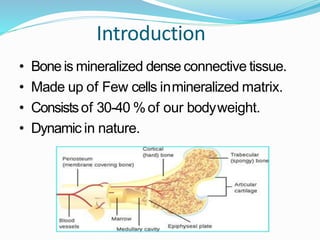
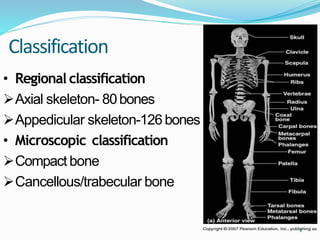
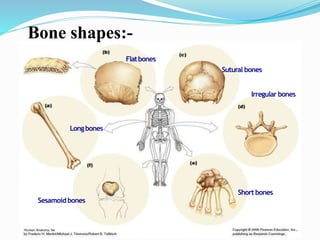
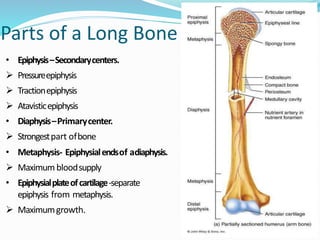
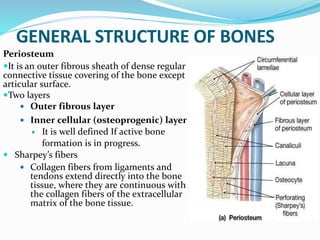
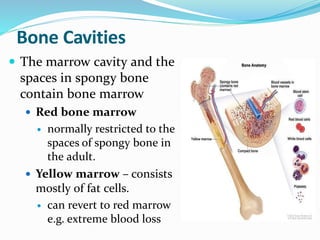
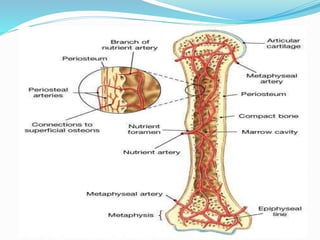
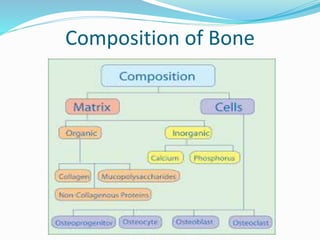
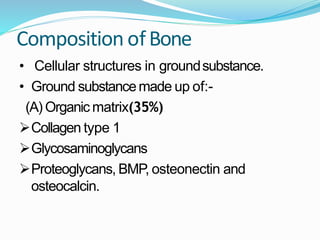
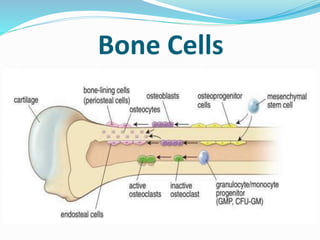
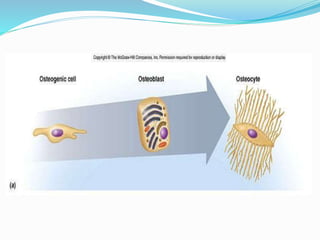
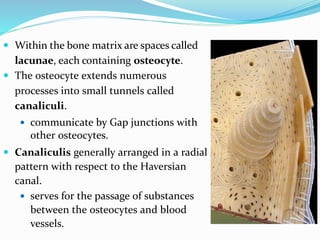
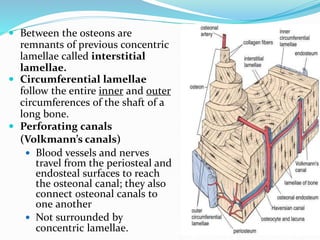
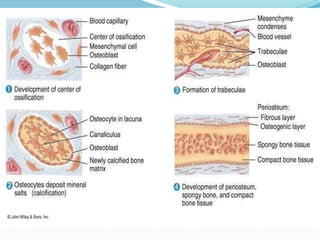
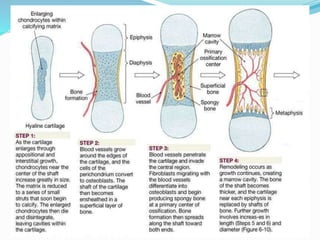
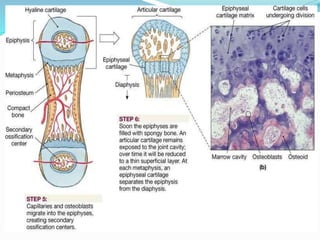
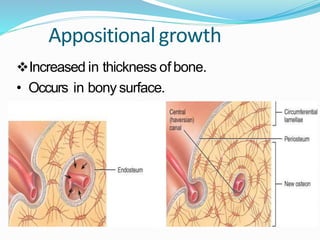
The document provides a comprehensive overview of bone structure, classification, and function, detailing its composition, types of bone cells, and the processes of bone formation. It explains the dynamic nature of bones, their roles in the body, and the microscopic architecture including the periosteum, marrow cavities, and various bone types. Additionally, it describes two primary methods of bone formation: intramembranous and endochondral ossification.