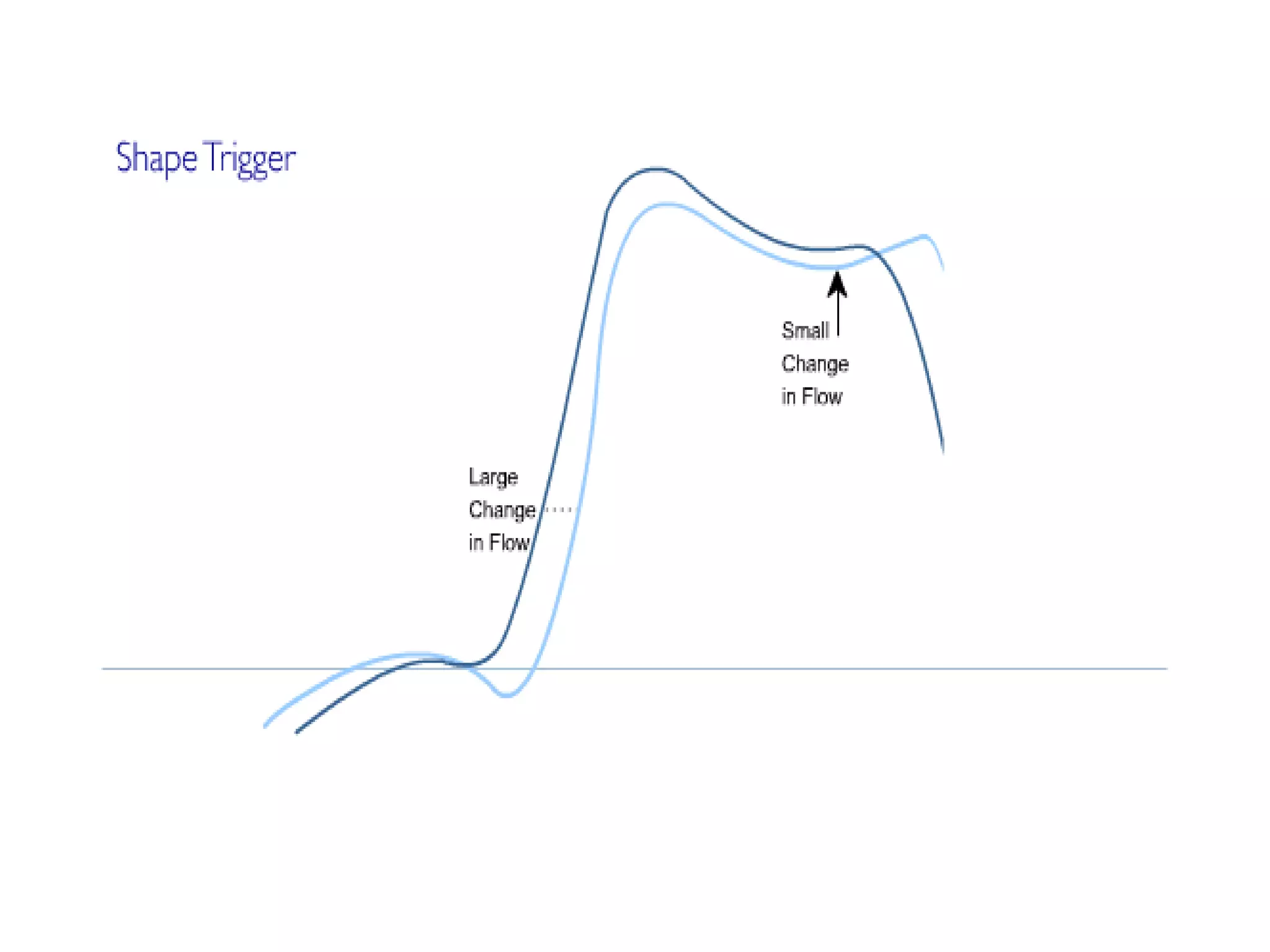
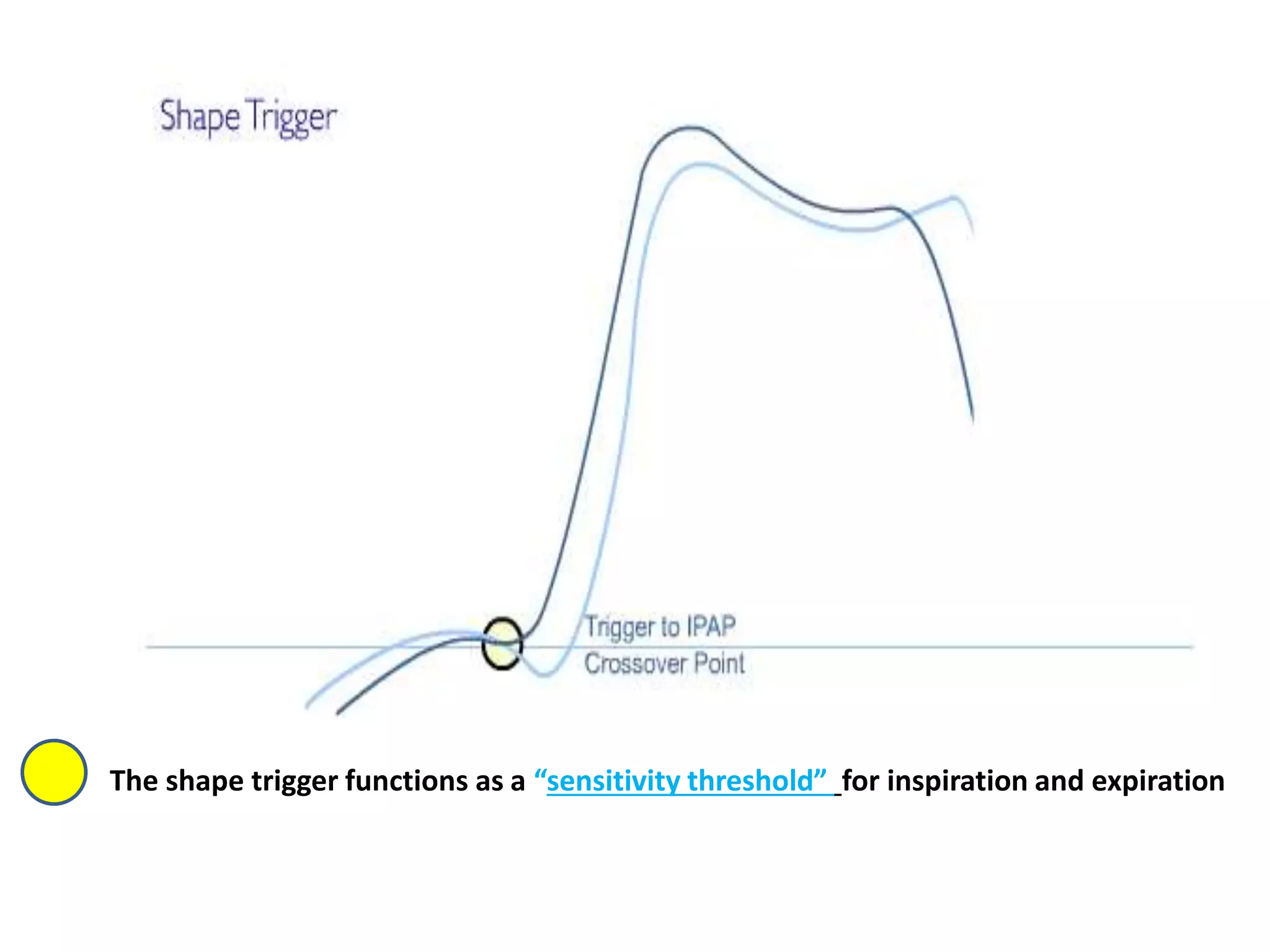
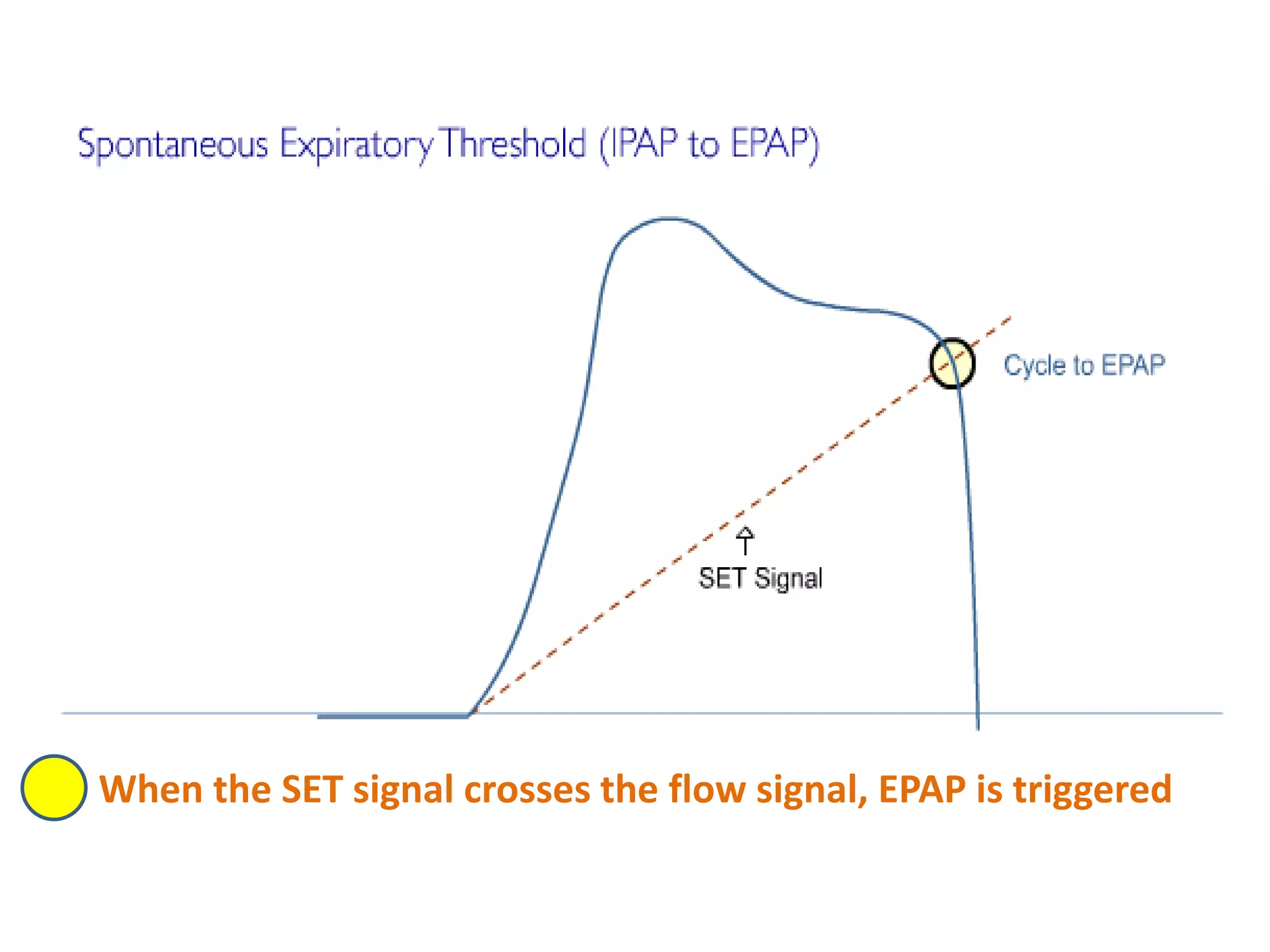
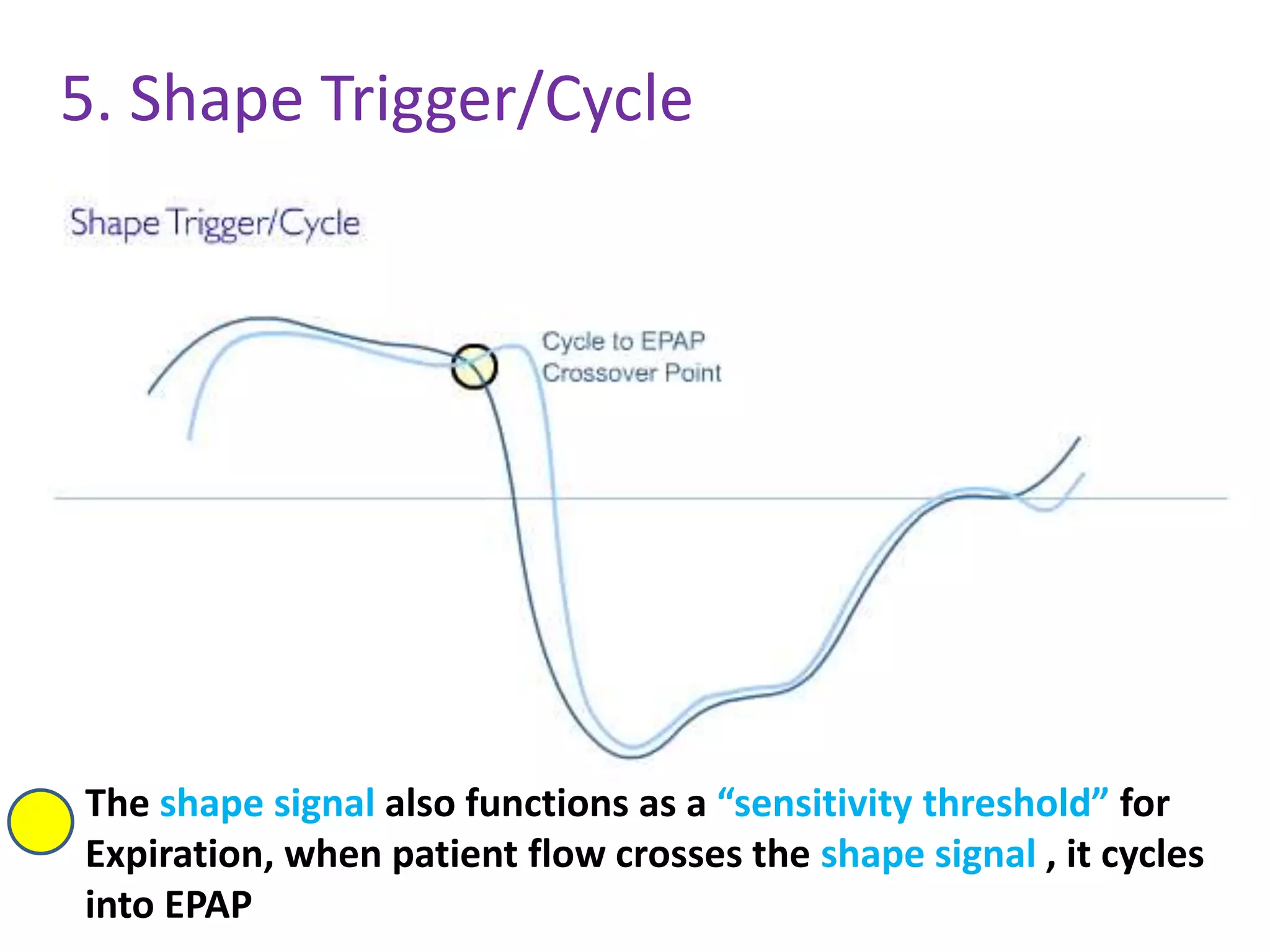
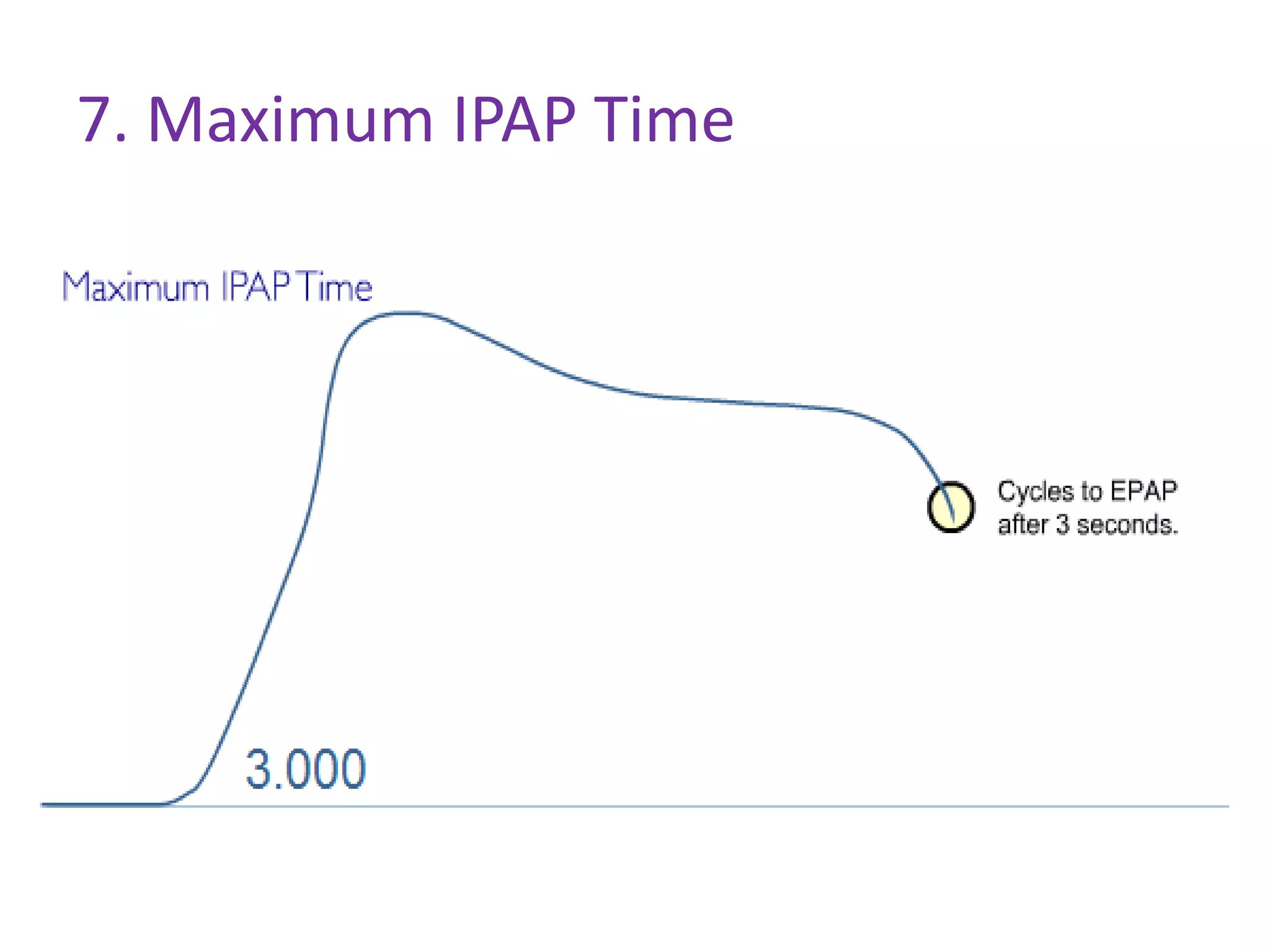
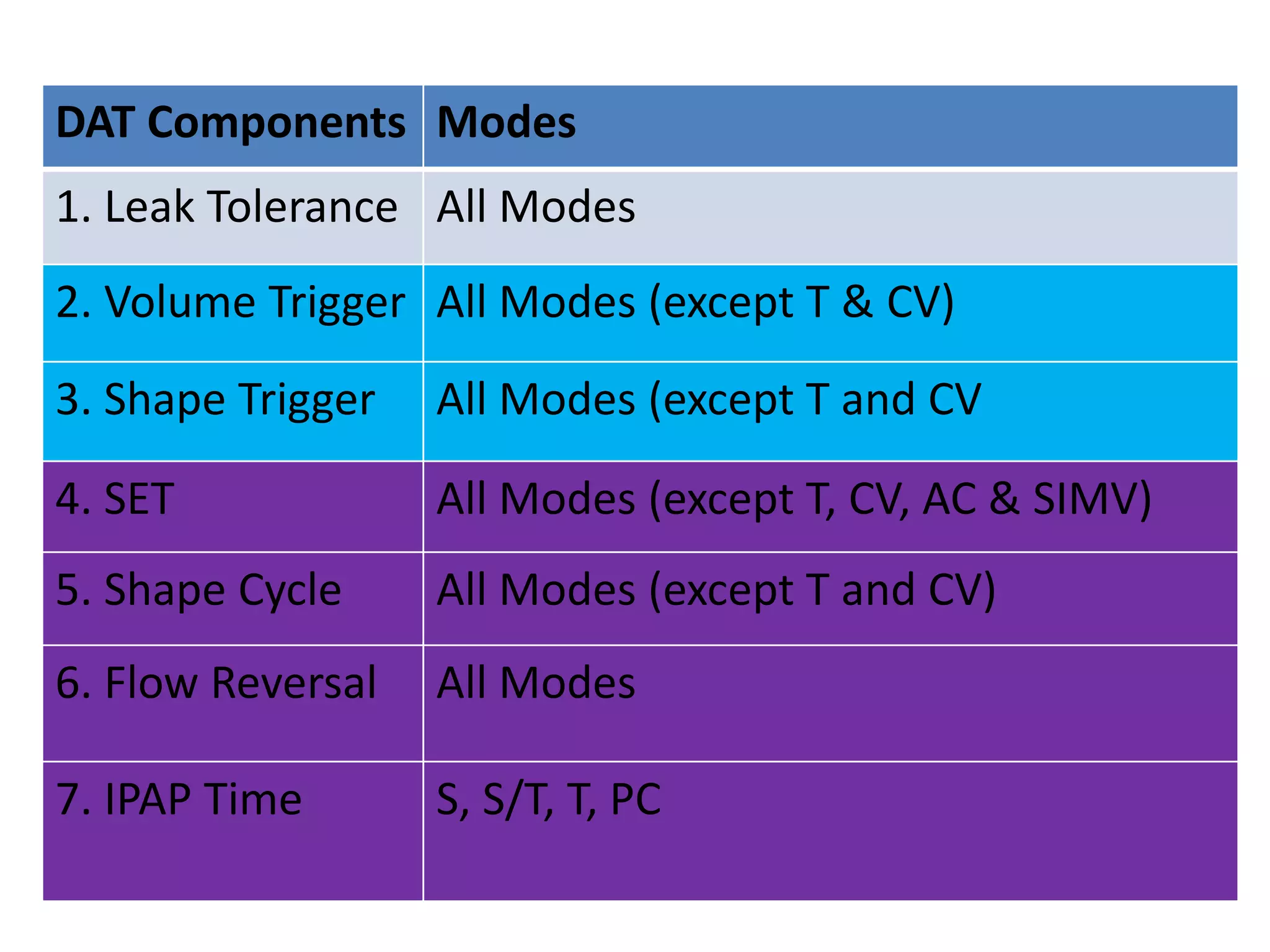
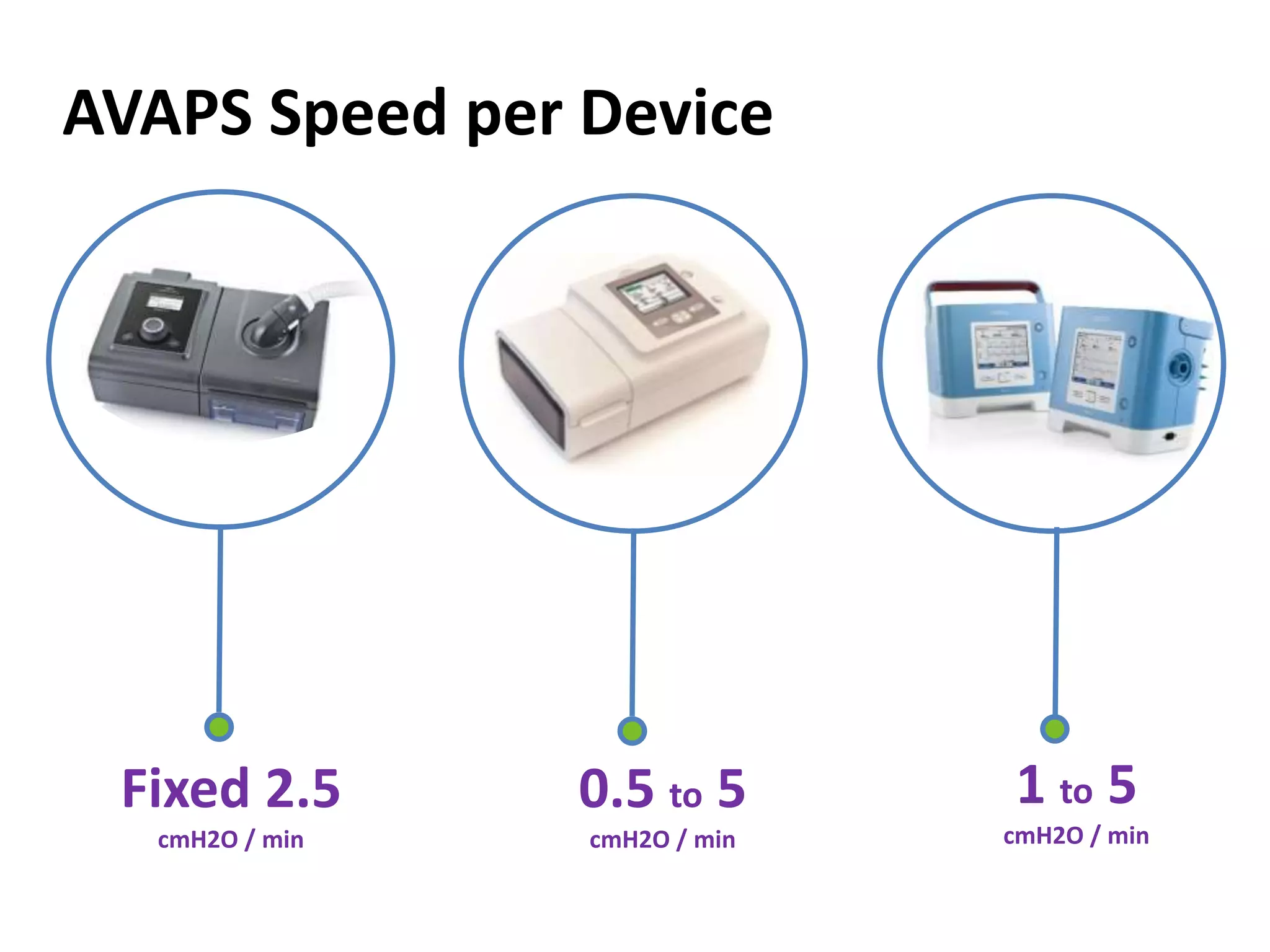
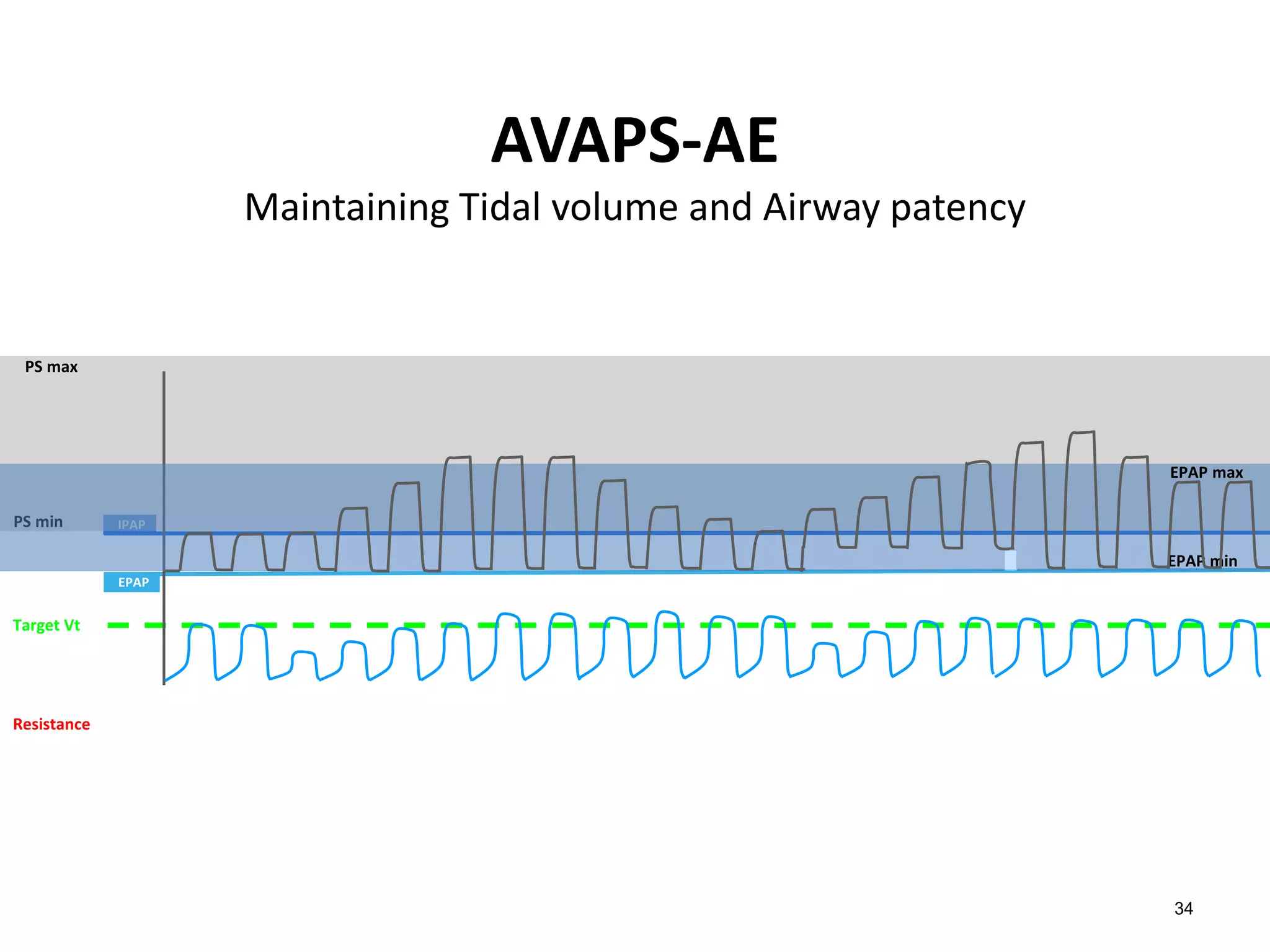
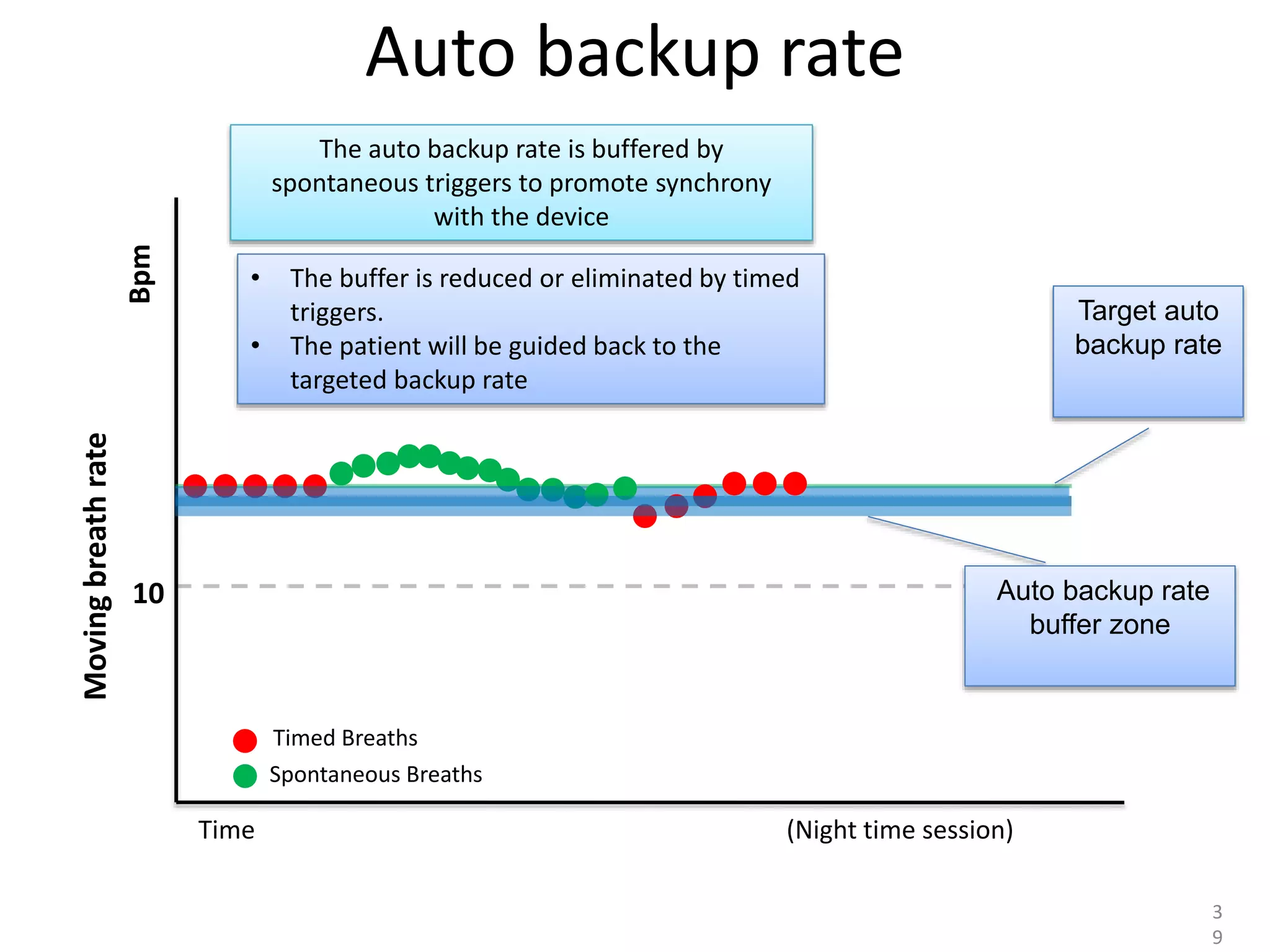
Philips Technologies offers several modes for non-invasive ventilation, including Digital AutoTrak (DAT) and hybrid modes. DAT uses algorithms to compensate for leaks, offering multiple options for triggering inspiration and expiring expiration. Hybrid modes like AVAPS and AVAPS-AE combine pressure support with targeted volume delivery. AVAPS-AE additionally features automatic EPAP adjustment to prevent airway closure and automatic backup rate selection to address inconsistent breathing patterns.