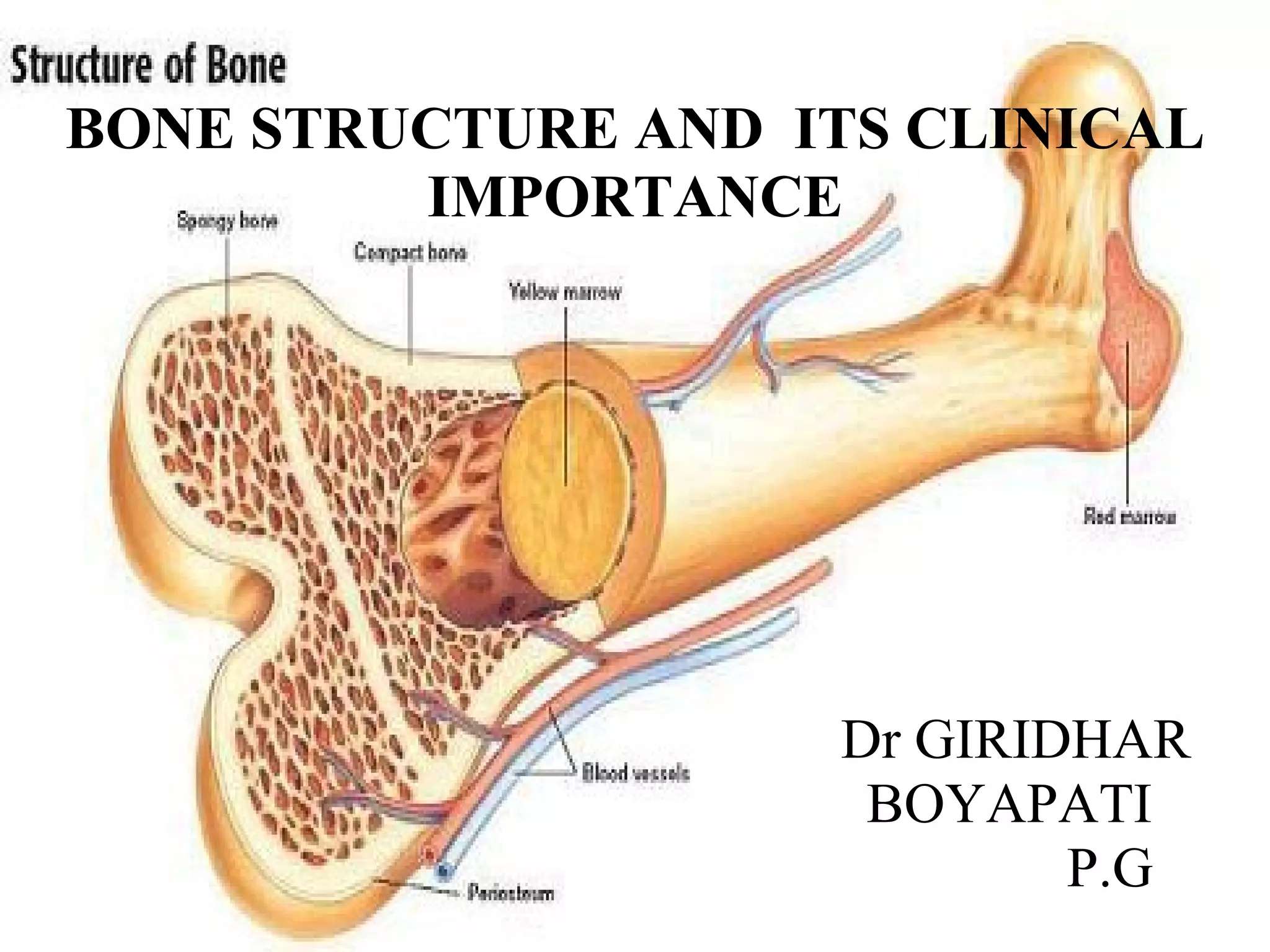
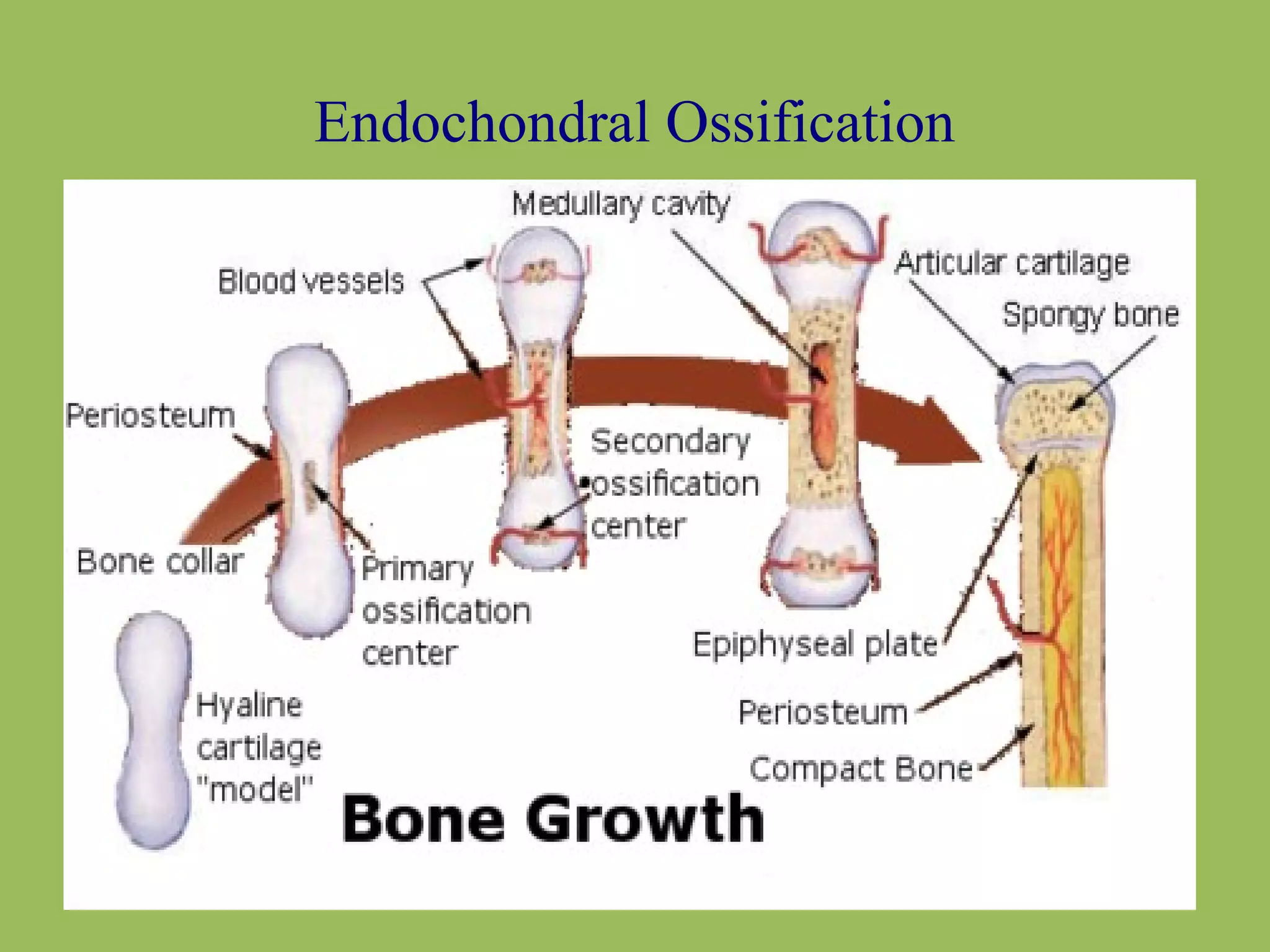
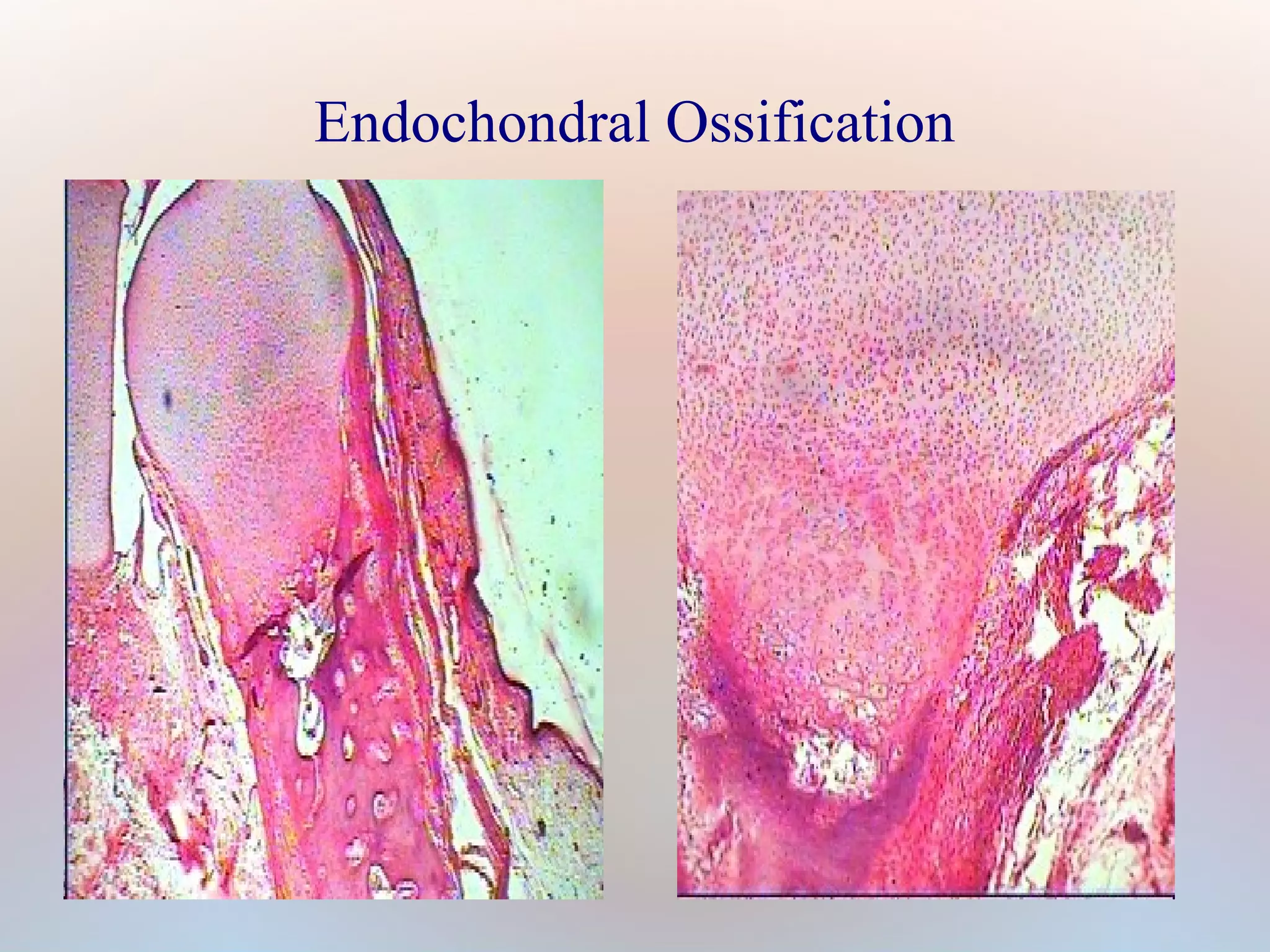
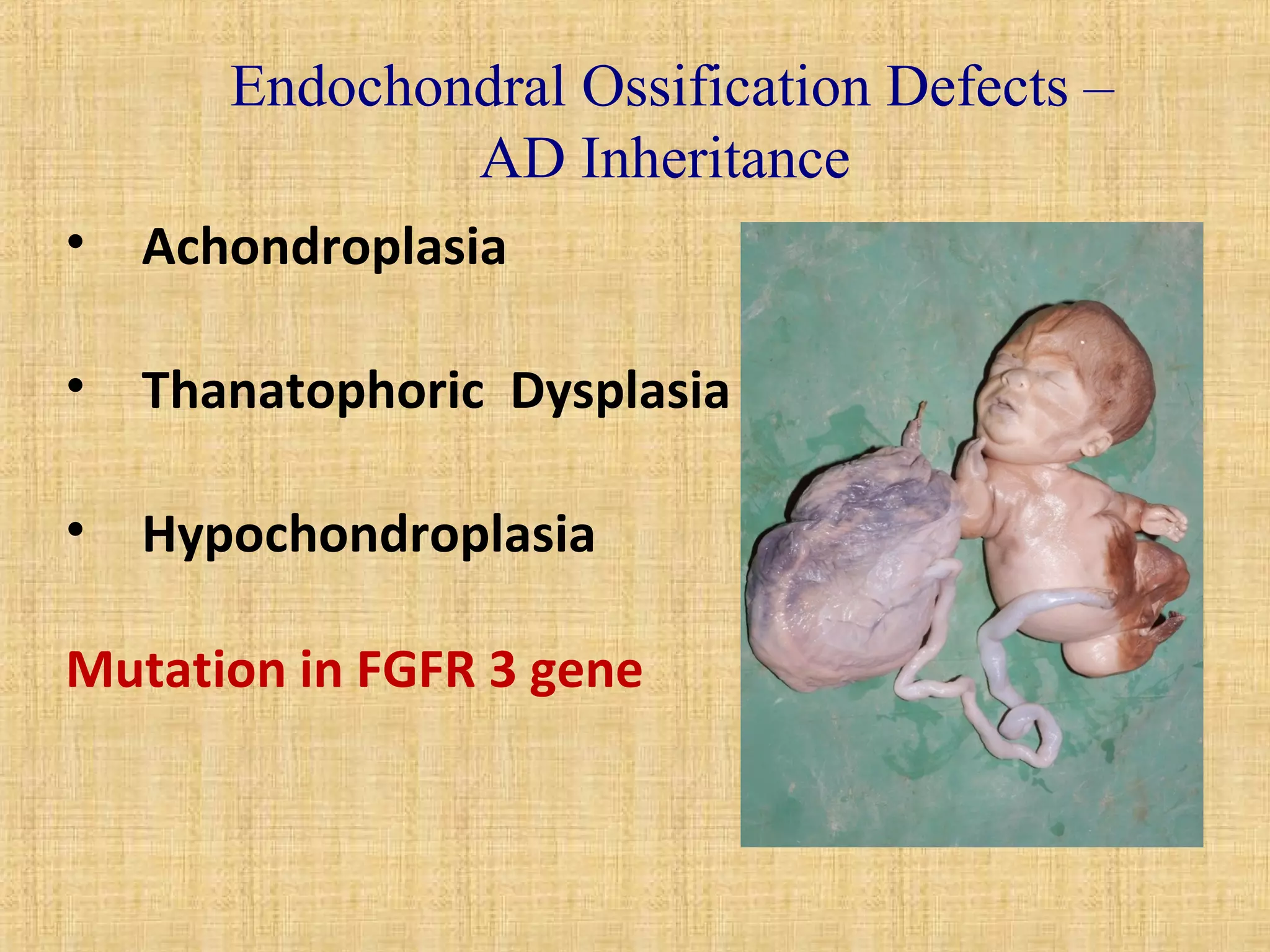
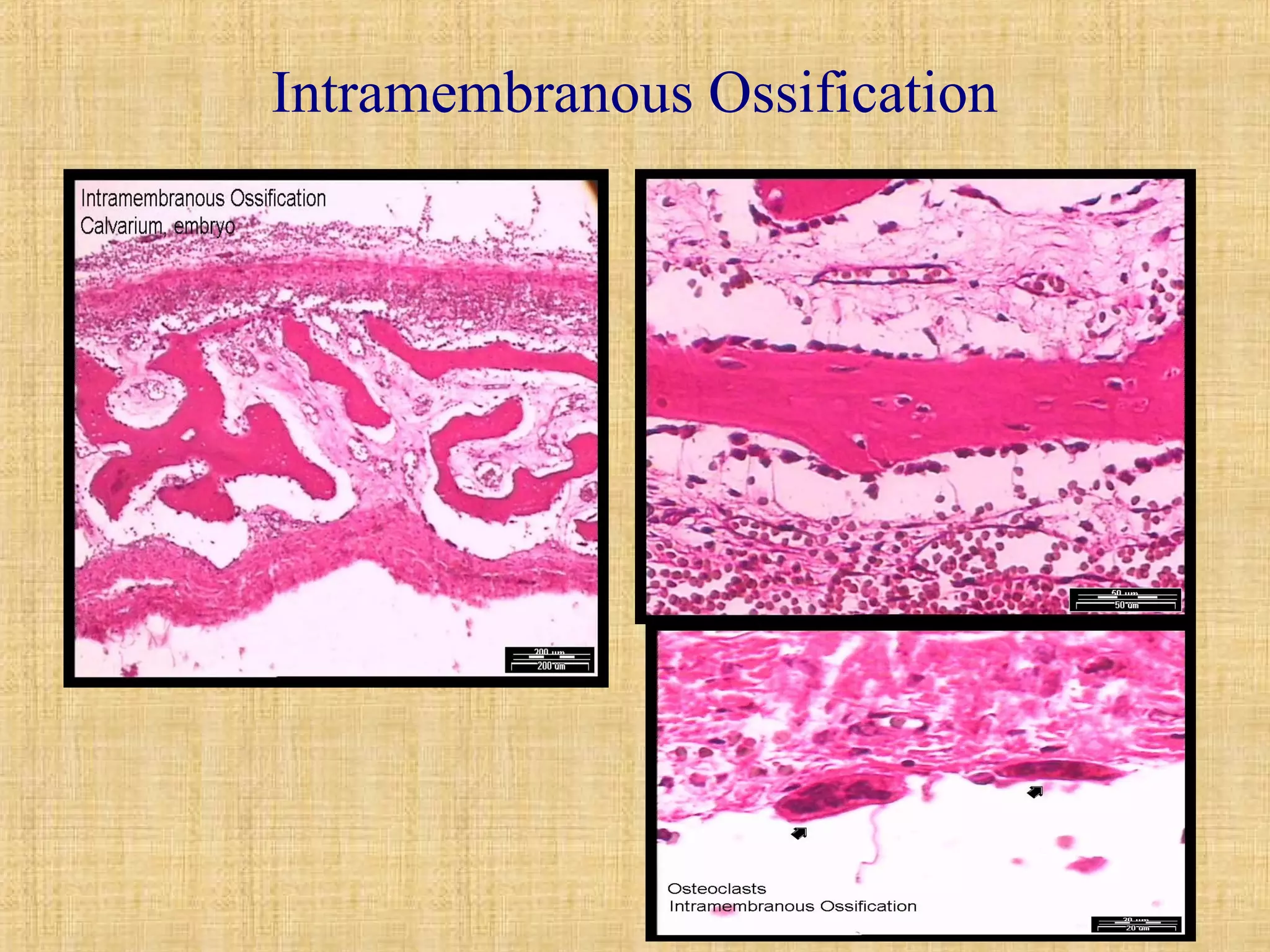
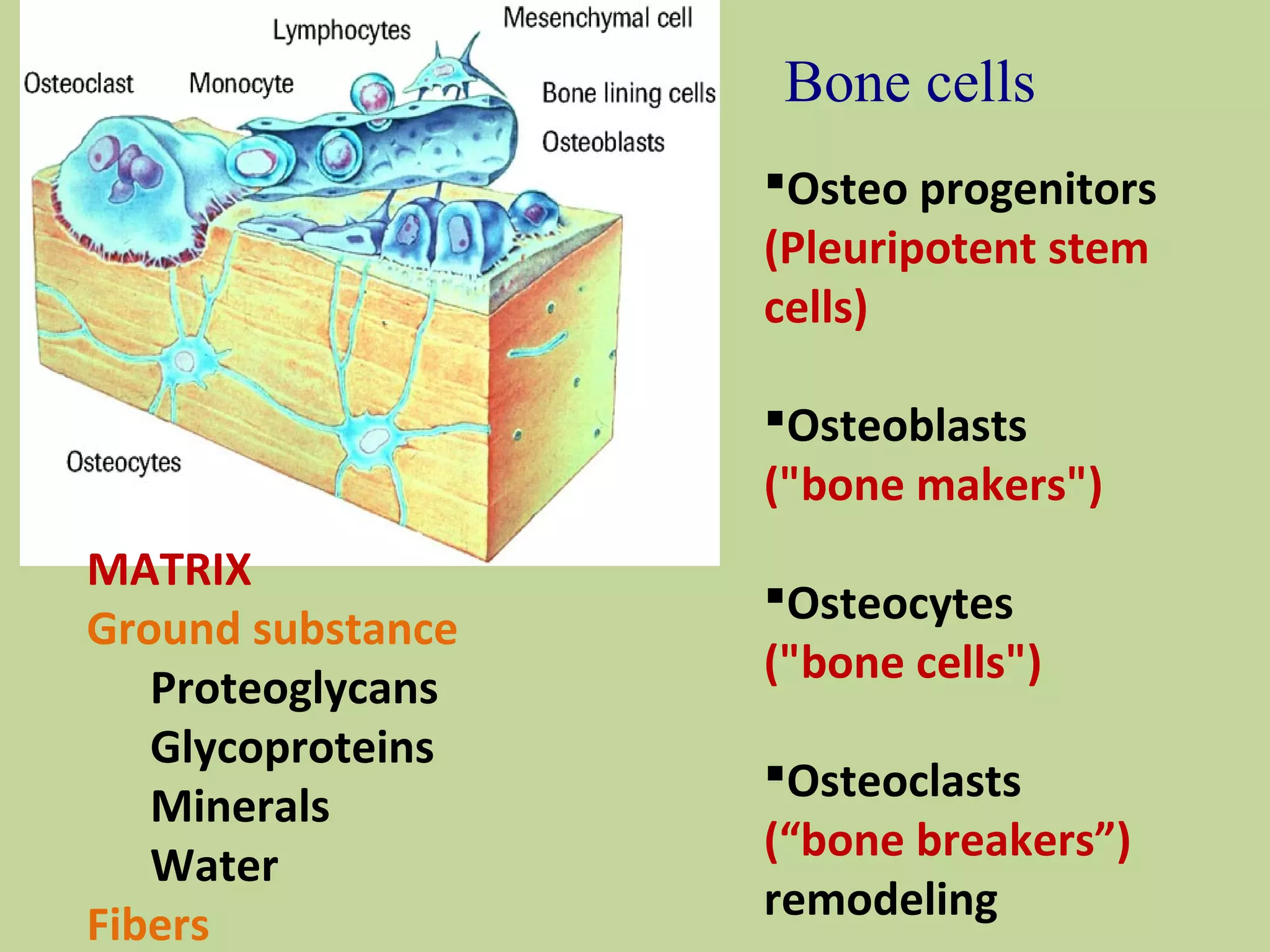
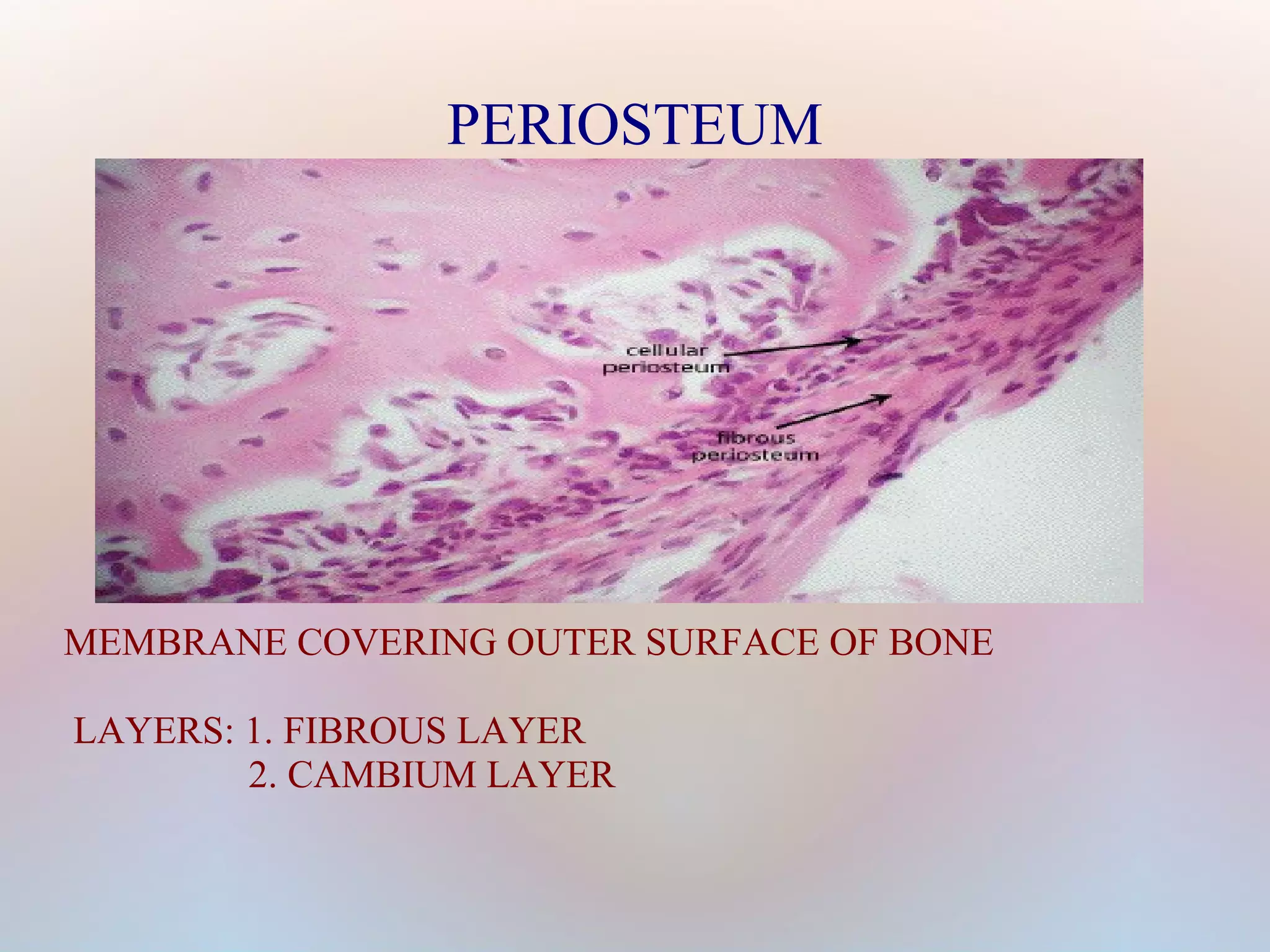
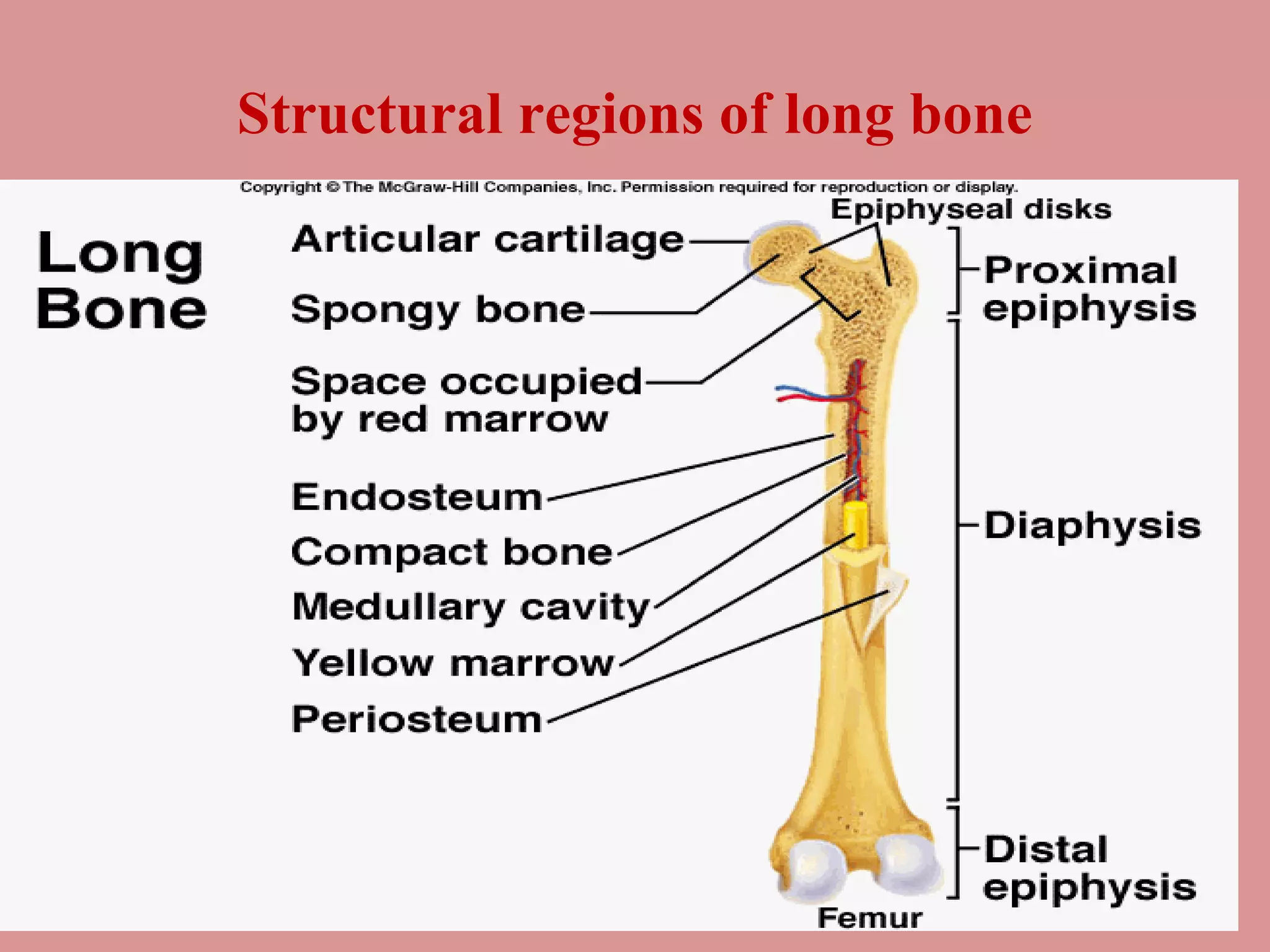
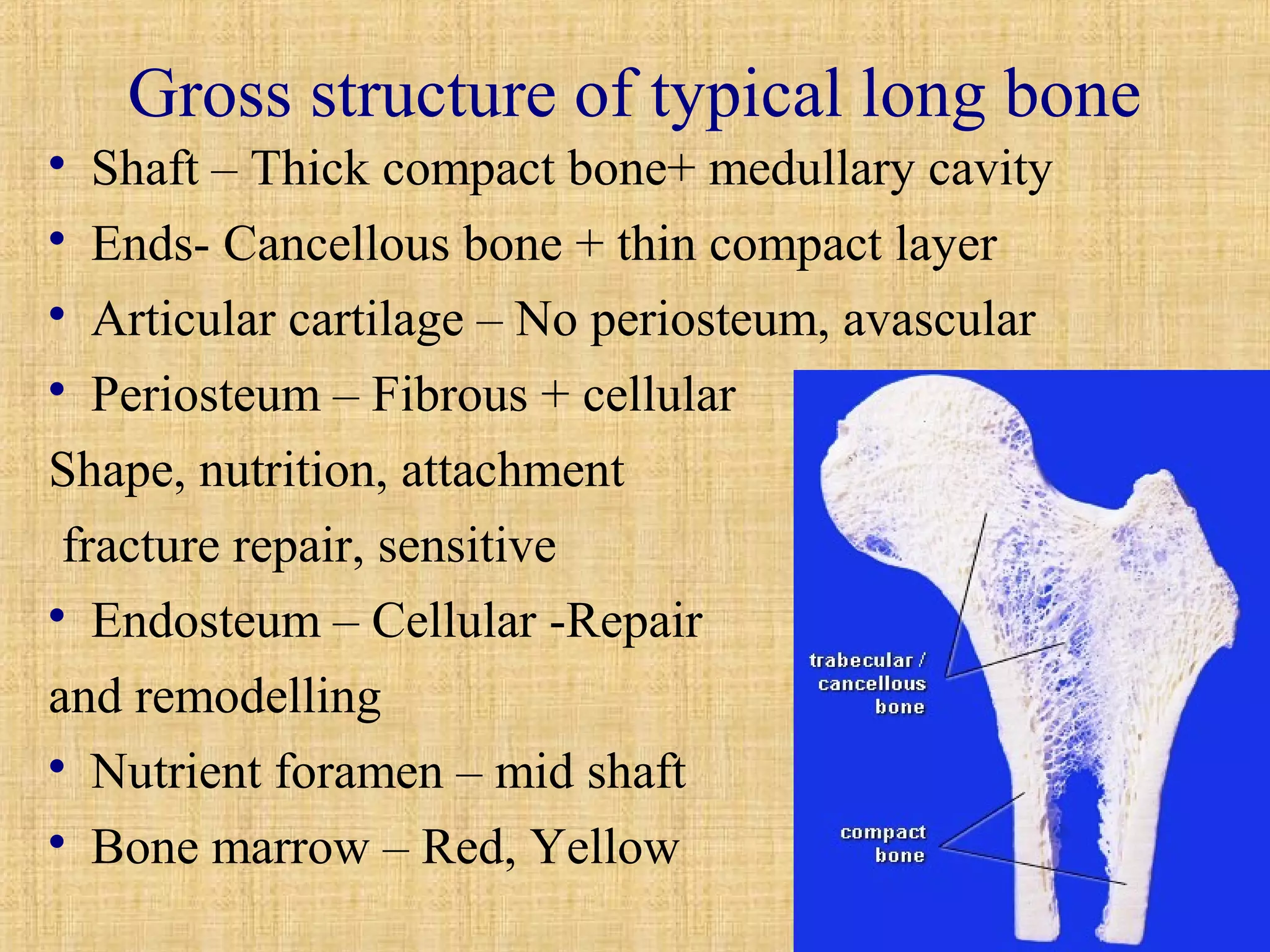
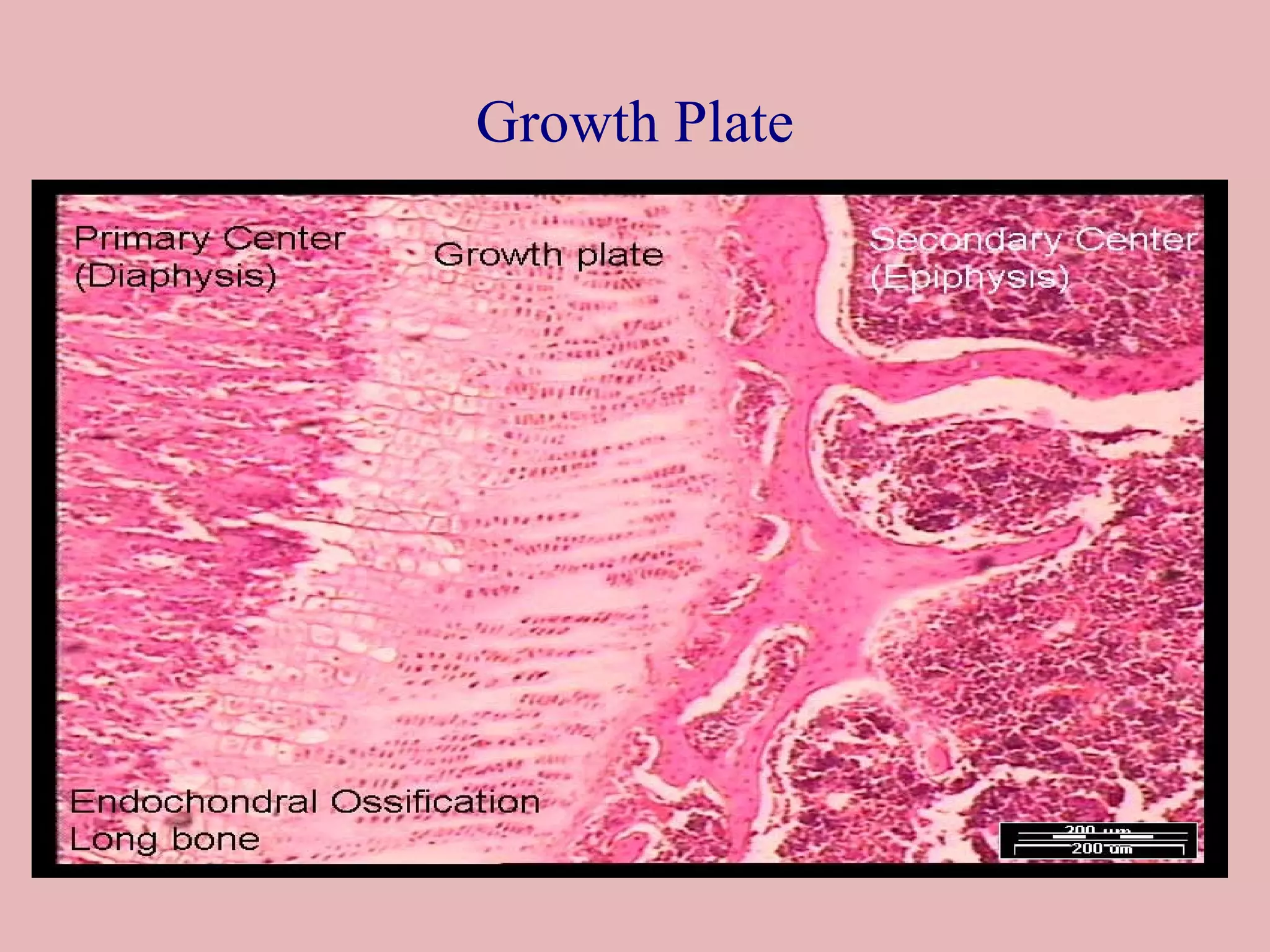
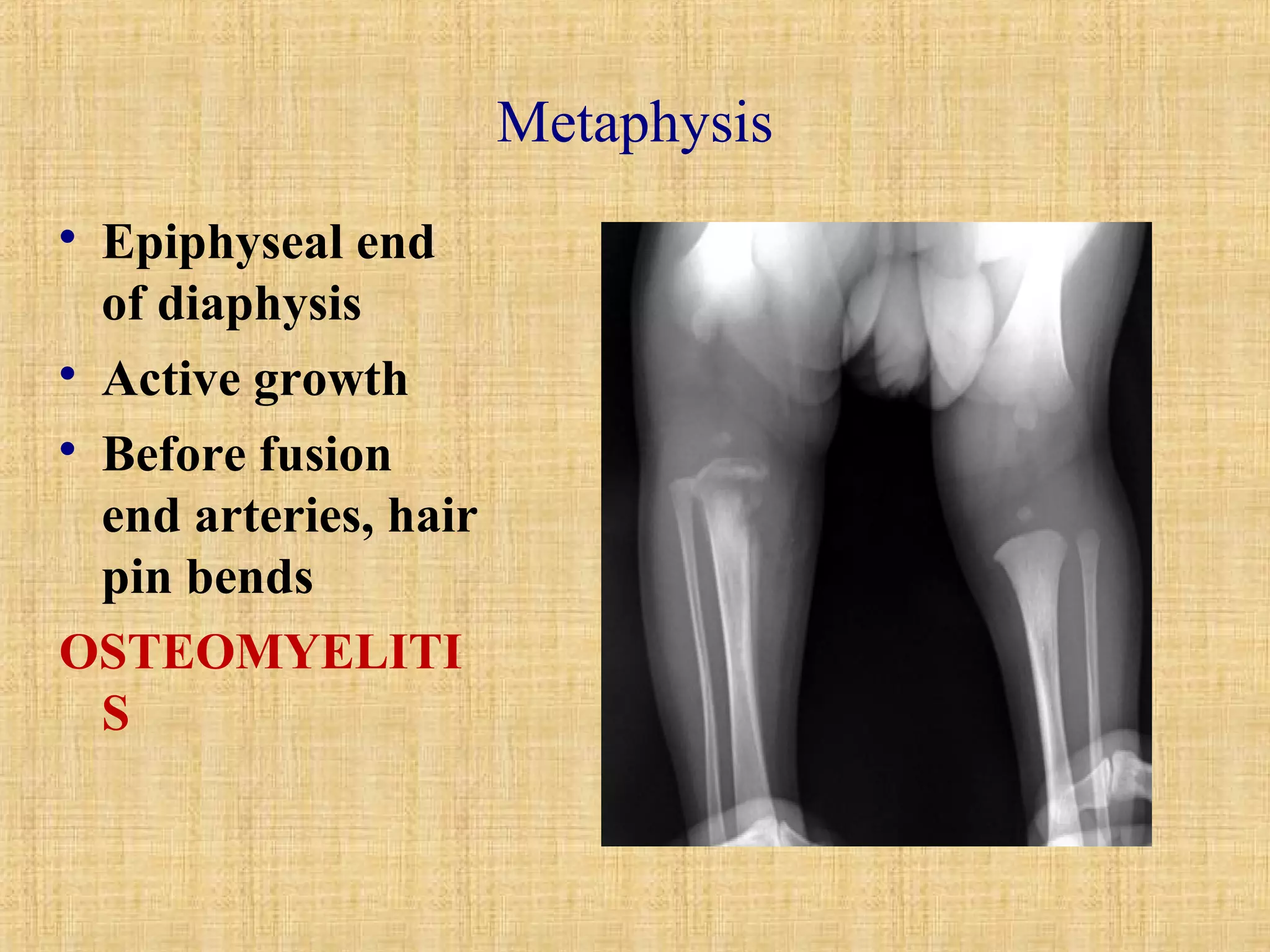
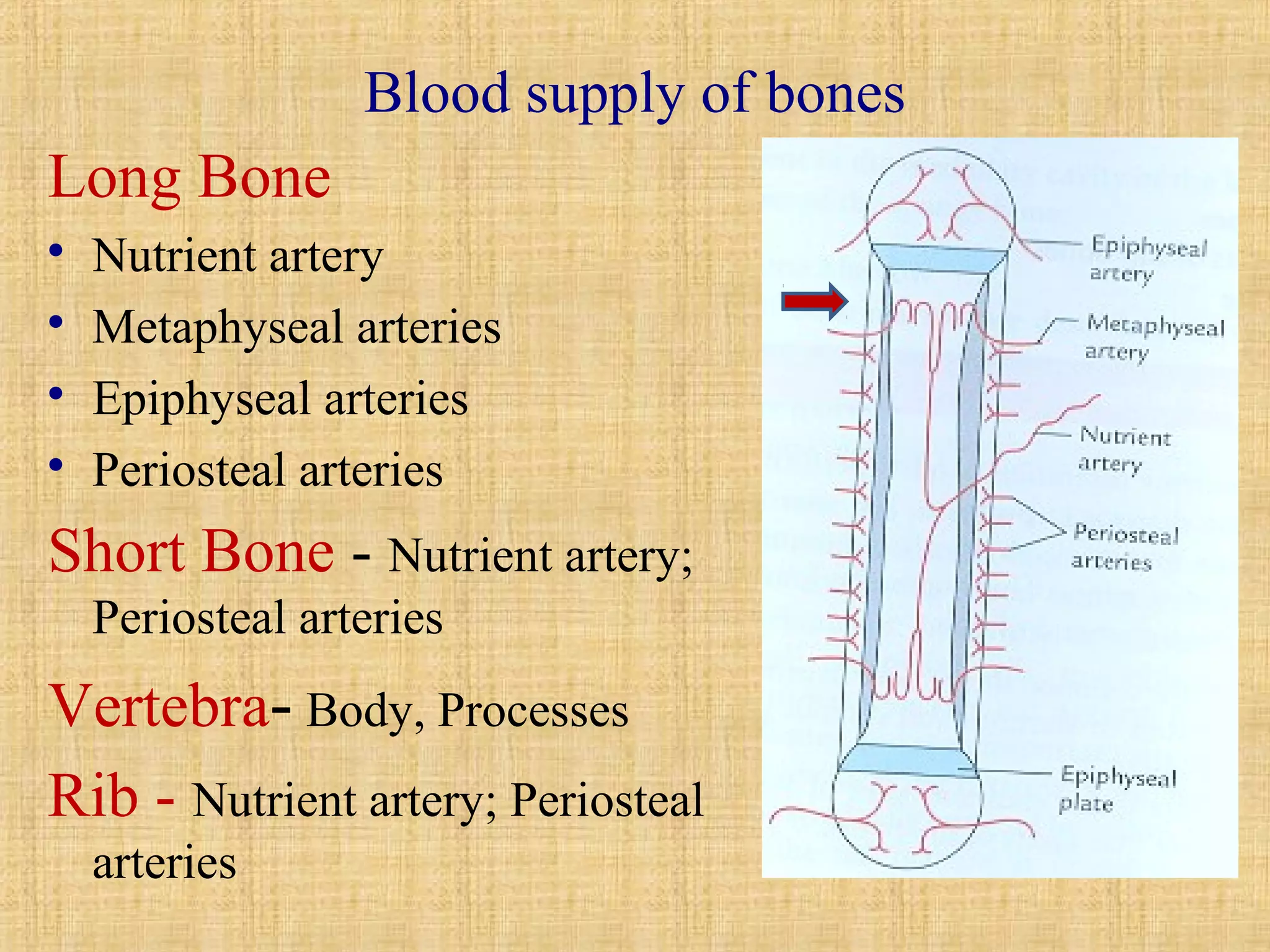
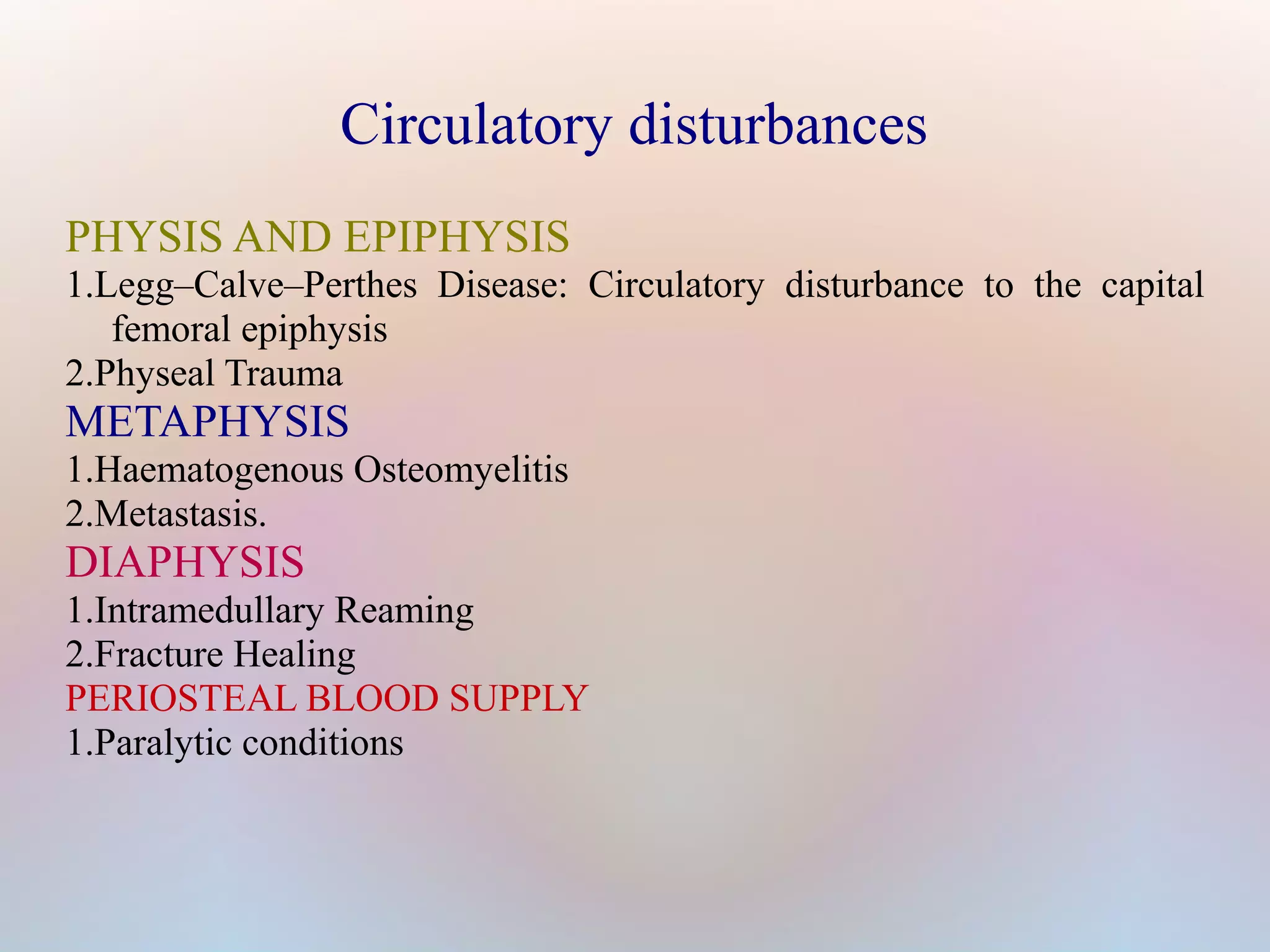
Bone is a mineralized connective tissue that forms the endoskeleton of vertebrates. It has both compact and spongy structures and develops through either membranous or endochondral ossification. Bone is made up of osteoprogenitor cells, osteoblasts, osteocytes, and osteoclasts. Osteoblasts form new bone tissue while osteoclasts resorb old or damaged bone. The intricate blood supply through nutrient arteries is essential for bone growth and healing. Fractures heal through the formation of a hematoma, fibrocartilaginous callus, bony callus, and remodeling into secondary bone.