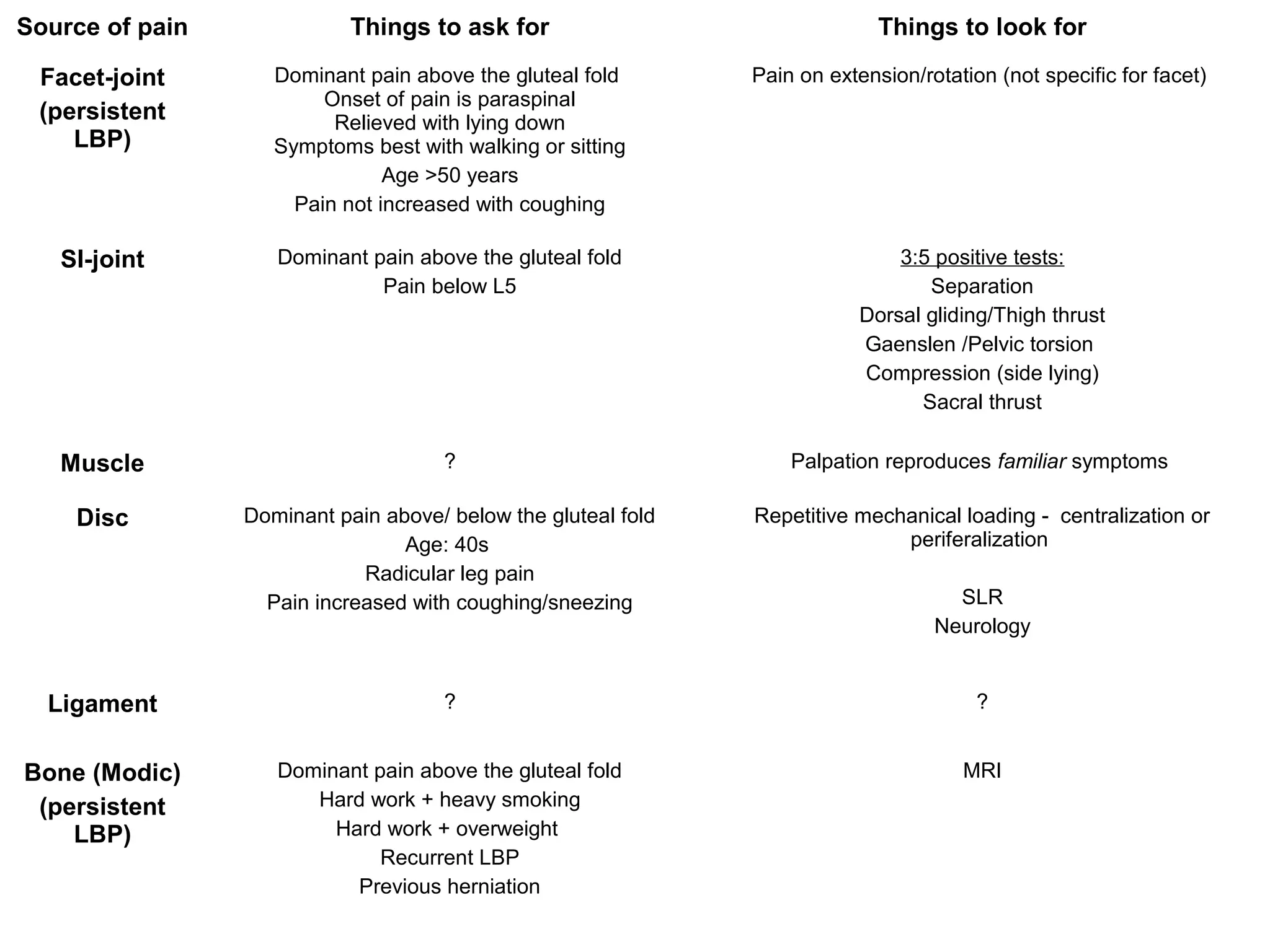
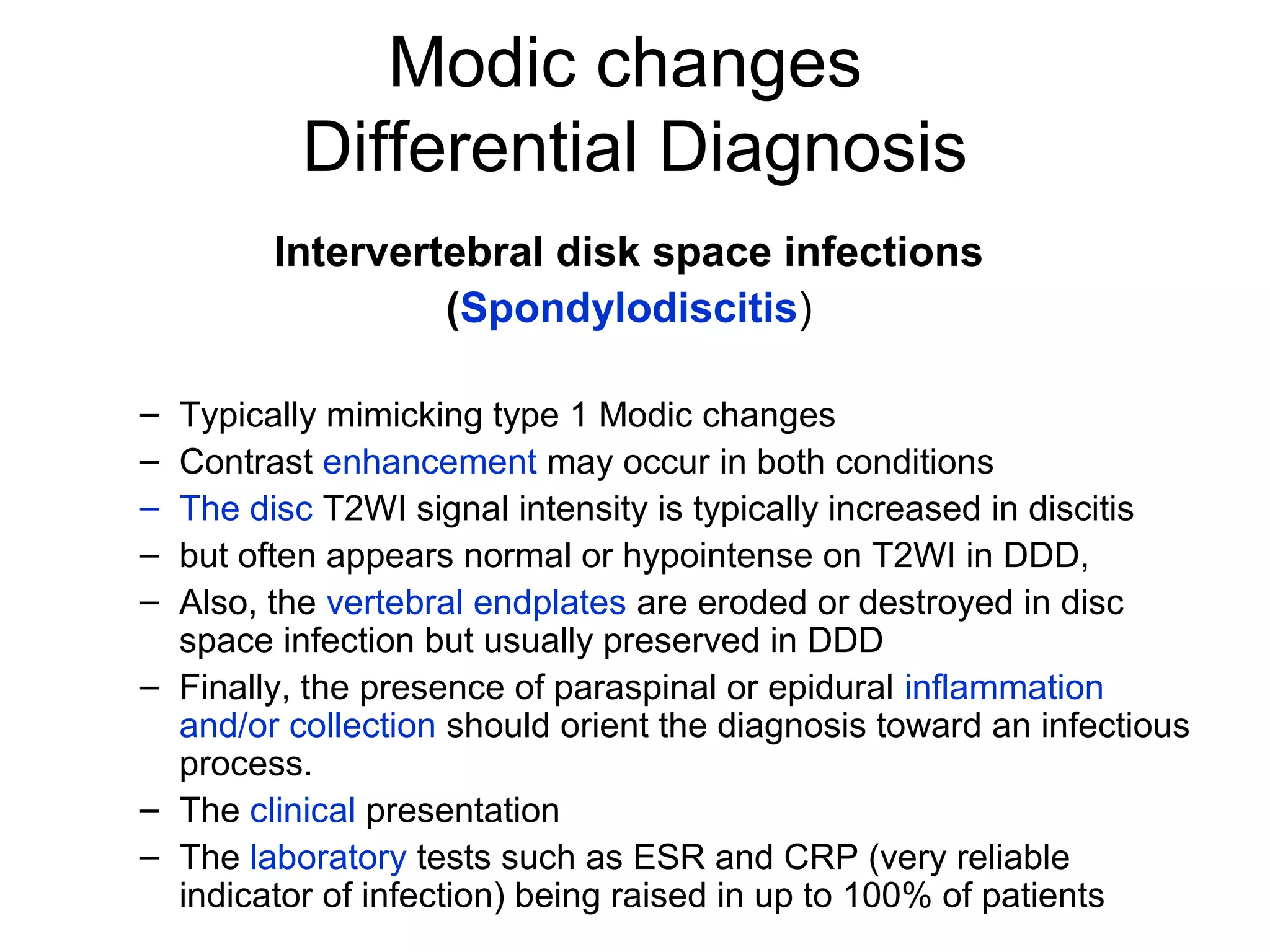
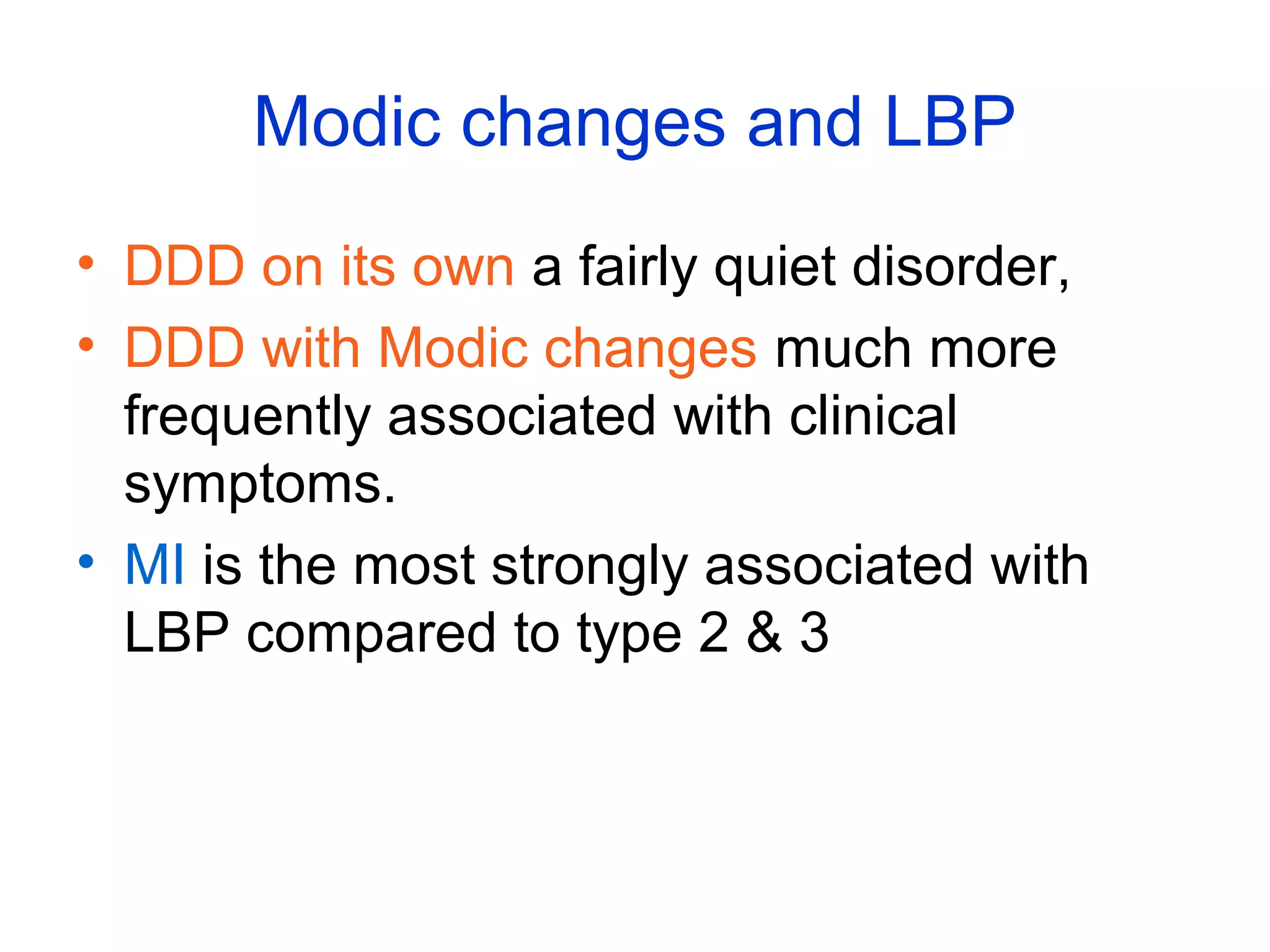
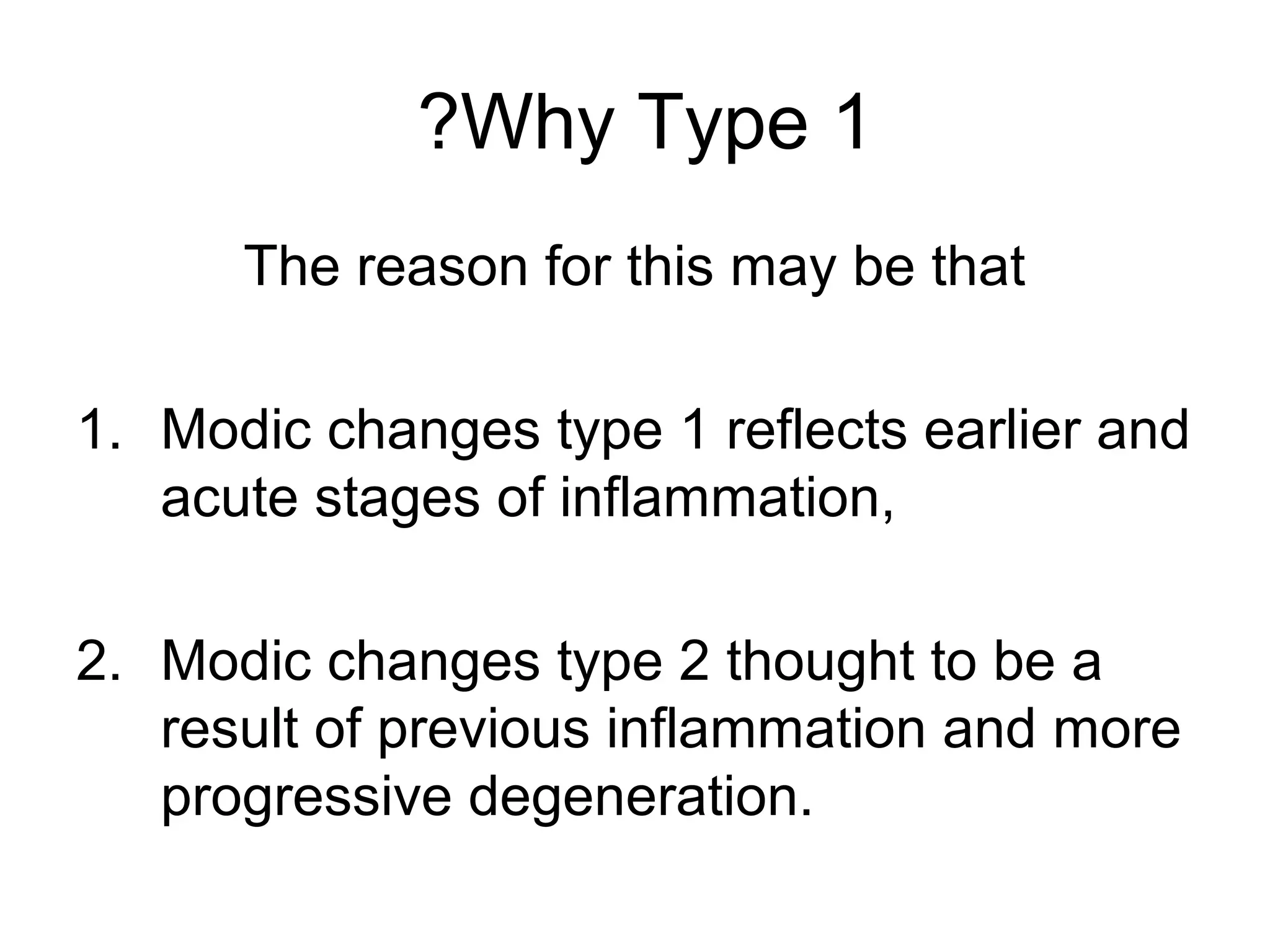
The document discusses Modic changes in vertebral endplates, classifying them into three types based on MRI signal intensity and their correlation with degenerative disc disease (DDD) and low back pain (LBP). Type 1 changes are associated with inflammatory processes, while Type 2 changes represent a chronic stage with fatty degeneration, and Type 3 indicates advanced sclerosis. It emphasizes the dynamic nature of these changes and their potential link to ongoing instability and surgical outcomes in patients with LBP.
![The reasons why Modic changes
may be painful are not known
• the pain may originate from damaged endplates in
patients with VESC.
– The lumbar vertebral endplate contains immunoreactive nerves,
– increased number of tumour necrosis factor (TNF)
immunoreactive nerve cells and fibres are present in endplates
that have VESC, especially in type 1 changes [111]. Therefore,
• a positive correlation between the presence and extent
of Modic changes and the amount of cartilage in the
extruded disk in patients undergoing lumbar
microdiskectomy and concluded that these changes may
result from avulsion-type disk herniation.](https://image.slidesharecdn.com/themodicvertebralendplateandmarrowchangesspine2010-141002175548-phpapp01/75/The-modic-vertebral-endplate-and-marrow-changes-spine-2010-30-2048.jpg)