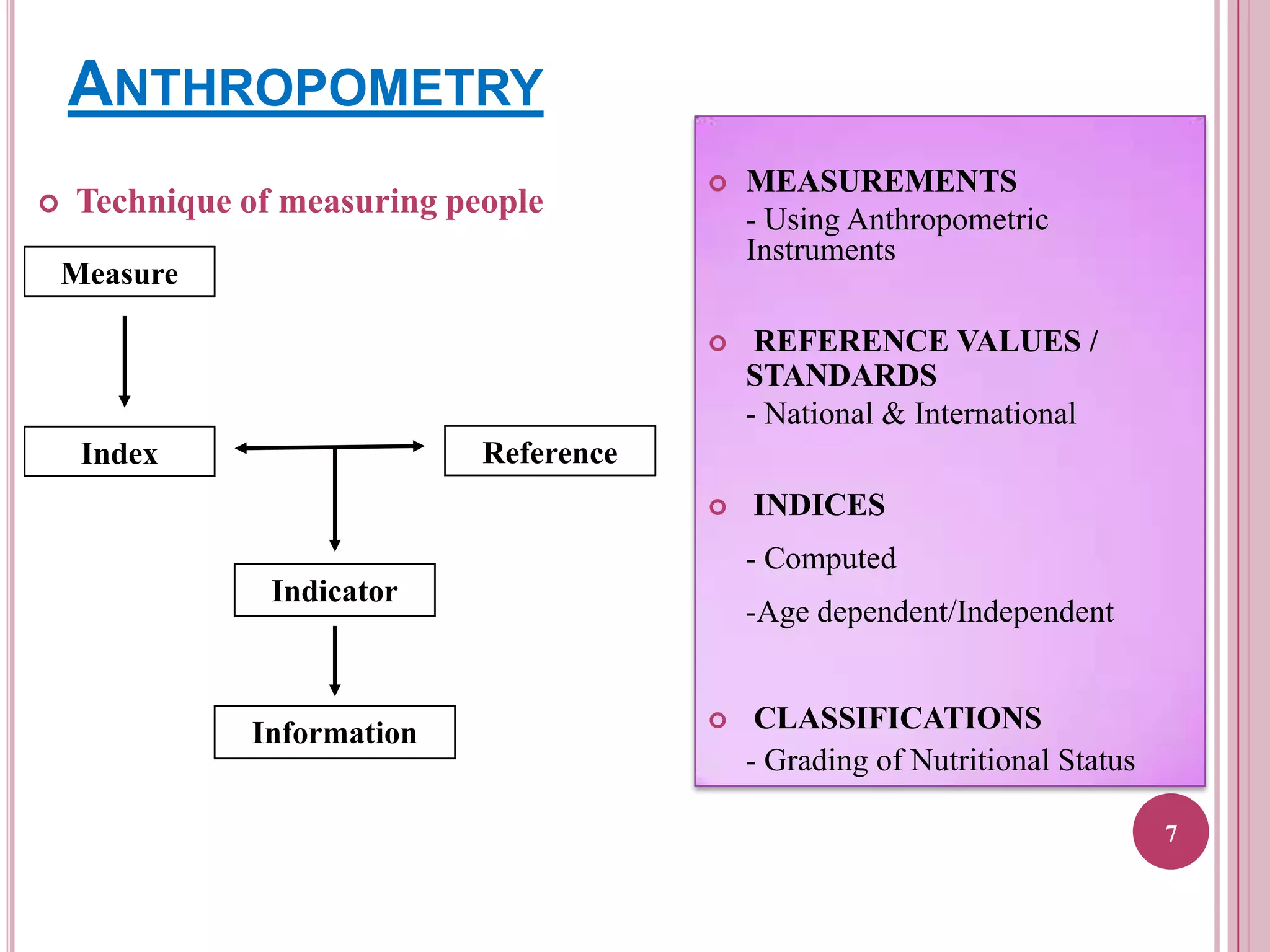
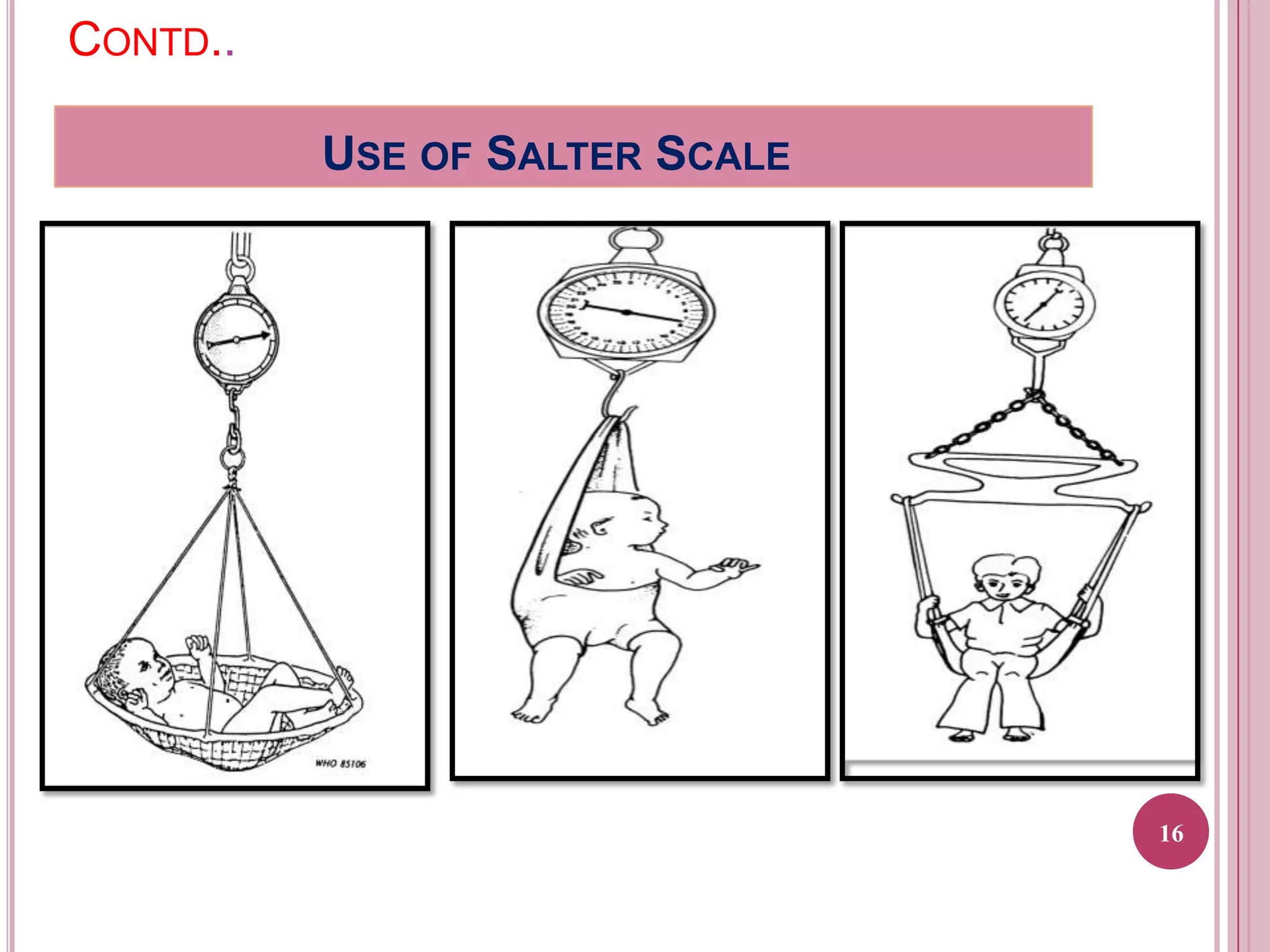
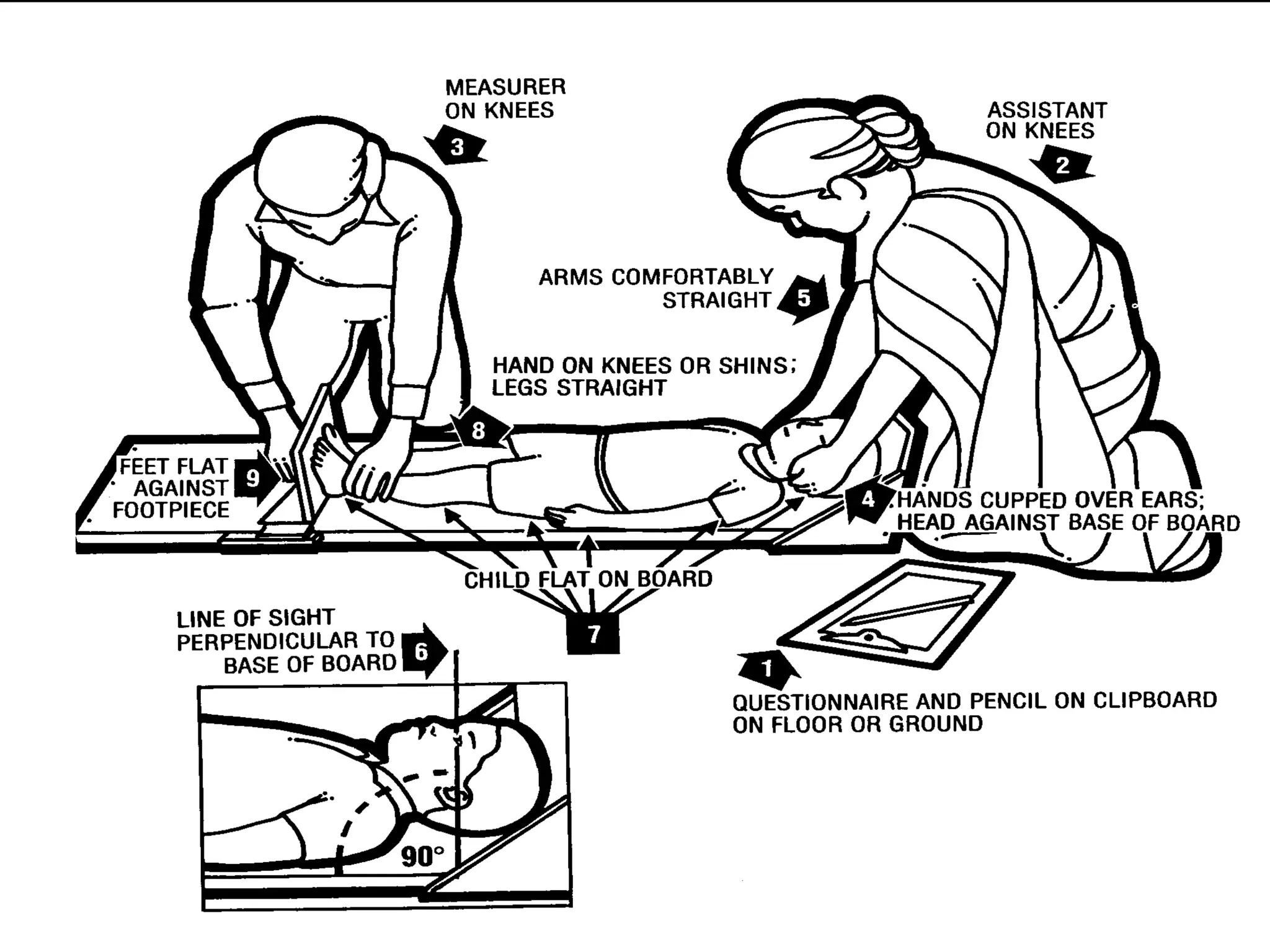
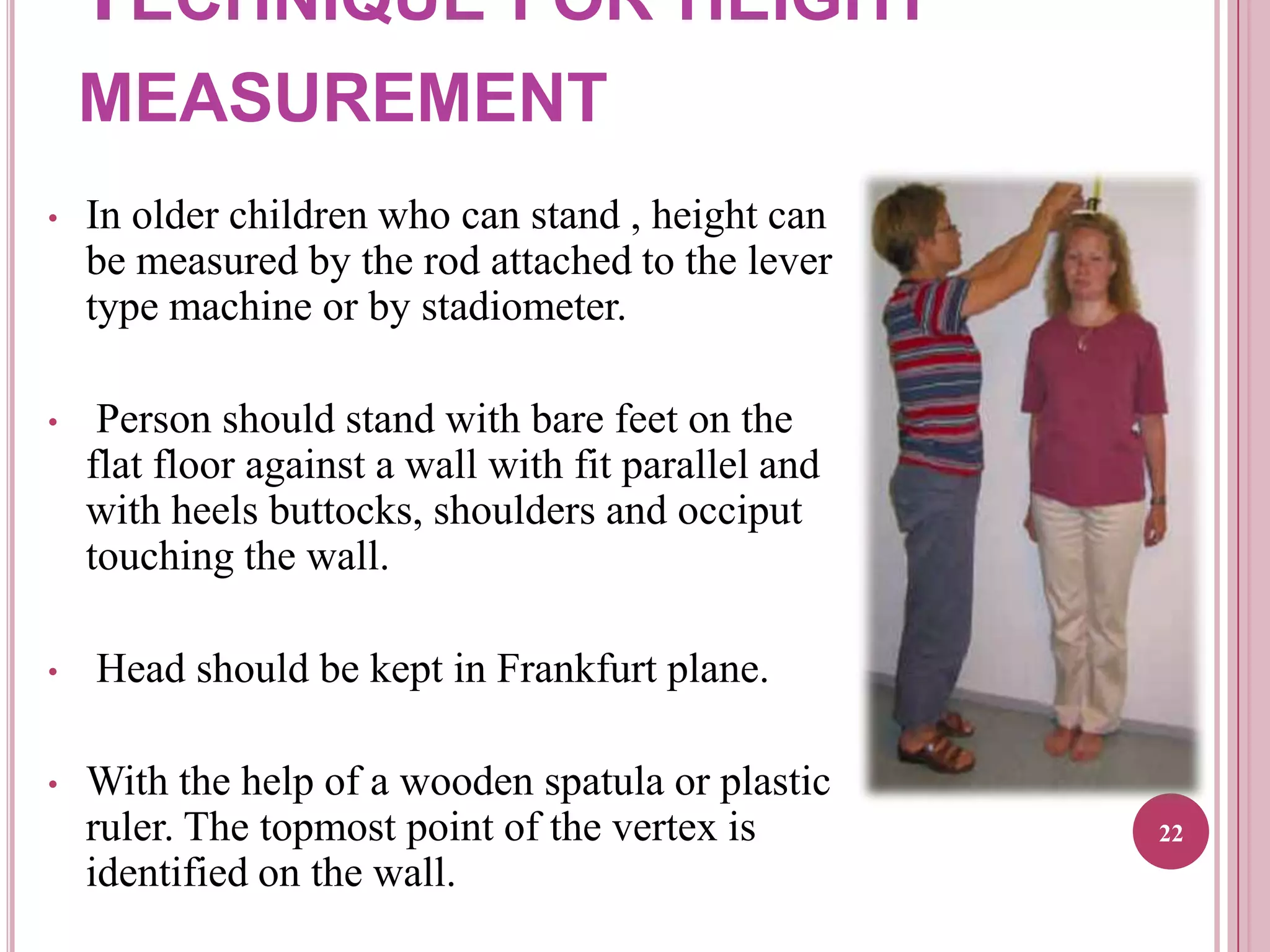
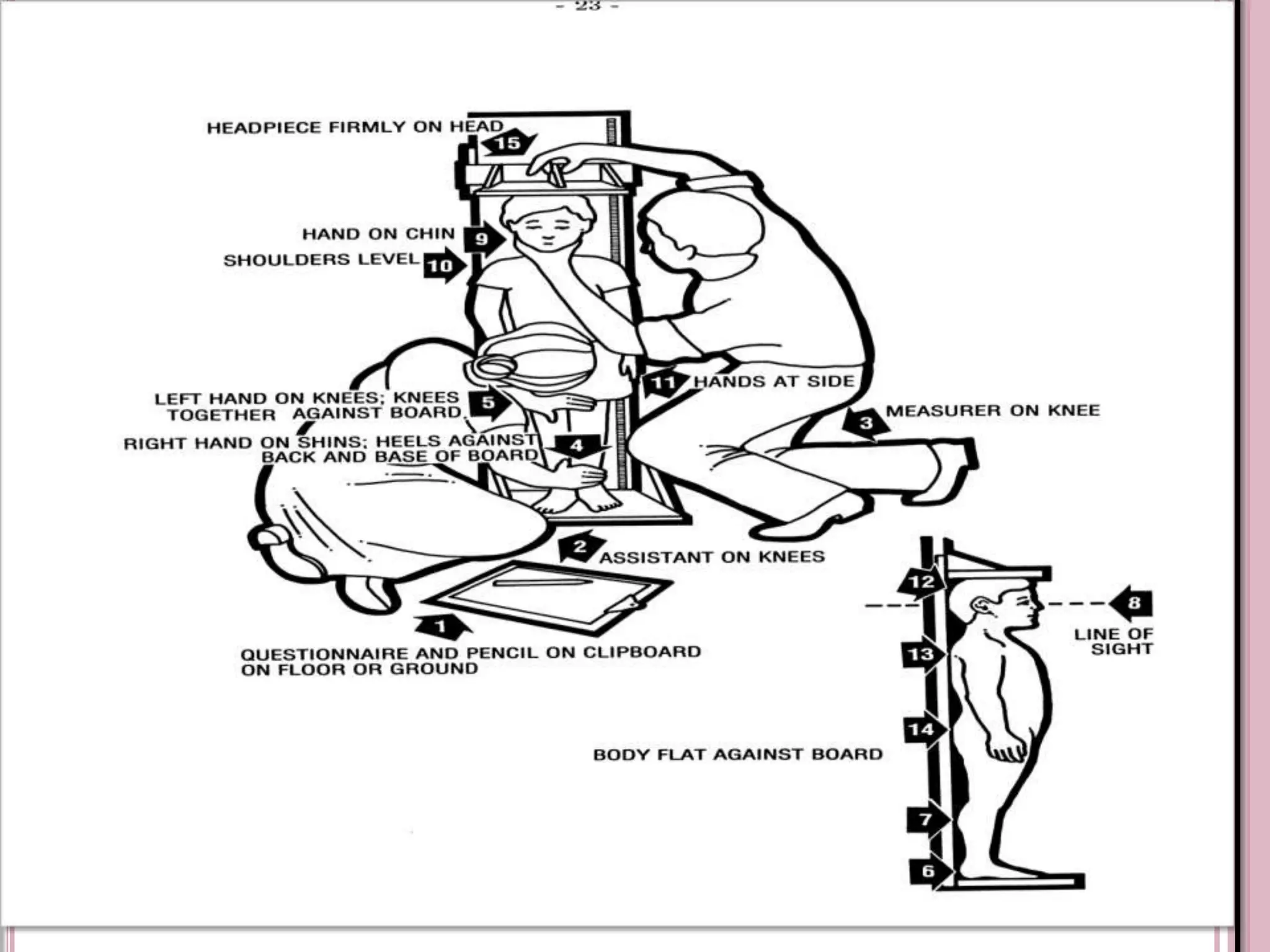
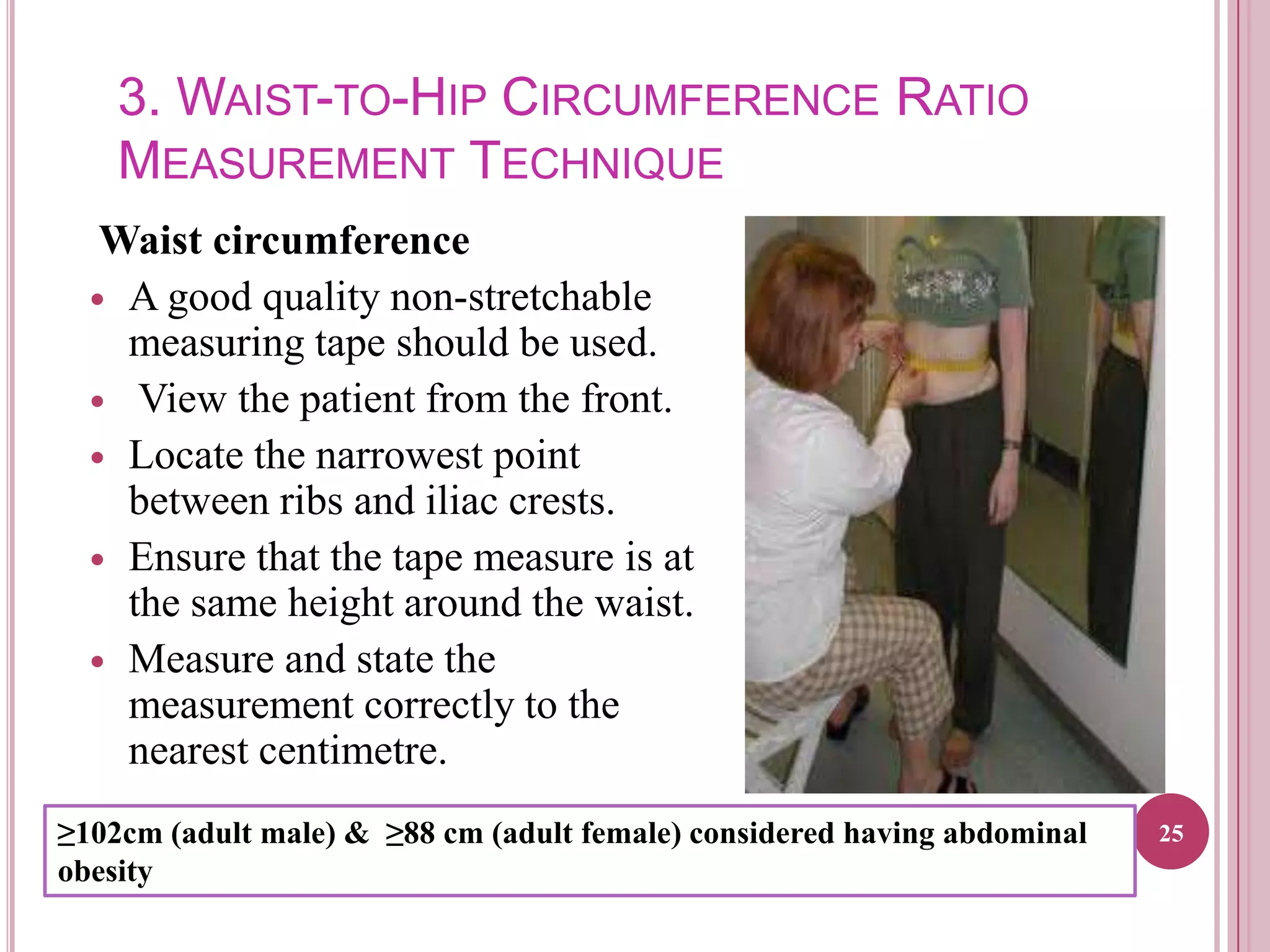
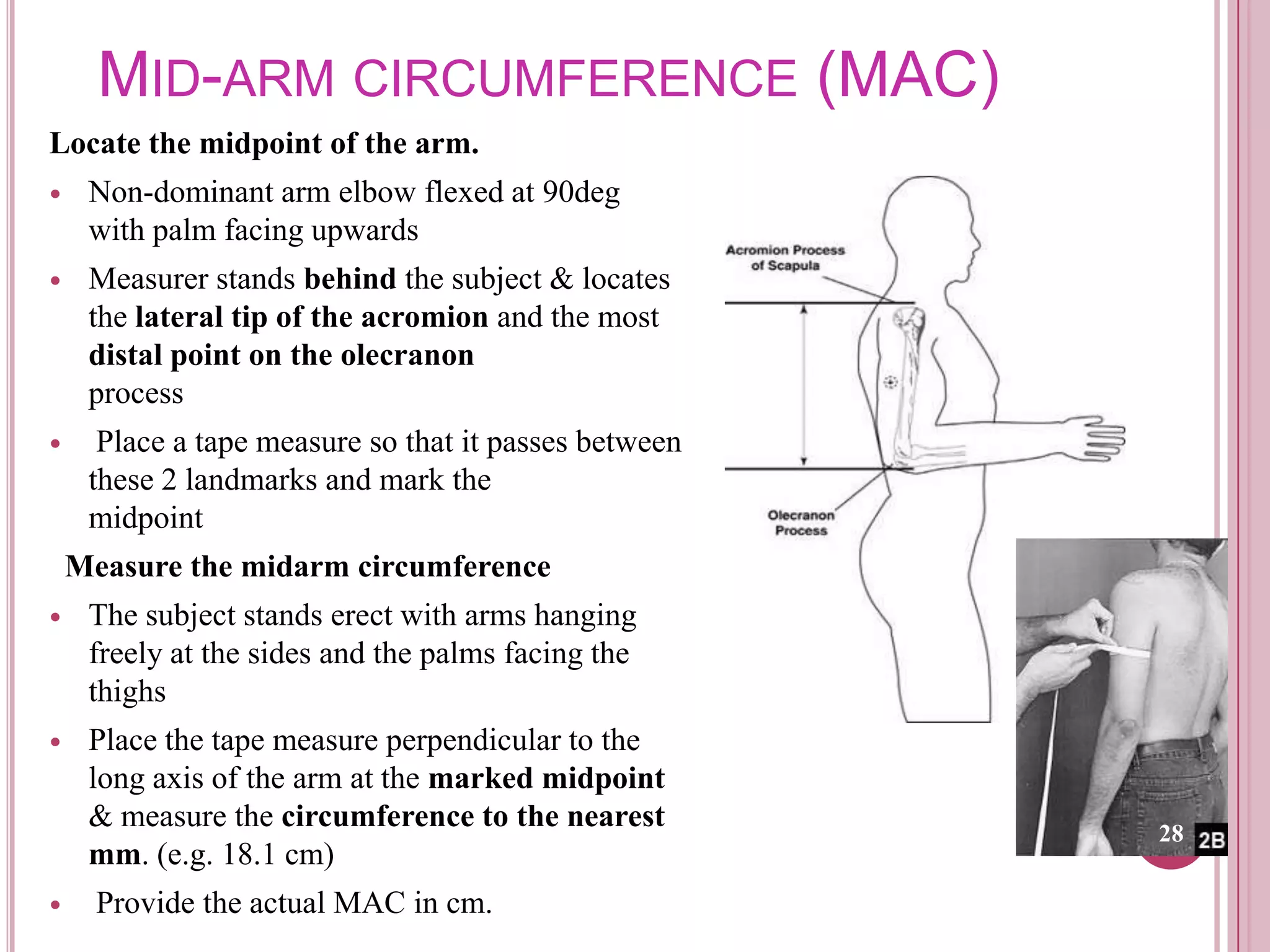
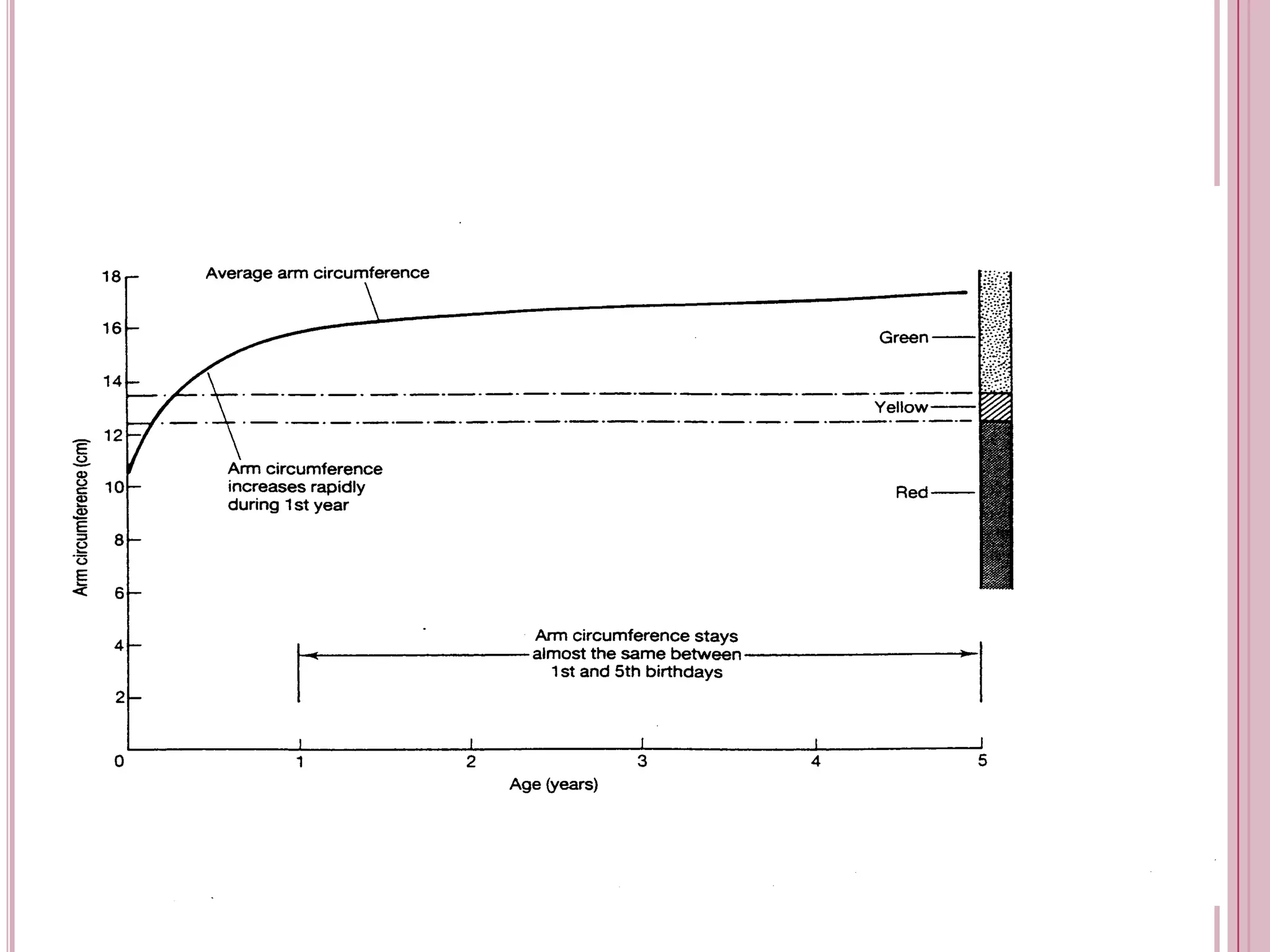
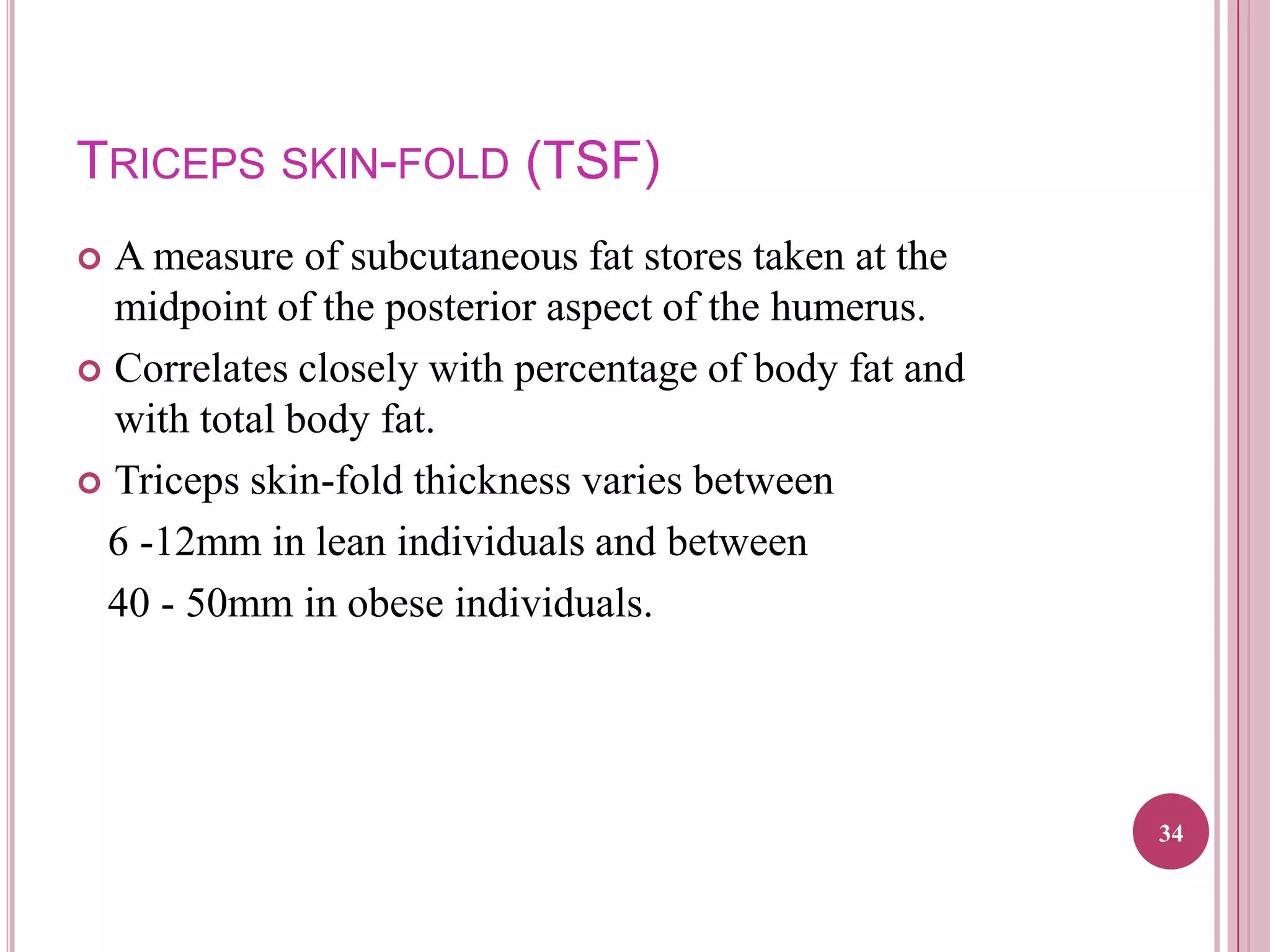
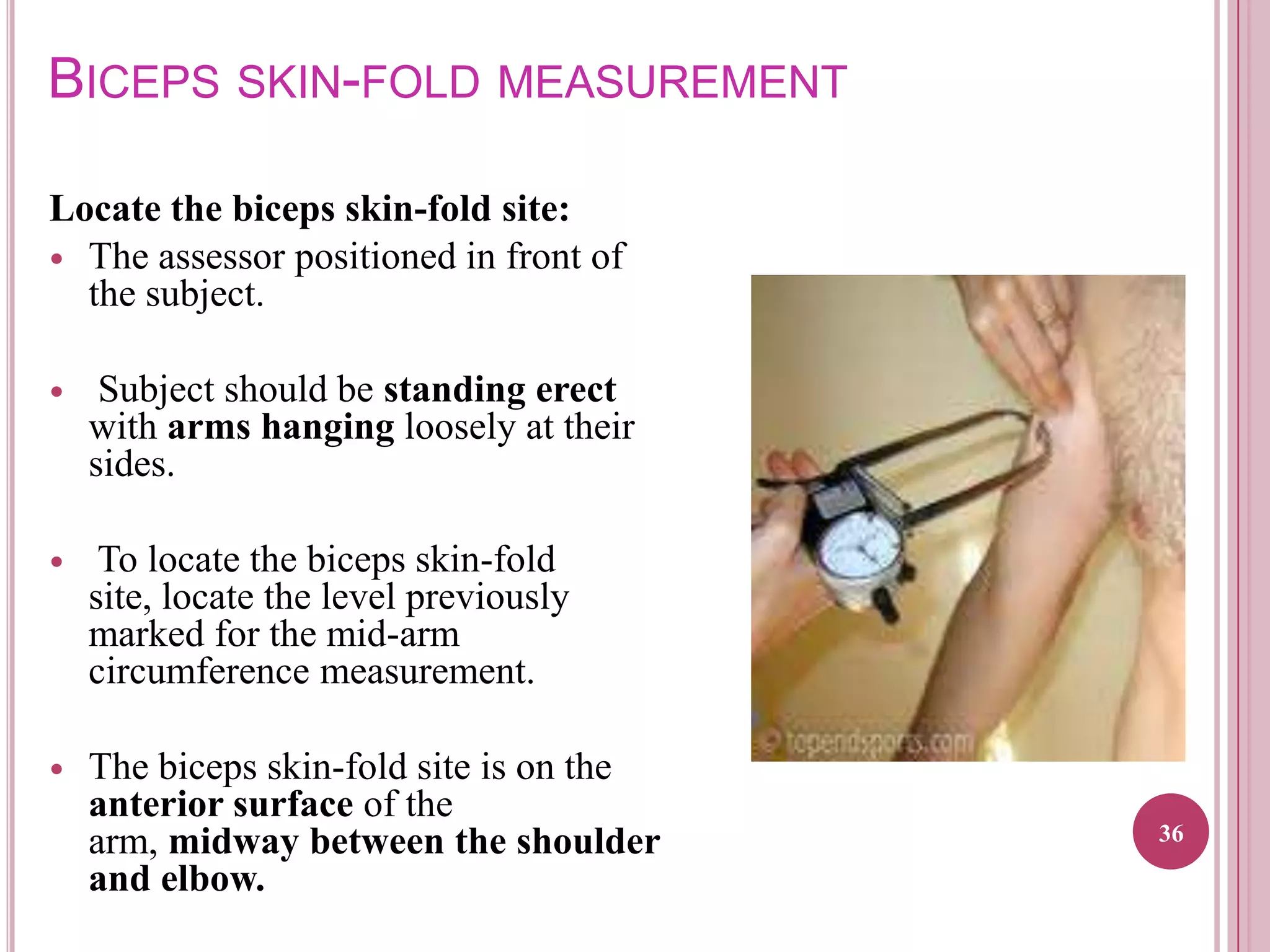
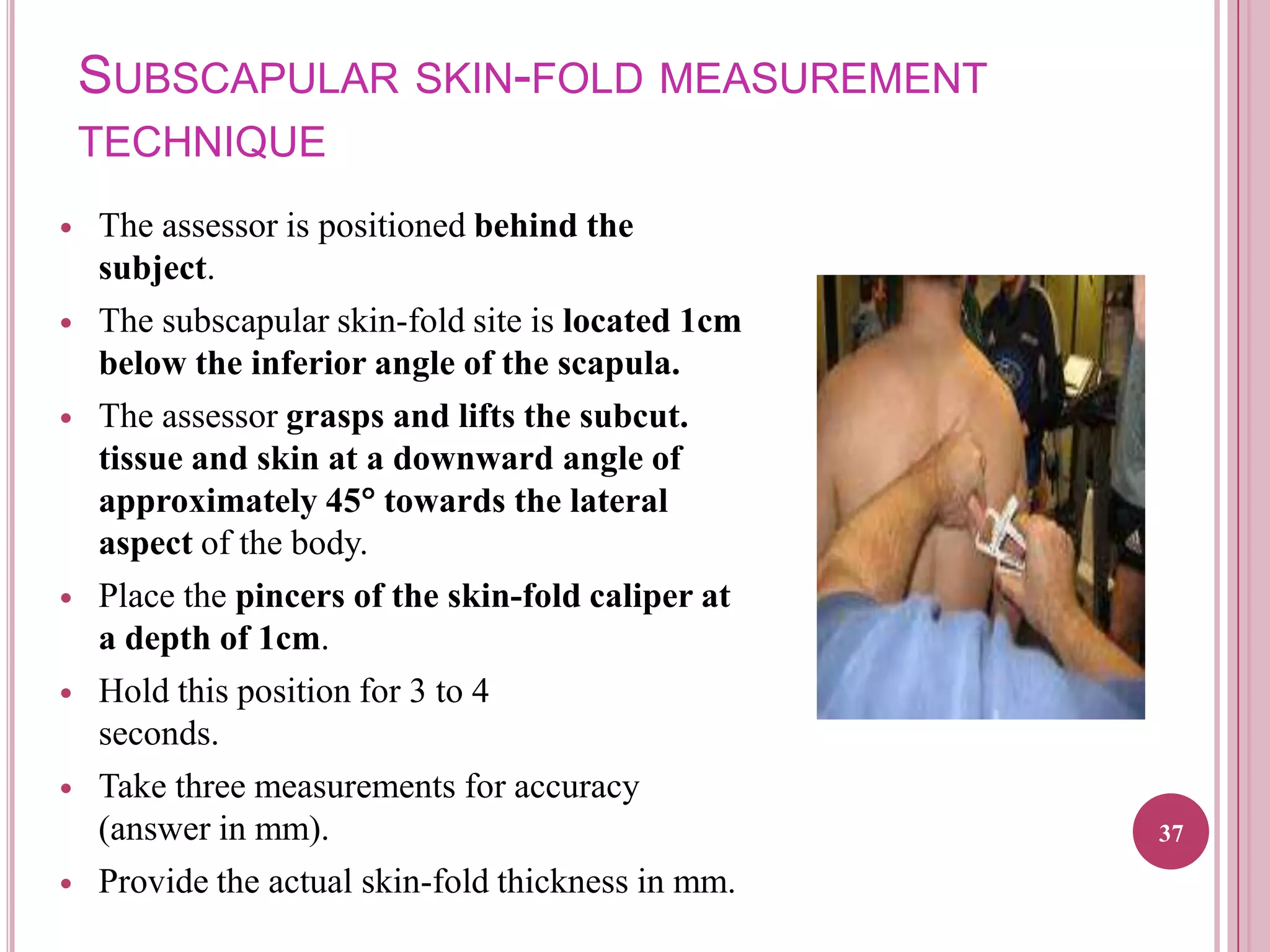
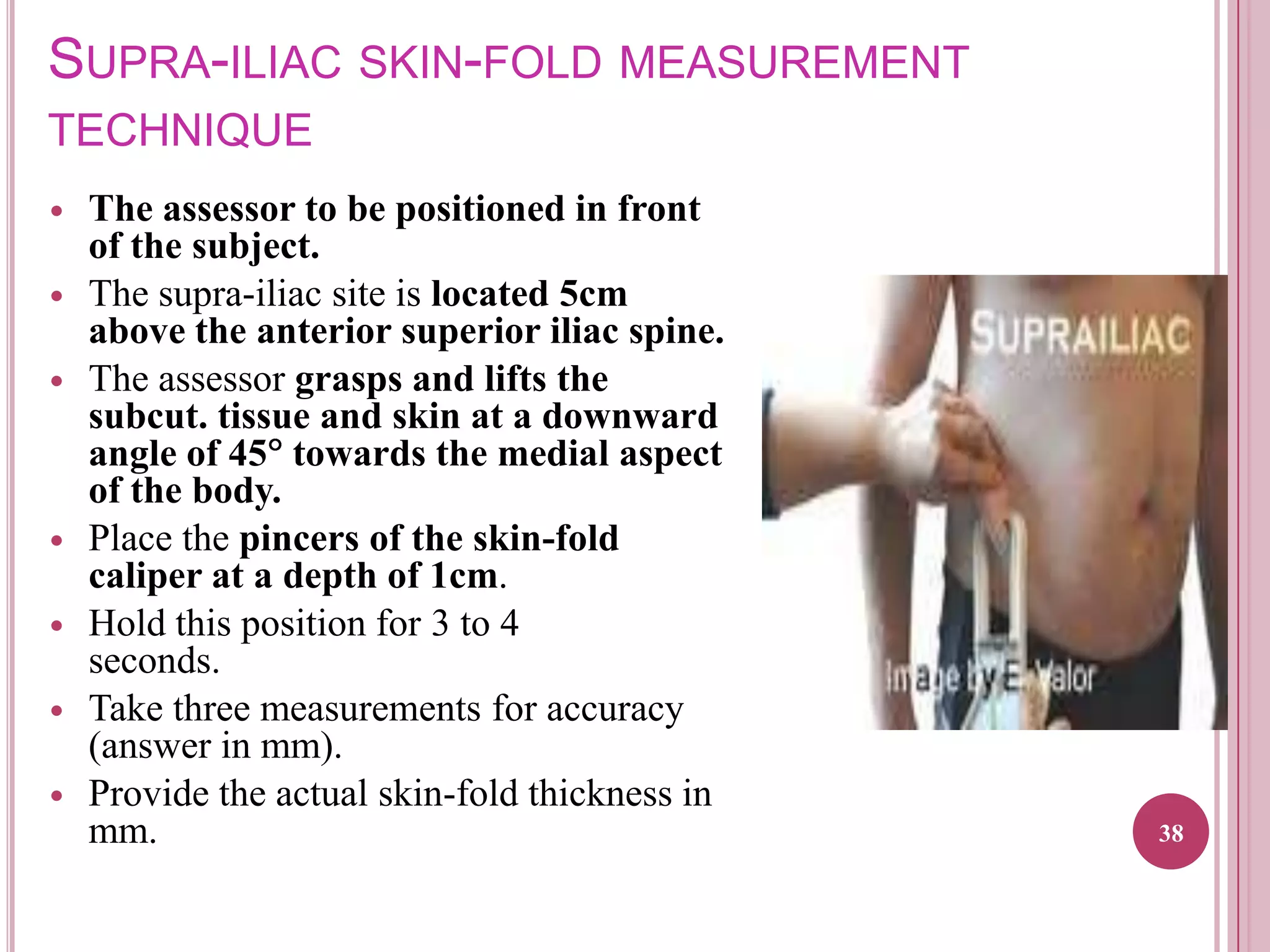
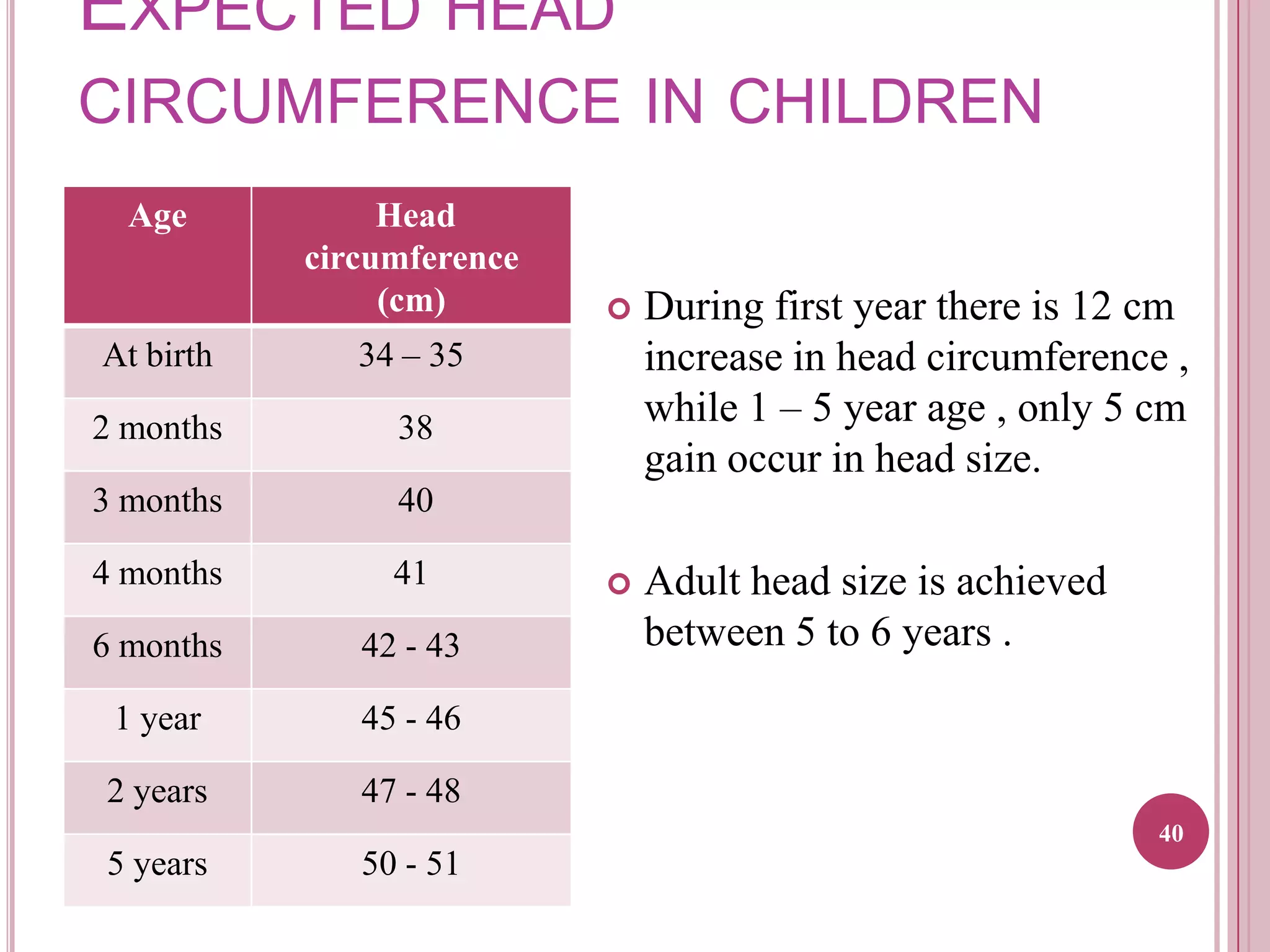
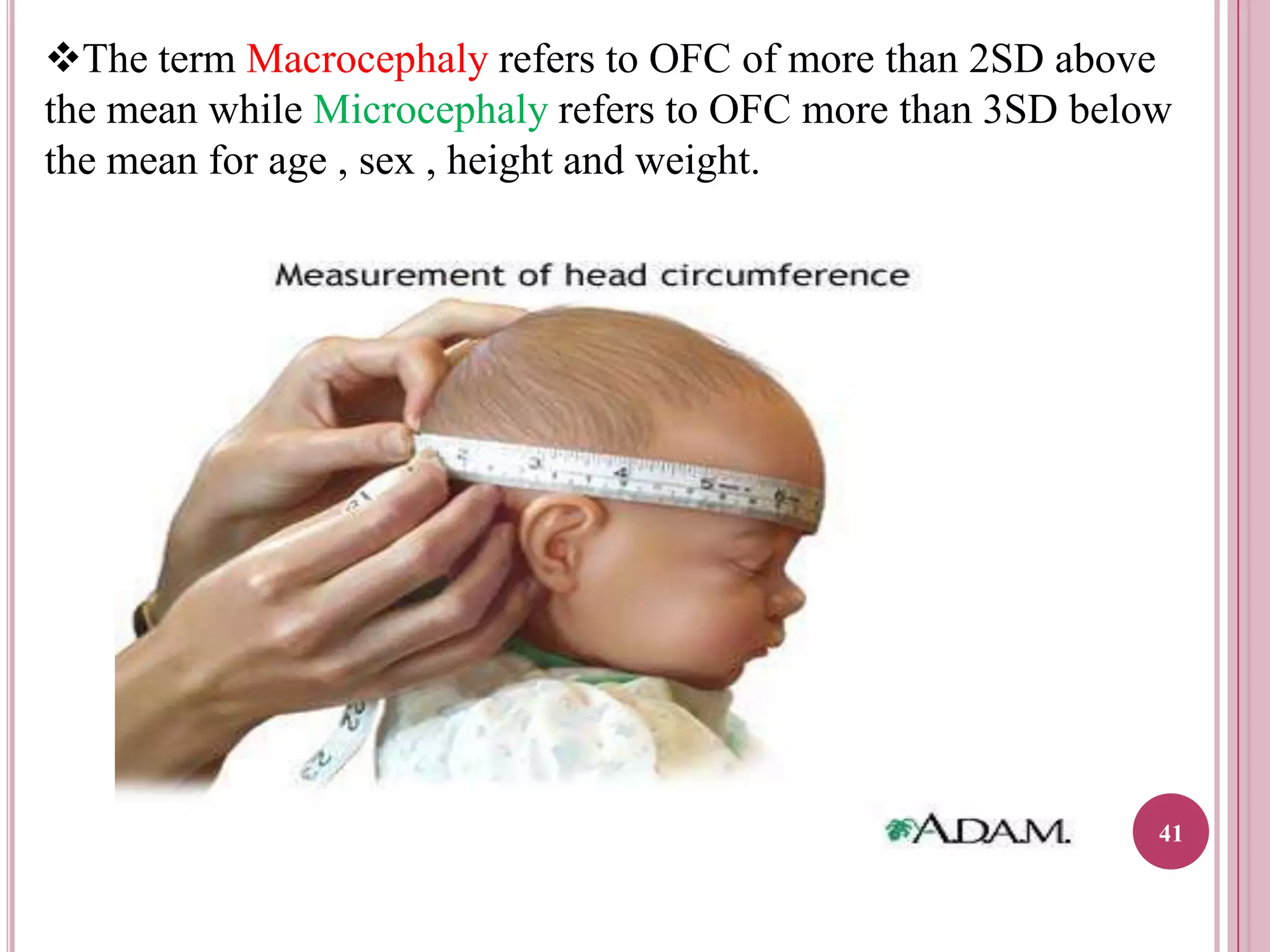
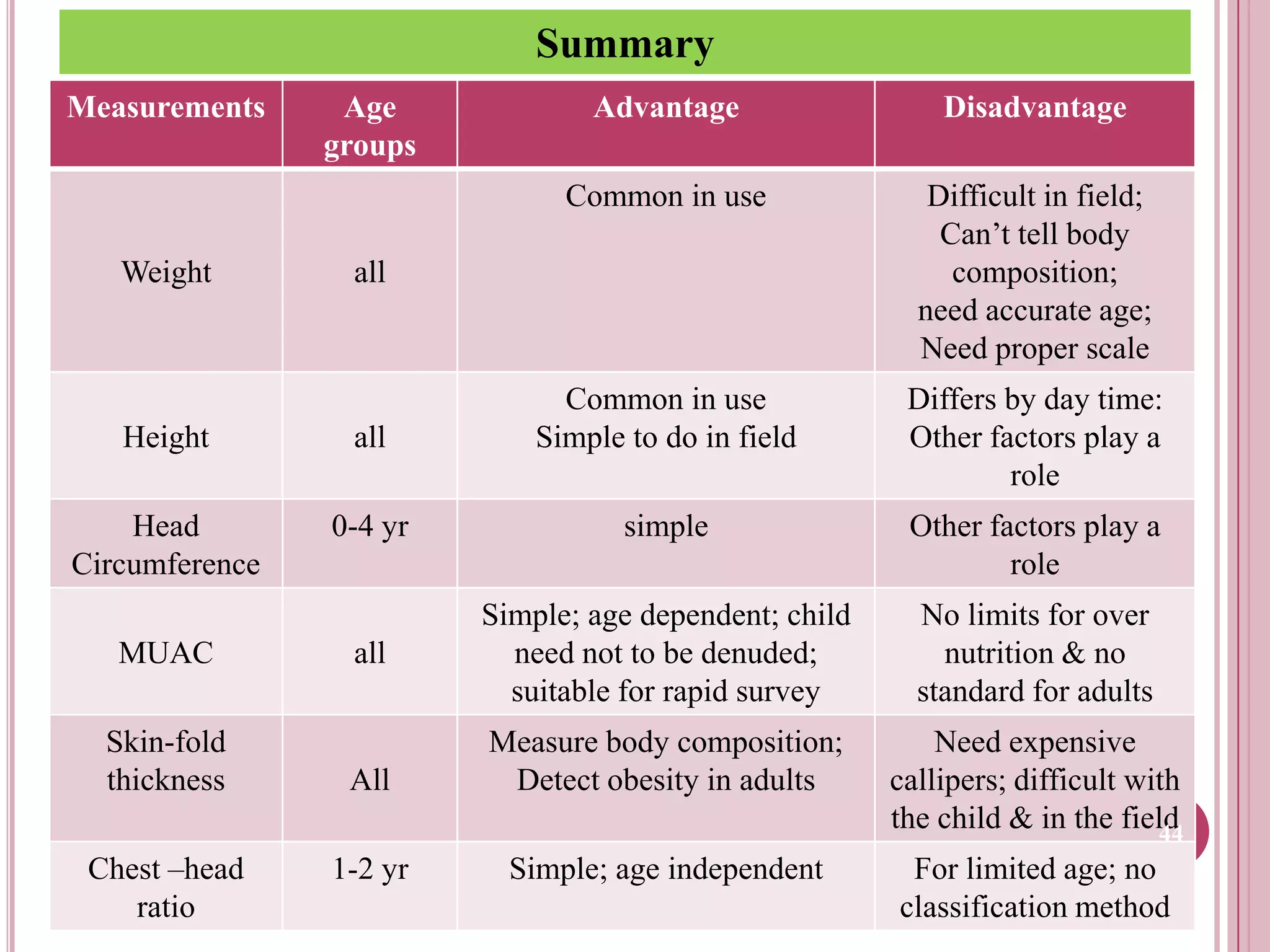
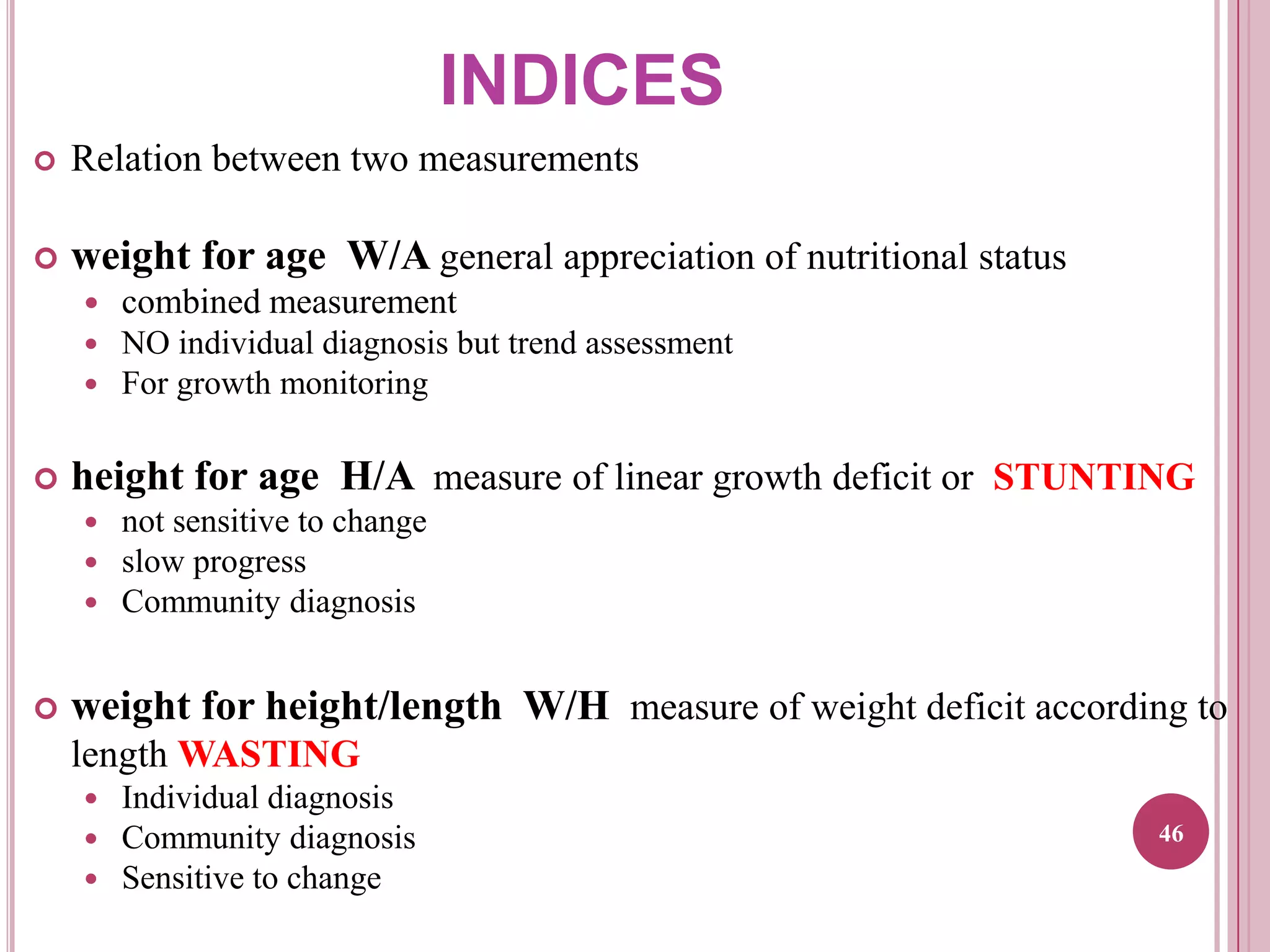
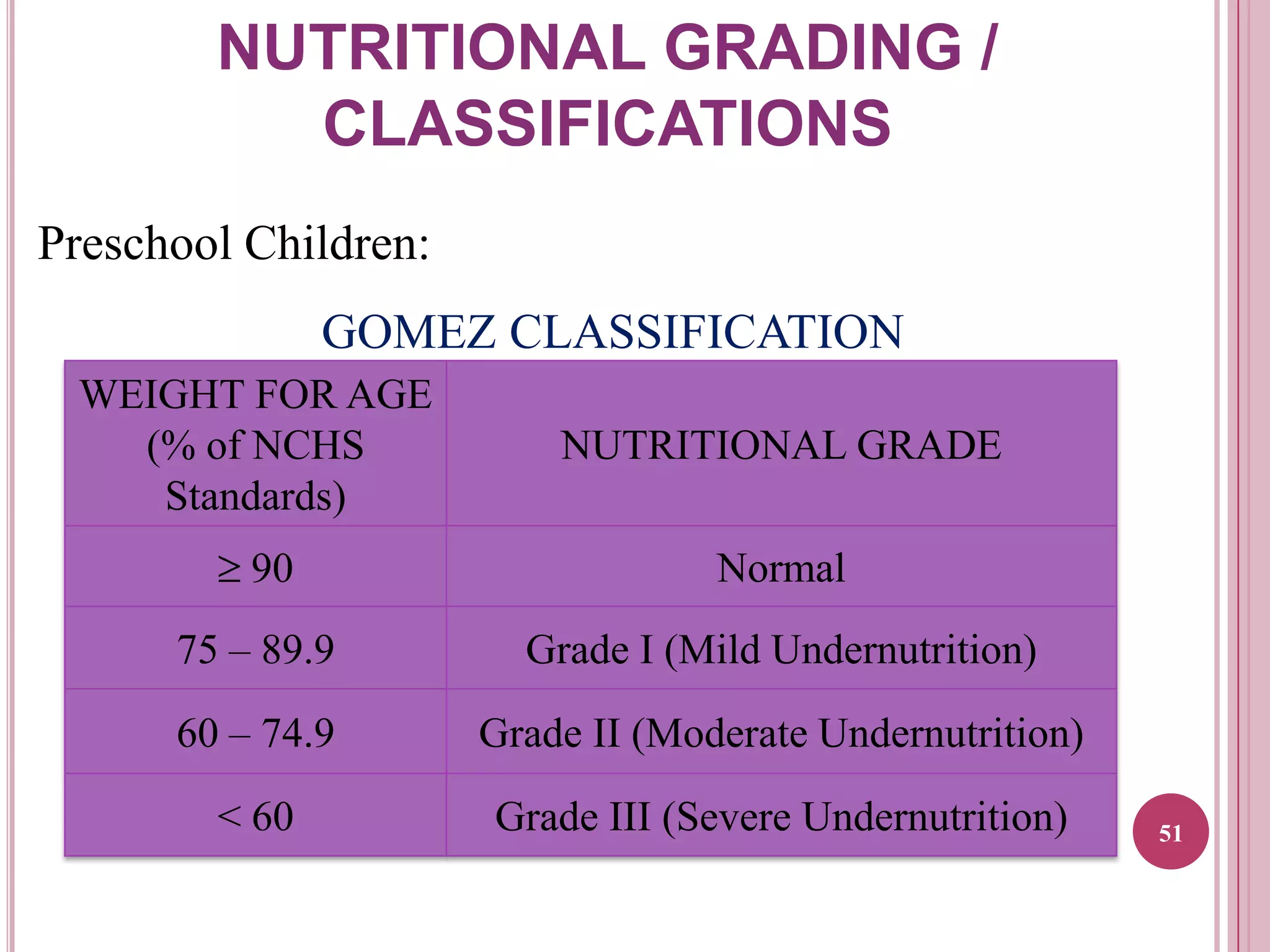
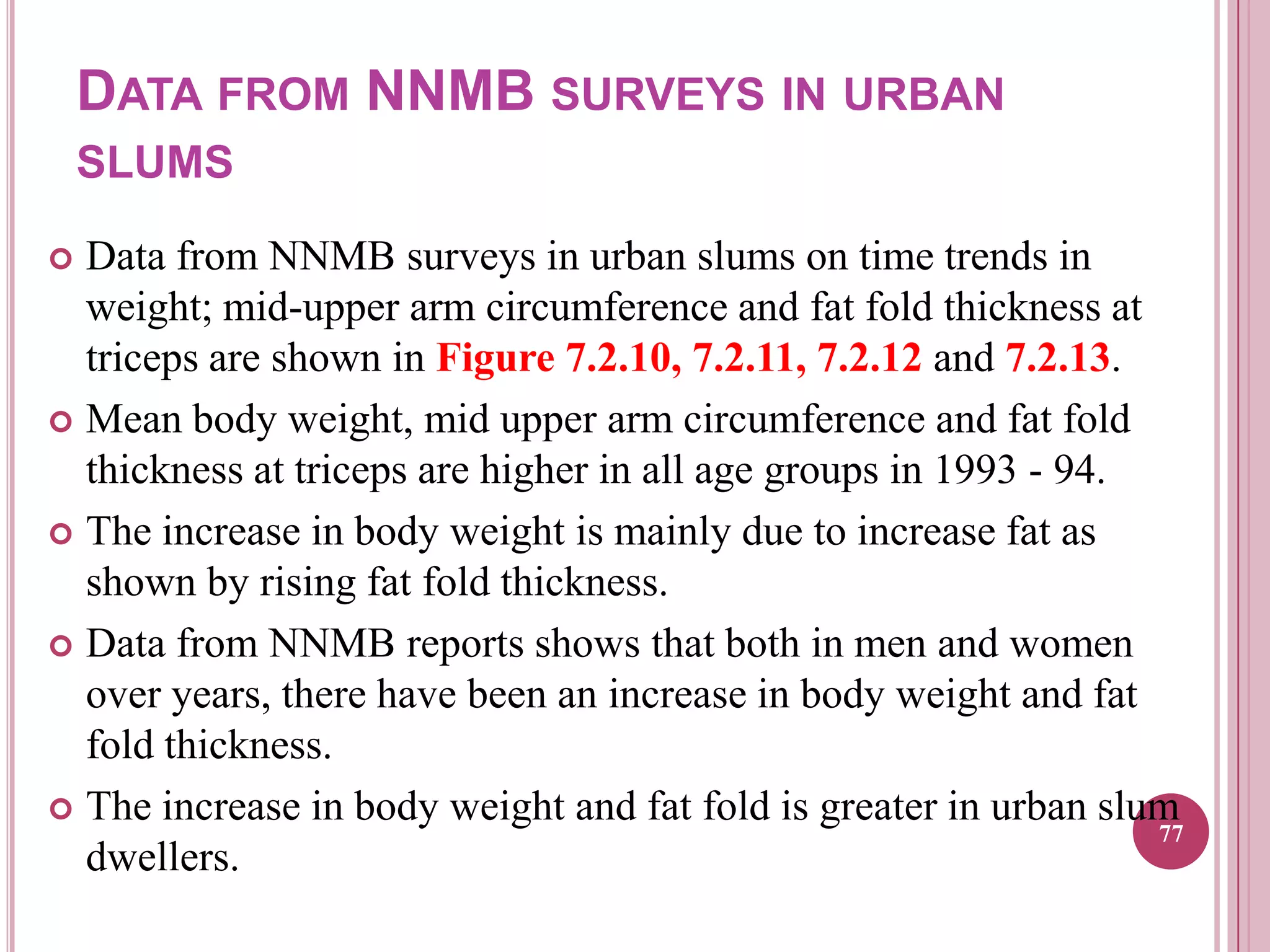
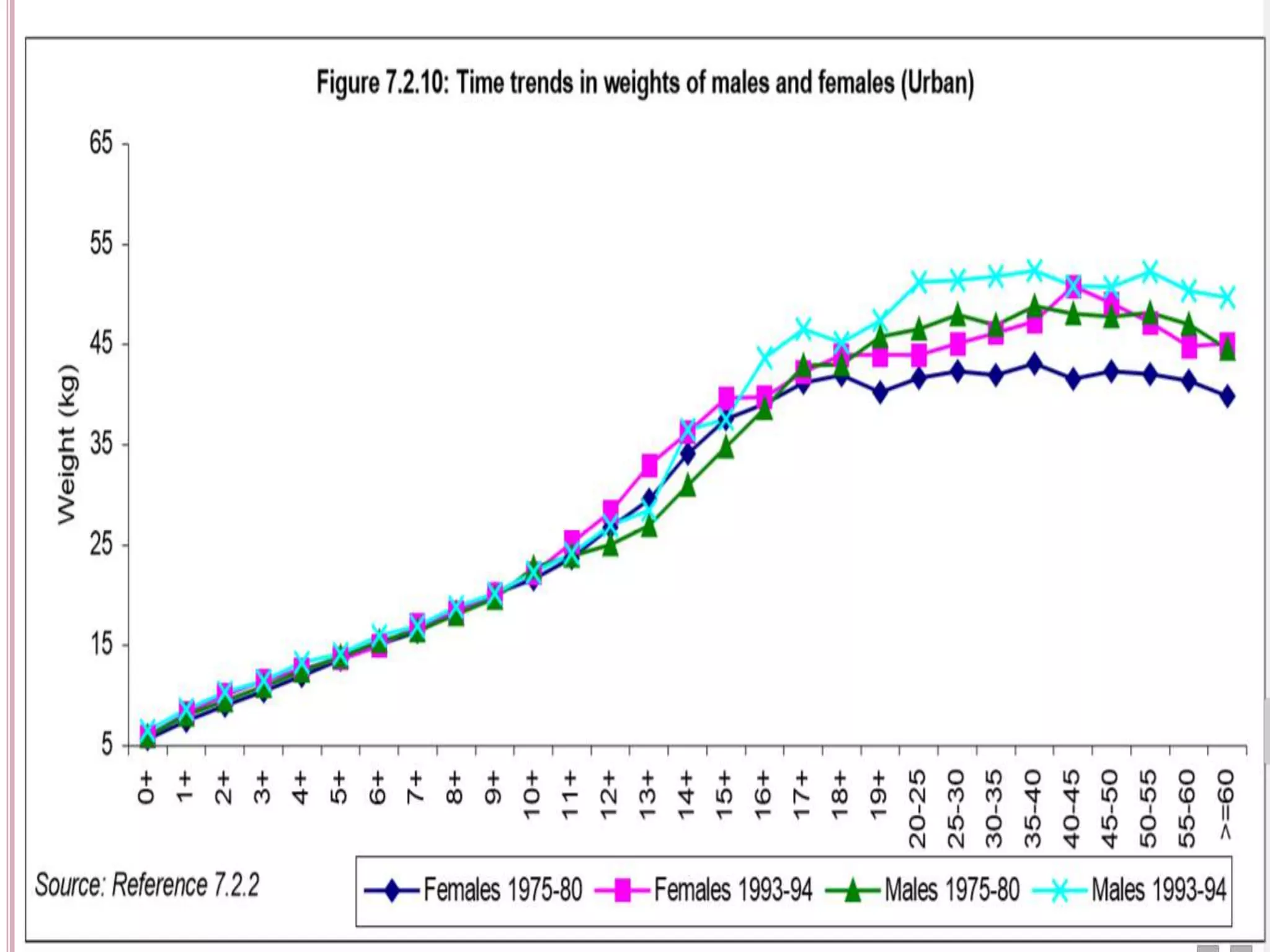
This document provides an overview of nutritional anthropometry. It begins by defining anthropometry as the quantitative measurement of the human body. It then discusses various anthropometric measurements that can be taken including weight, height, waist-to-hip ratio, mid-upper arm circumference, skin folds, head circumference, and chest circumference. The document provides details on techniques for accurately measuring each indicator. It explains how anthropometric data can be used at both individual and population levels. Key advantages and disadvantages of anthropometry are also summarized.