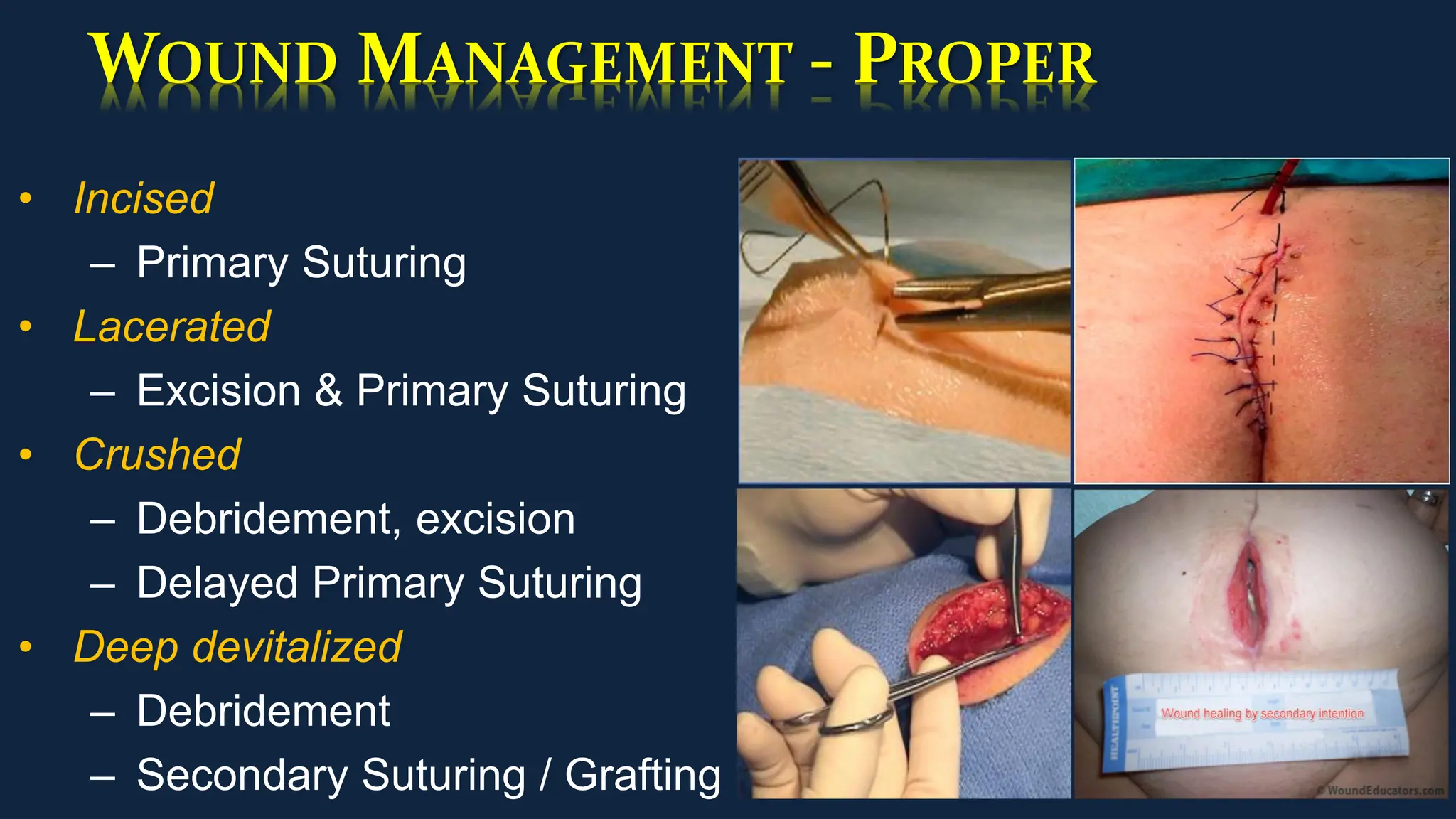
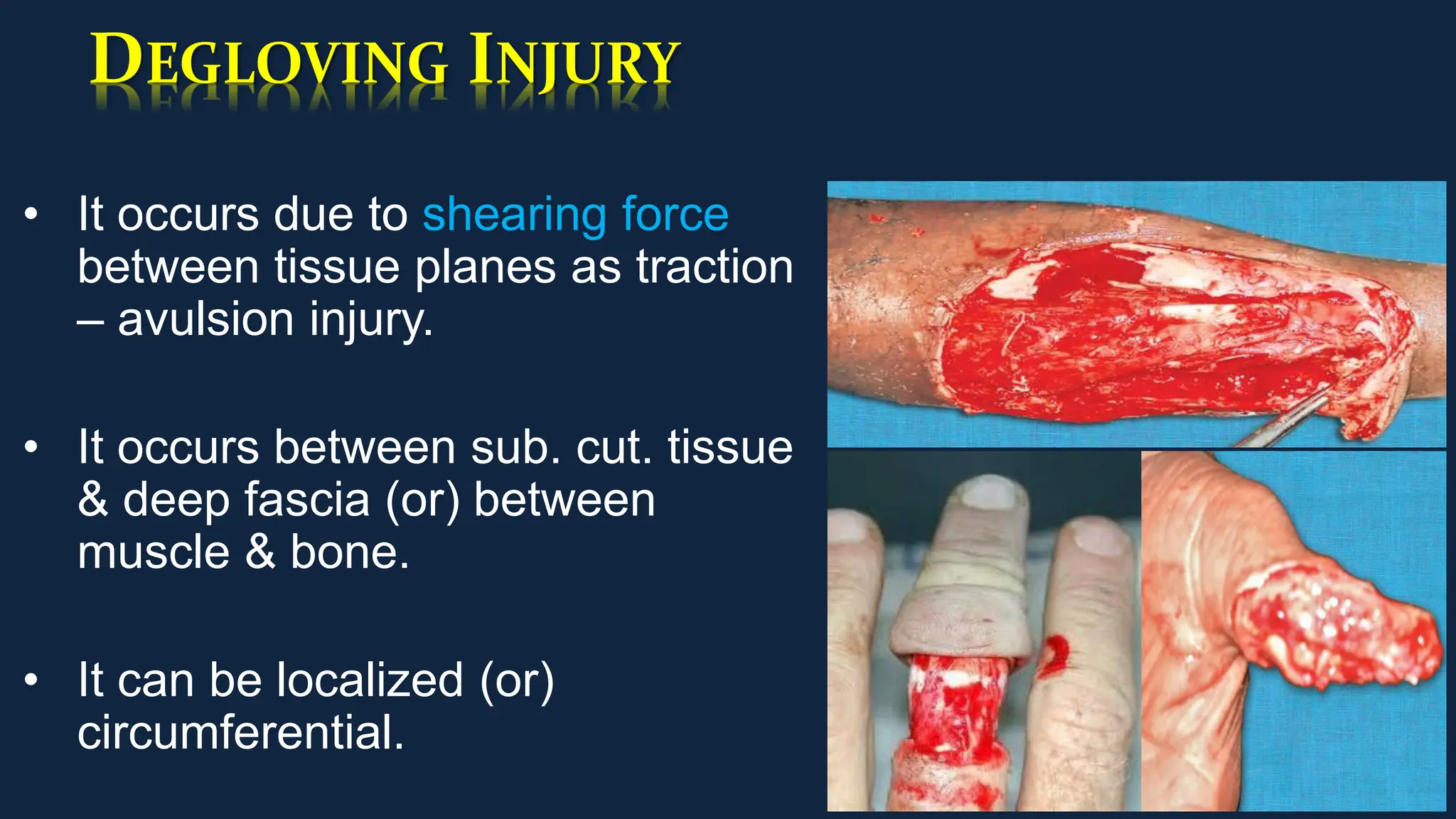
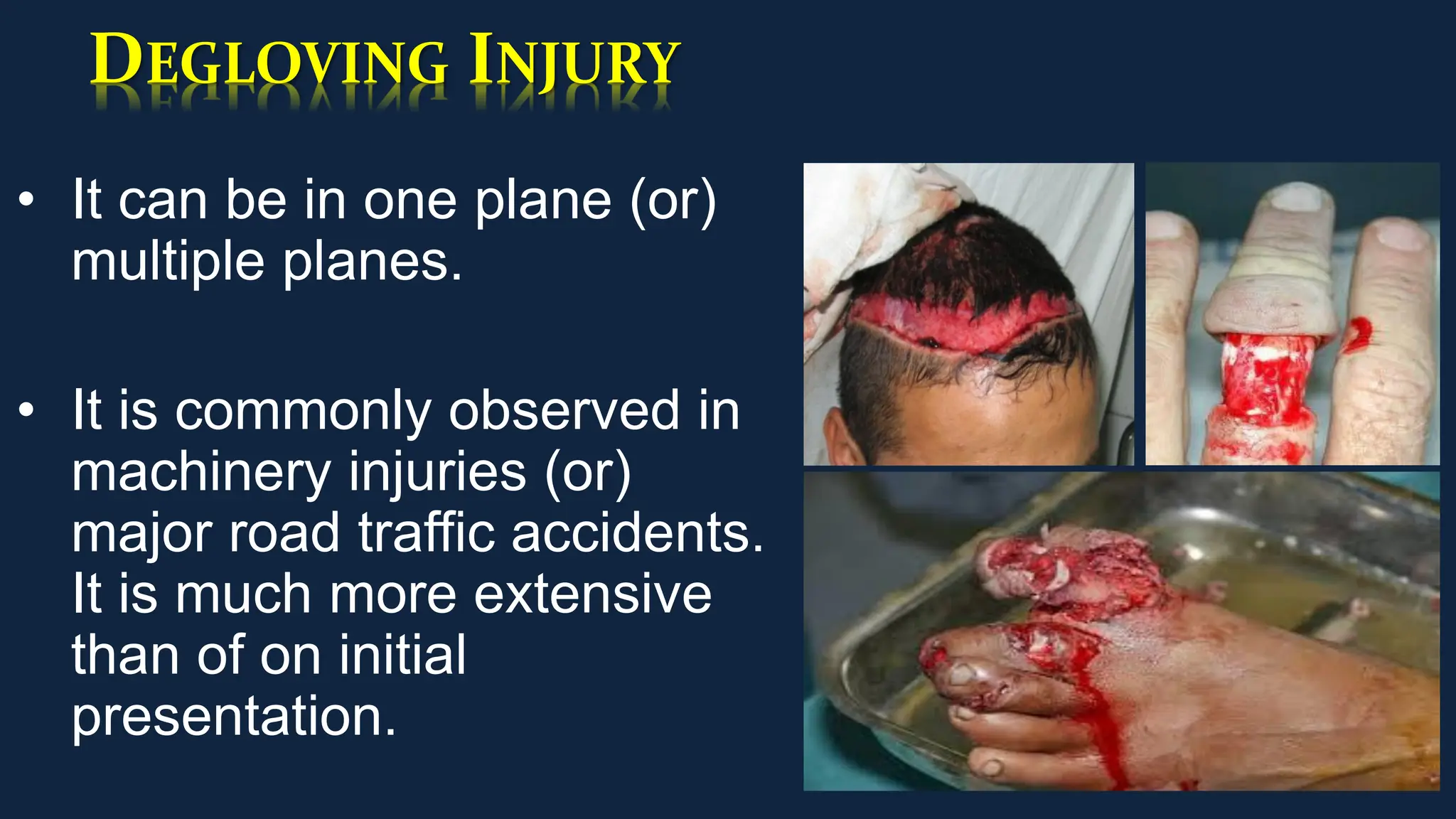
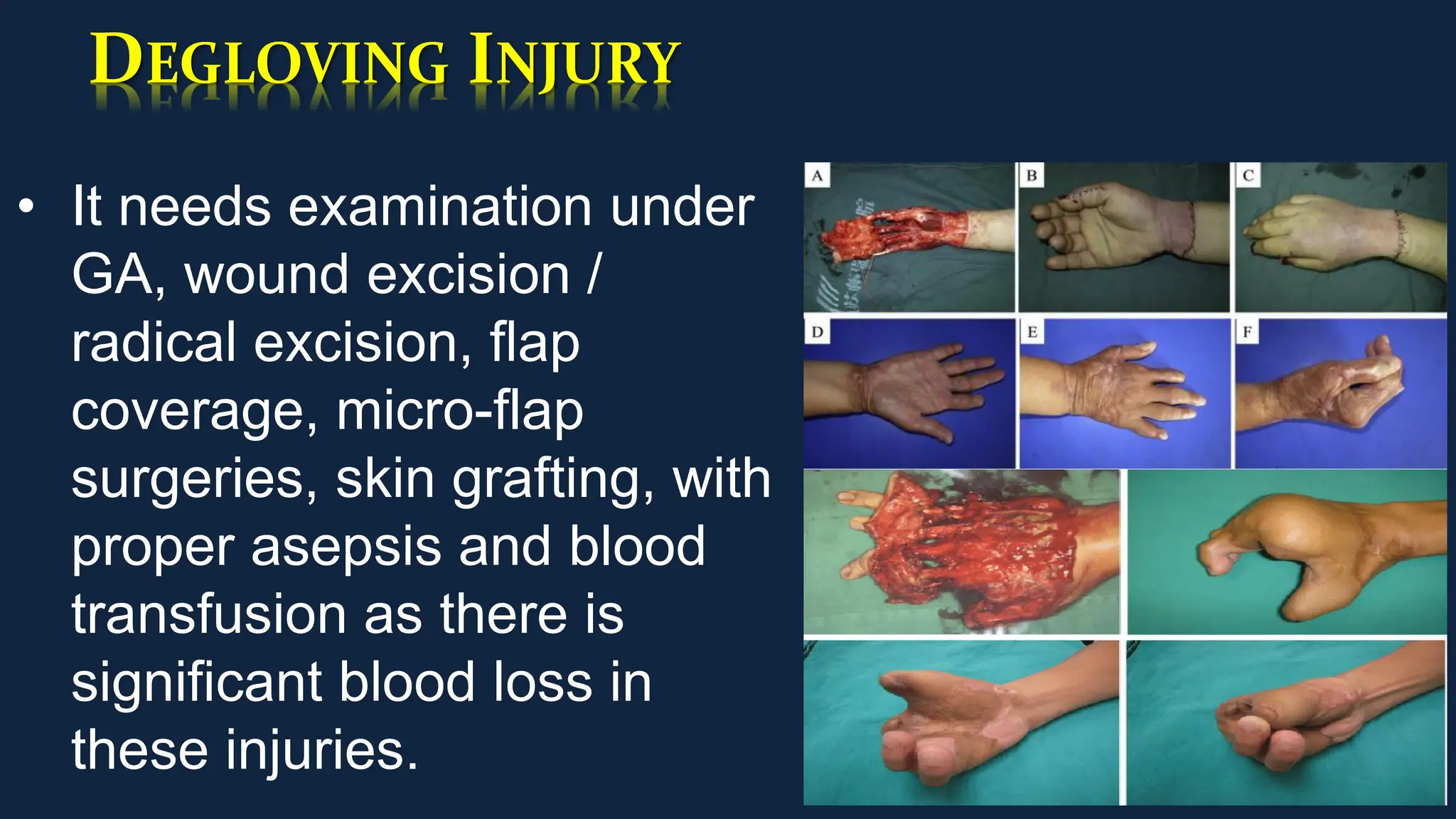
The document outlines the types of wounds and their management, including definitions, classifications, and features of various wound types such as open, closed, and complex wounds. It details wound assessment, preparation, debridement, closure methods, and discusses specific conditions like crush syndrome and de-gloving injuries. Key points include the necessity of proper wound care protocols and categorization of surgical wounds based on infection risk.



















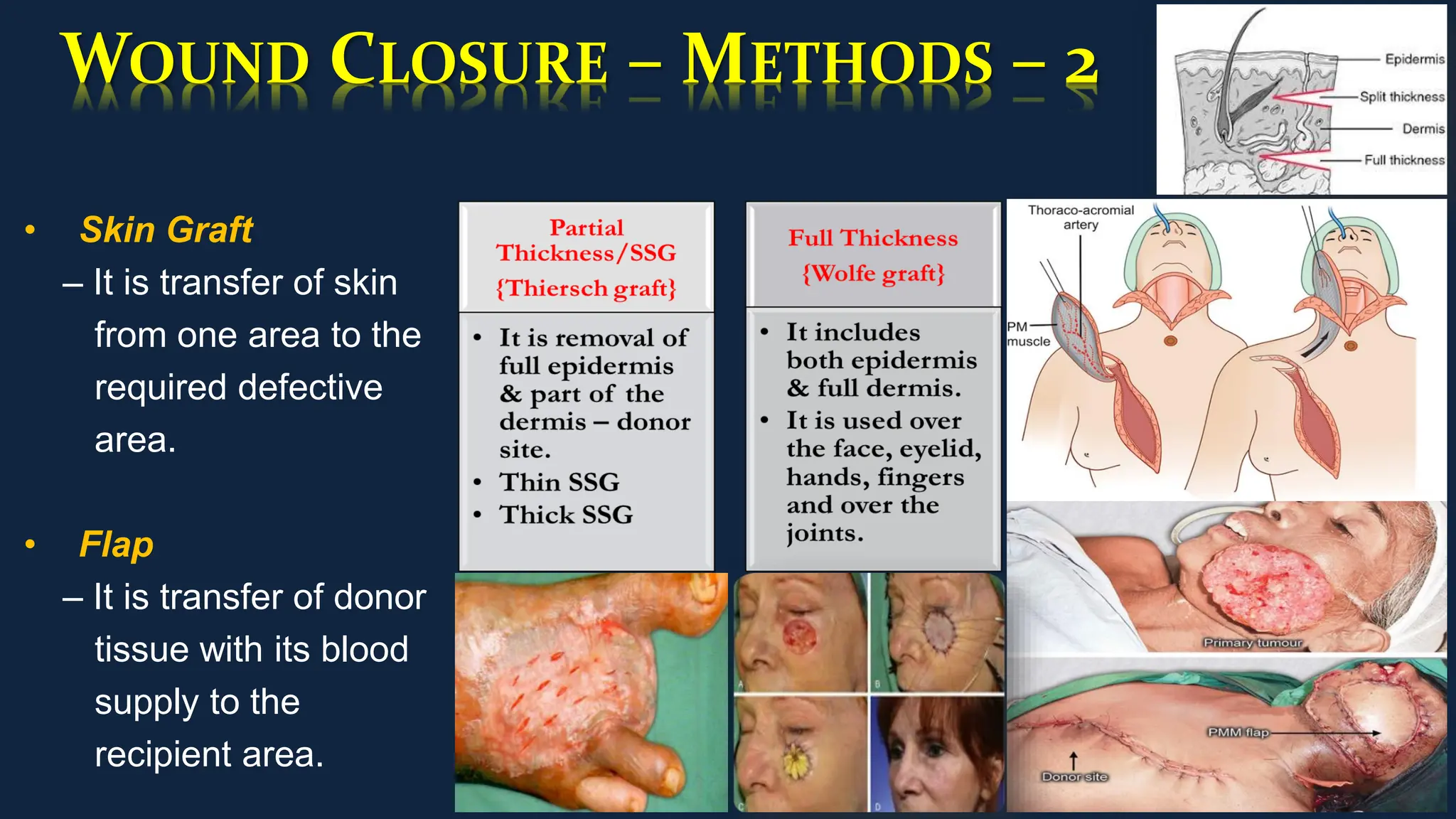
![WOUND CLOSURE – METHODS – 3
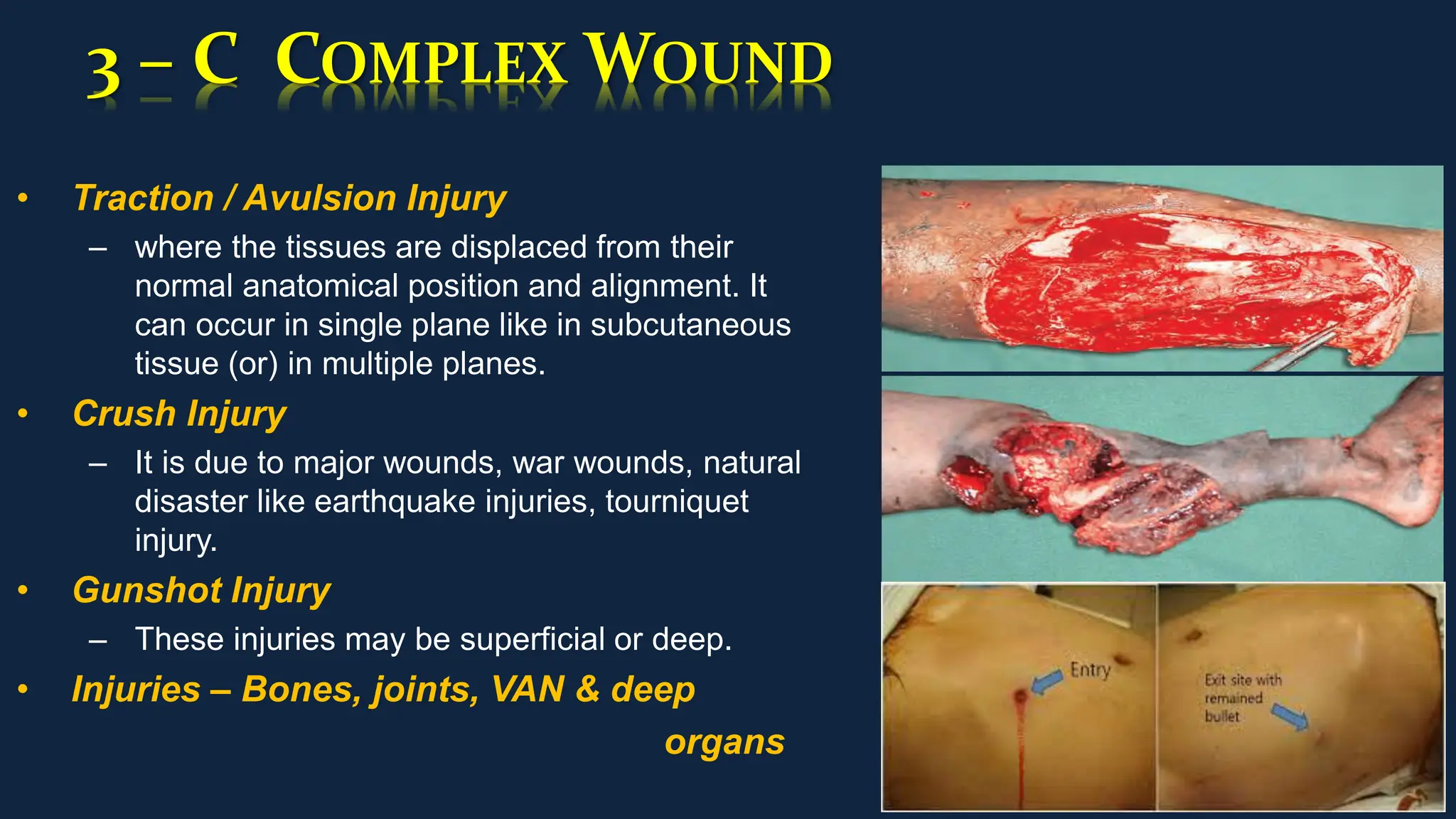
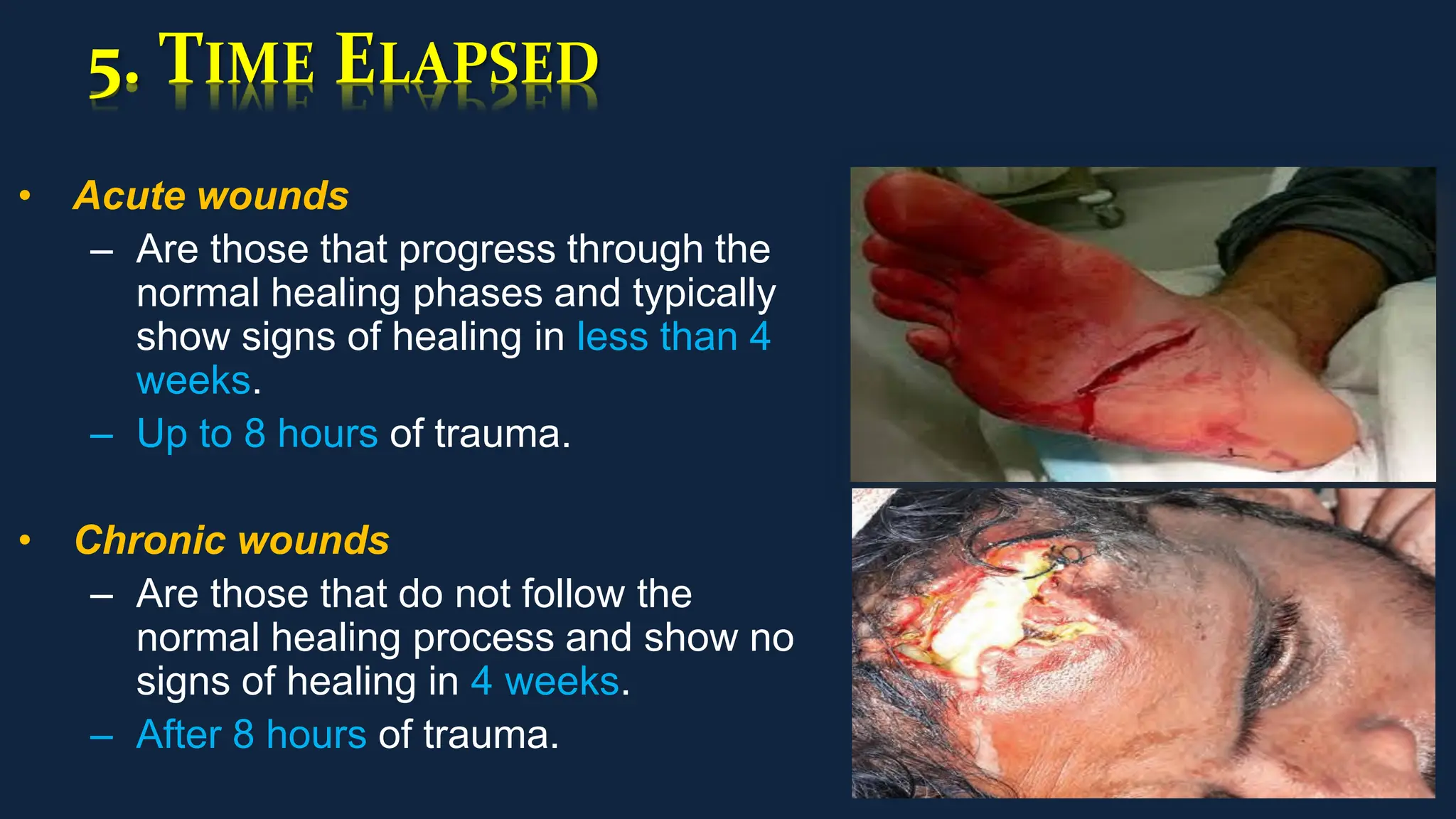
• Negative Pressure Wound Therapy [NPWT]
– It is a useful adjunct to definitive wound
closure.
– Negative pressure helps draw the wound
edges together, remove exudate, reduce
oedema and promote granulation tissue
formation.
• Vacuum Assisted Closure [VAC]
– It is by creation of negative pressure (25-200
mmHg), continuous (or) intermittent over the
wound surface.
– It reduces fluid in the interstitial space, reduces
edema, increases the cell proliferation
& promotes formation of healthy GT.](https://image.slidesharecdn.com/woundtypesmgt-231026134510-160ea869/75/Wound-Types-Management-28-2048.jpg)


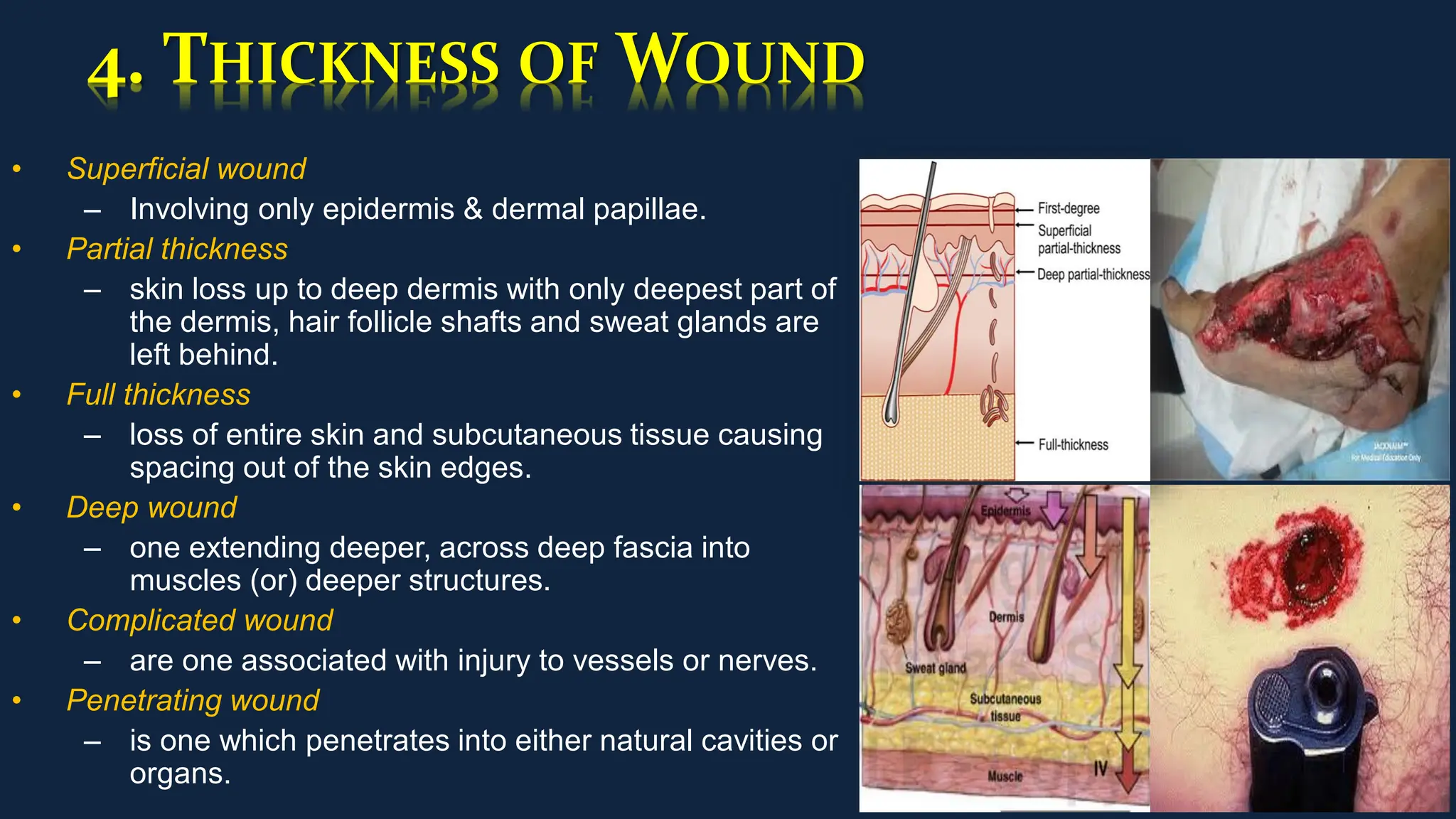
![CRUSH SYNDROME
Causes
• Earthquakes
• Mining & Industrial
accidents
• Battlefield incidents
• Air crash
• Tourniquet
Pathogenesis
• Tension ↑ muscle
compt.
• ↓
• ↑ ischaemic damage
• ↓
• Urine – discoloured
& Scanty
• ↓
• Uraemia [restless,
apathy]
Effects
• Renal failure
• Toxaemia
• Septicaemia
• Disability with tissue
loss
• Gas gangrene](https://image.slidesharecdn.com/woundtypesmgt-231026134510-160ea869/75/Wound-Types-Management-32-2048.jpg)



![ALL THE FOLLOWING ARE PRINCIPLES OF
NEGATIVE PRESSURE WOUND THERAPY [NPWT]
EXCEPT –
• A. Stabilization of wound environment.
• B. Clearance of infection.
• C. Drawing the edges together.
• D. Decreased oedema.](https://image.slidesharecdn.com/woundtypesmgt-231026134510-160ea869/75/Wound-Types-Management-41-2048.jpg)




