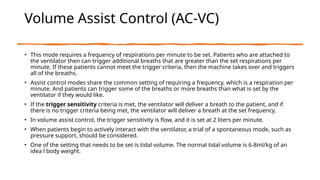
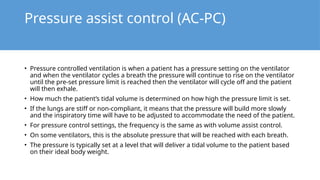
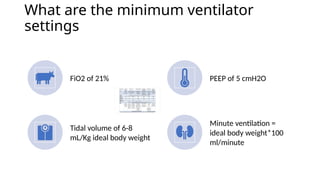
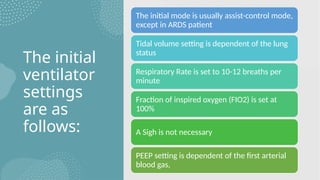
The document outlines the settings and modes for mechanical ventilation, detailing indications for use such as respiratory arrest and acute lung injury. It explains initial settings like assist-control mode and common ventilator parameters including FiO2, PEEP, and tidal volume, emphasizing the importance of adjusting these based on the patient's condition. The document also covers the different modes of ventilation, such as pressure assist control and volume assist control, and their respective functionalities and settings.






![How do you calculate an ideal body
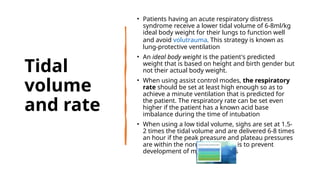
weight?
Men: Ideal Body Weight (kg) = [Height (cm) - 100] - ([Height (cm) - 100] x
10%)
Women: Ideal Body Weight (kg) = [Height (cm) - 100] + ([Height (cm) - 100] x
15%)
The reason behind using an ideal body weight instead of an actual body
weight is because. An actual body weight will overestimate the tidal volume
required.
Patients are required to be ventilated with a lower tidal volume of 6-8ml/kg](https://image.slidesharecdn.com/mechanicalventilatorsettingsandbasicmodes-240827032548-092601db/85/Mechanical-Ventilator-Settings-and-Basic-Modes-pptx-11-320.jpg)