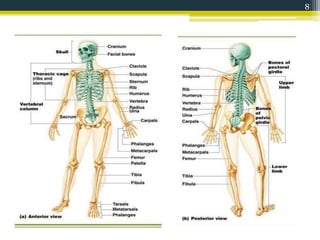
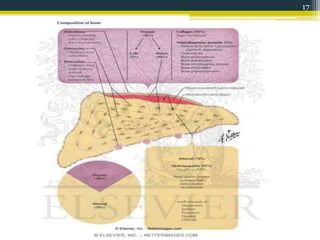
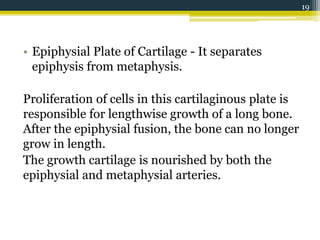
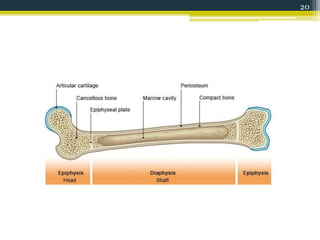
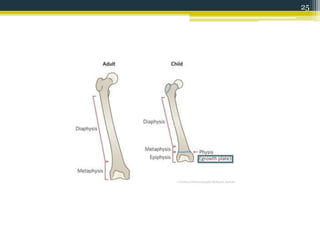
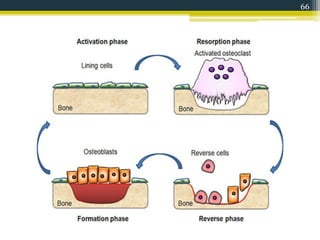
This document provides an overview of bone anatomy and physiology. It defines bone, describes its various functions, and classifications including by position, shape, development, and structure. The document discusses the composition of bone, including its organic and inorganic components. It describes the anatomy of bone including its blood and nerve supply. Finally, it provides details on the histology of bone, the different cell types involved in bone formation and resorption, and the processes of ossification and bone remodeling throughout life.