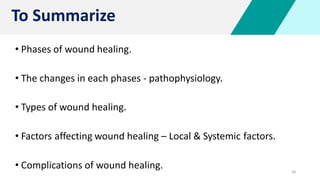
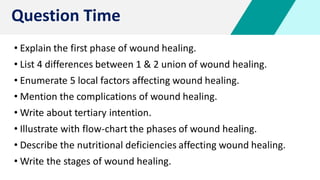
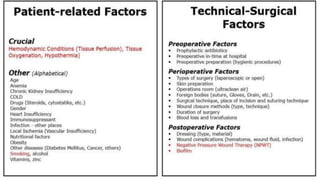
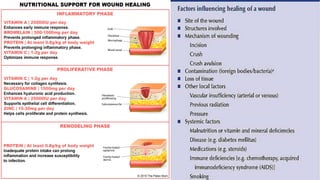
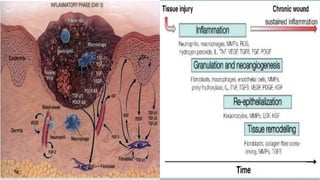
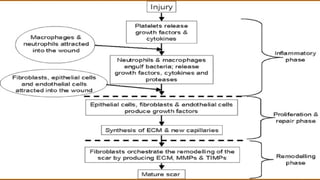
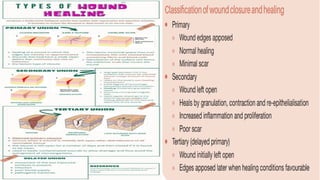
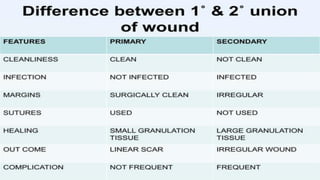
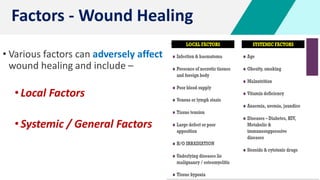
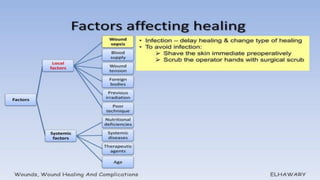
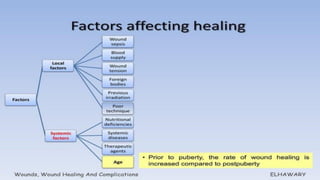
The document discusses wound healing as a complex biological process involving distinct phases: inflammatory, proliferative, and remodeling. Each phase is characterized by specific cellular activities and physiological responses, including hemostasis, inflammation, re-epithelialization, and collagen maturation. Additionally, the document outlines types of wound healing (primary, secondary, and tertiary intention) and factors that can affect healing, as well as complications that may arise.


![4
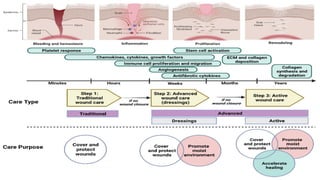
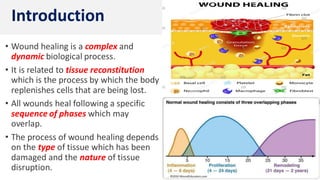
• Classically, wound healing has been
arbitrarily described in 3 overlapping
but distinct stages / phases and include:
• Inflammatory phase
[ Lag / Substrate / Exudative phase ]
• Proliferative phase
[ Collagen / Fibroblastic phase ]
• Remodeling phase
[ Maturation phase ]
Phases of Wound Healing](https://image.slidesharecdn.com/woundhealing-231026135553-d98a4fd4/85/Wound-Healing-4-320.jpg)
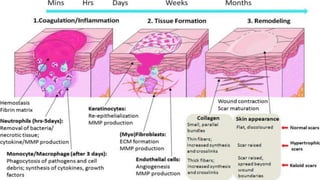
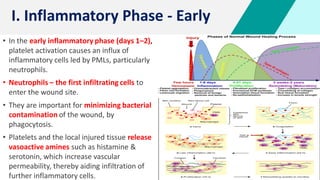
![5
• It begins immediately after wounding & and
lasts 2–3 days.
• Hemostasis, is often described as the
immediate phase occurring before
inflammation.
• Hemostasis is achieved by vasoconstriction
with formation of platelet plug [PT adhere,
activate and aggregate] & activation of
clotting pathway, resulting in formation of
fibrin matrix.
• The fibrin clot helps to stabilize the platelet
plug and form a scaffold for migration of
inflammatory cells [PMLs] into the wound.
I. Phase – H & I](https://image.slidesharecdn.com/woundhealing-231026135553-d98a4fd4/85/Wound-Healing-5-320.jpg)
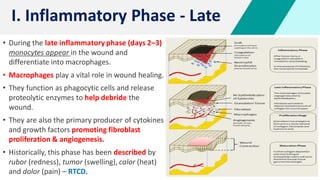


![16
• Wound healing is accomplished in one of
the following 3 ways –
• Healing by primary intention
[wounds with opposed edges]
• Healing by secondary intention
[wounds with separated edges]
• Healing by tertiary intention
[tertiary wound healing]
Types of Wound Healing](https://image.slidesharecdn.com/woundhealing-231026135553-d98a4fd4/85/Wound-Healing-16-320.jpg)
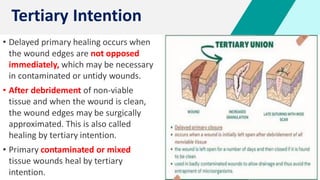














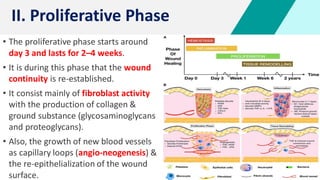
![Complications – W H
• Excessive Scar Formation: Hypertrophic scar,
Keloid.
• Deficient Scar Formation: Result in wound
dehiscence [or] rupture of the wound due to
inadequate formation of granulation tissue.
• Exuberant Granulation (Proud Flesh):
Excessive GT that protrudes above the skin
level.
• Deficient contraction – Skin grafts
Excessive contraction – In Burns
• Others: Pigmentary changes, Incisional
hernia, Dystrophic calcification, Neoplastic
changes.](https://image.slidesharecdn.com/woundhealing-231026135553-d98a4fd4/85/Wound-Healing-55-320.jpg)