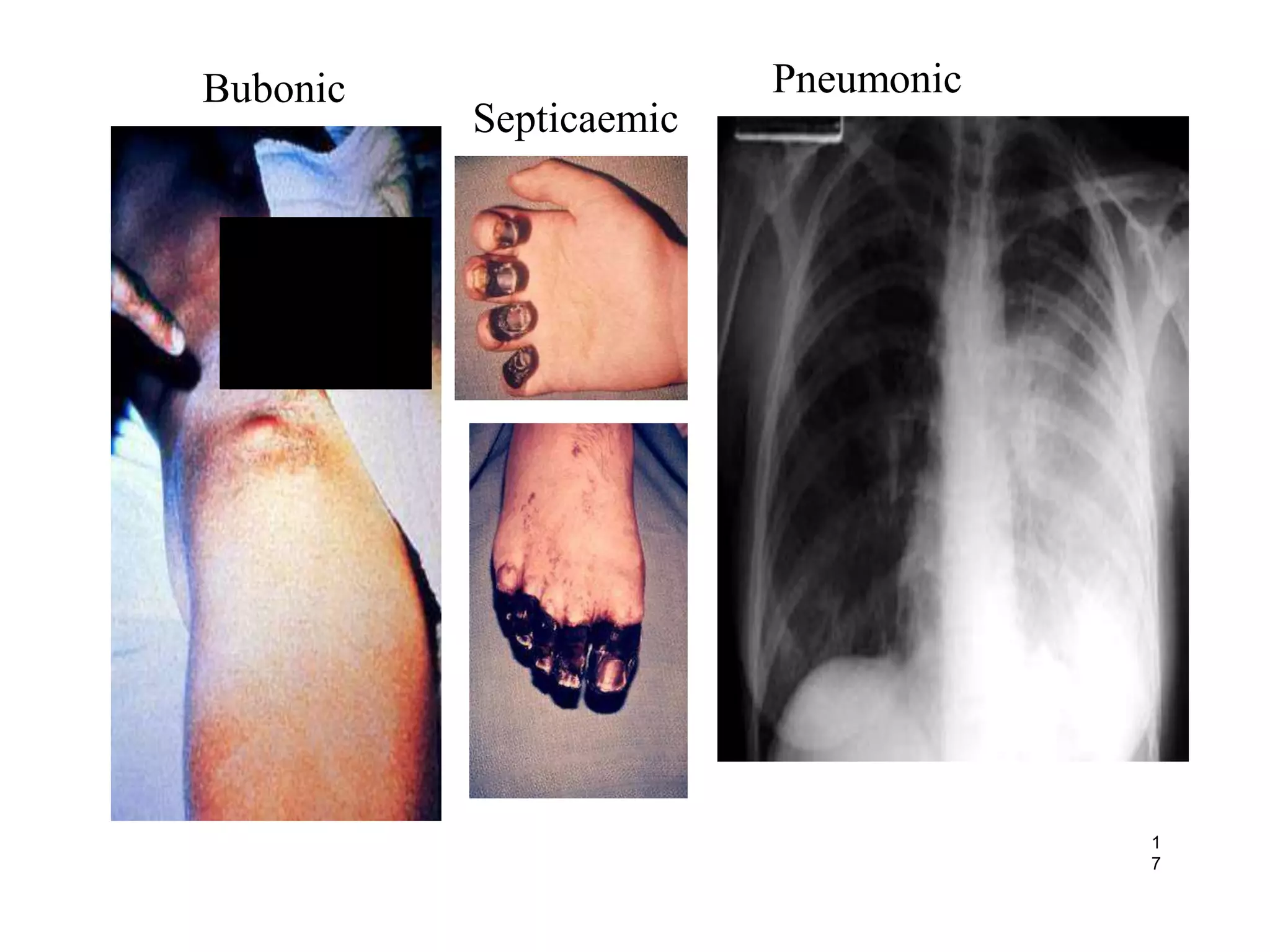
This document discusses Yersinia pestis, the bacteria that causes plague. It describes the key characteristics of Y. pestis, including that it is a gram-negative rod-shaped bacteria. It also outlines the three main forms of plague caused by Y. pestis: bubonic plague, septicemic plague, and pneumonic plague. The document provides details on the transmission, symptoms, treatment, and prevention of plague caused by this pathogenic bacteria.