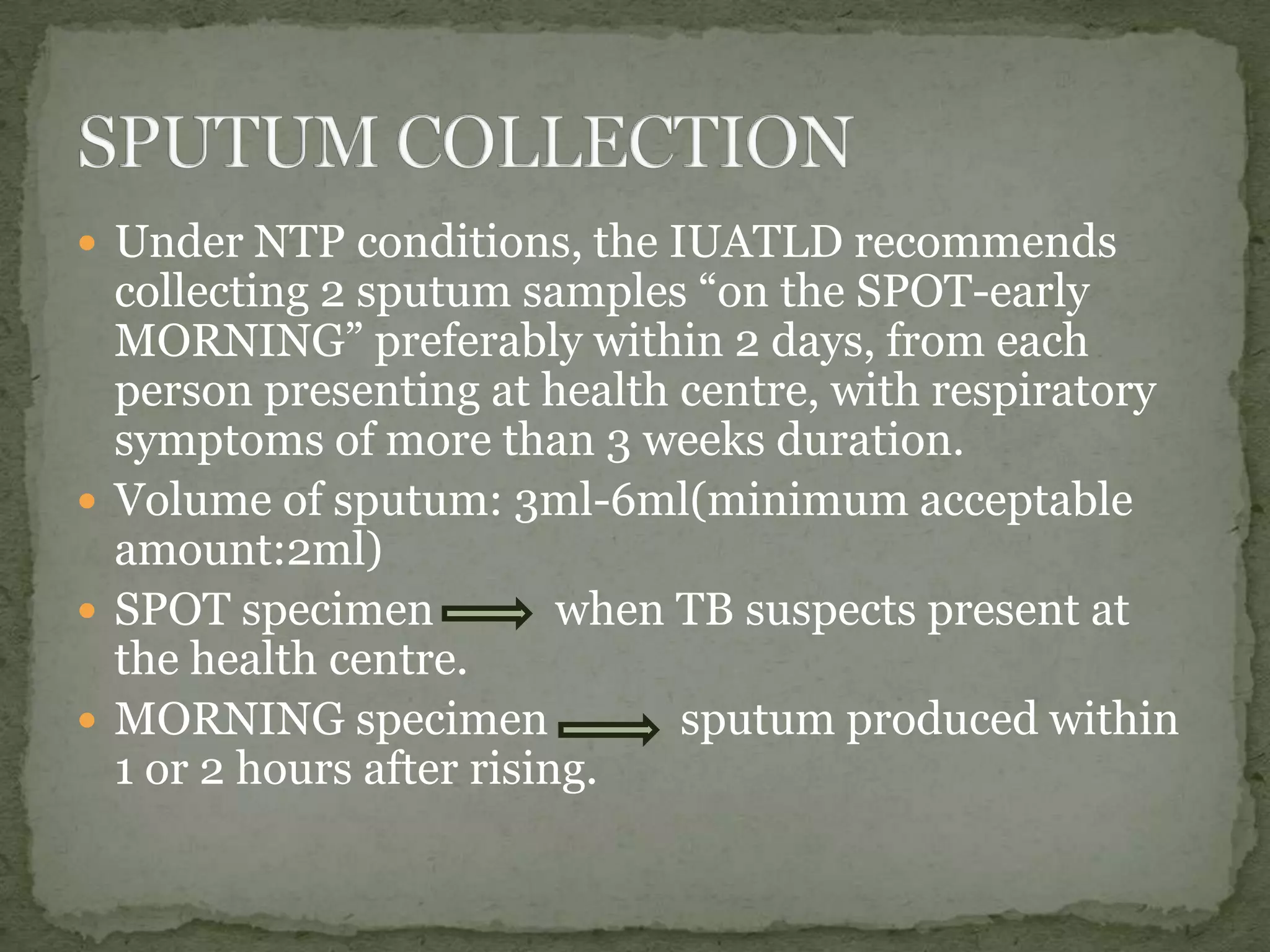
This document discusses sputum smear microscopy for the diagnosis of pulmonary tuberculosis. Sputum smear microscopy is the most confirmatory test but requires ensuring the sputum is from the lungs. It can miss 25% of positive cases with a single smear. When performed correctly it is simple, inexpensive, and provides timely results. Sputum smear microscopy is used for early diagnosis, confirming the acid-fast nature of the organism, monitoring treatment effectiveness, and determining if other tests are needed. The document outlines procedures for collecting and examining sputum samples via Ziehl-Neelsen staining under a microscope.







![ Transmitted light: Carbol fuchsin staining.[contrast
red colour AFB on blue background]
Fluorescence : Auramine staining[contrast
light/dark]](https://image.slidesharecdn.com/sputumafbtest-sreejitht-140223114501-phpapp02/75/TB-Sputum-AFB-Test-9-2048.jpg)










