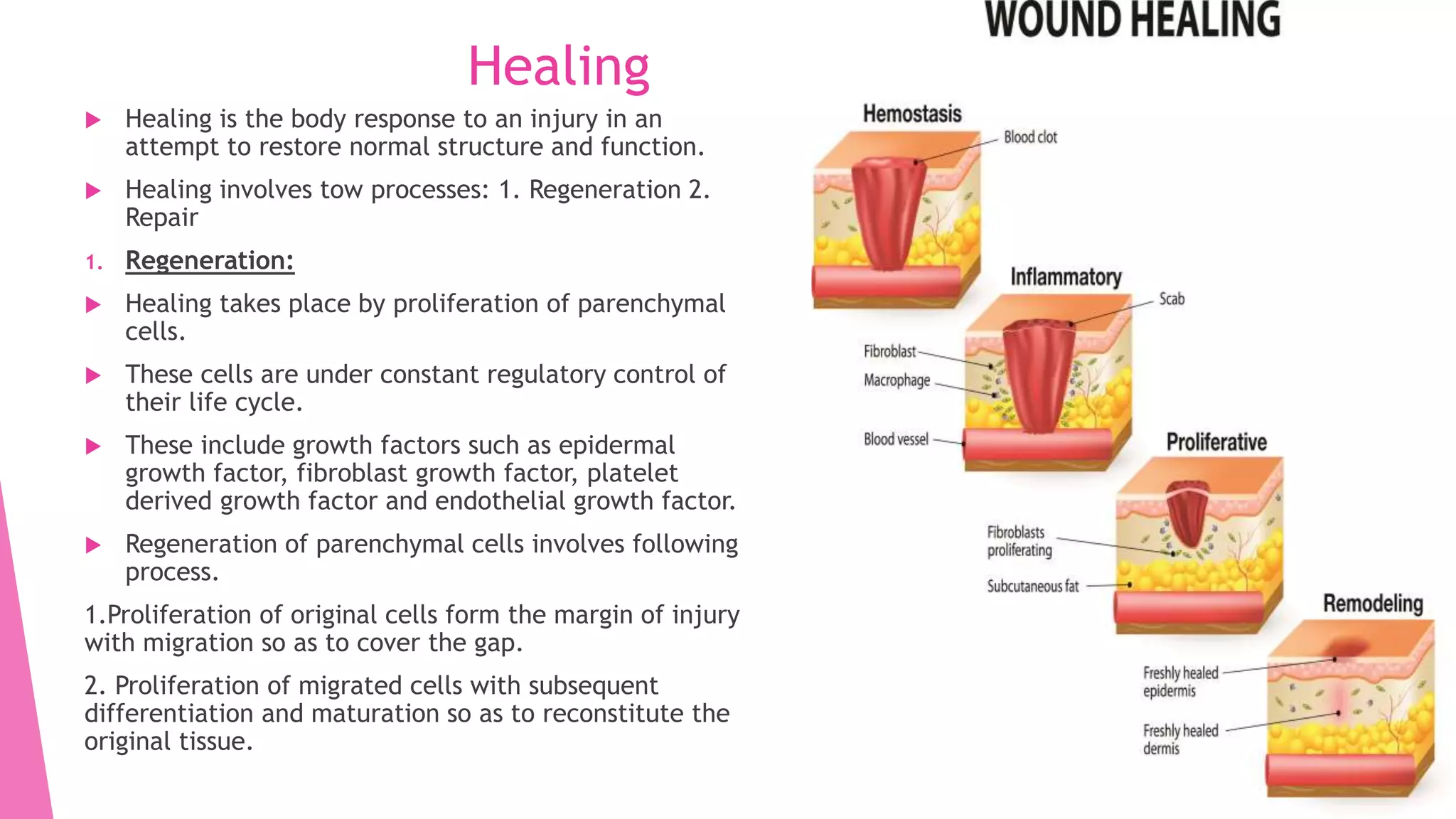
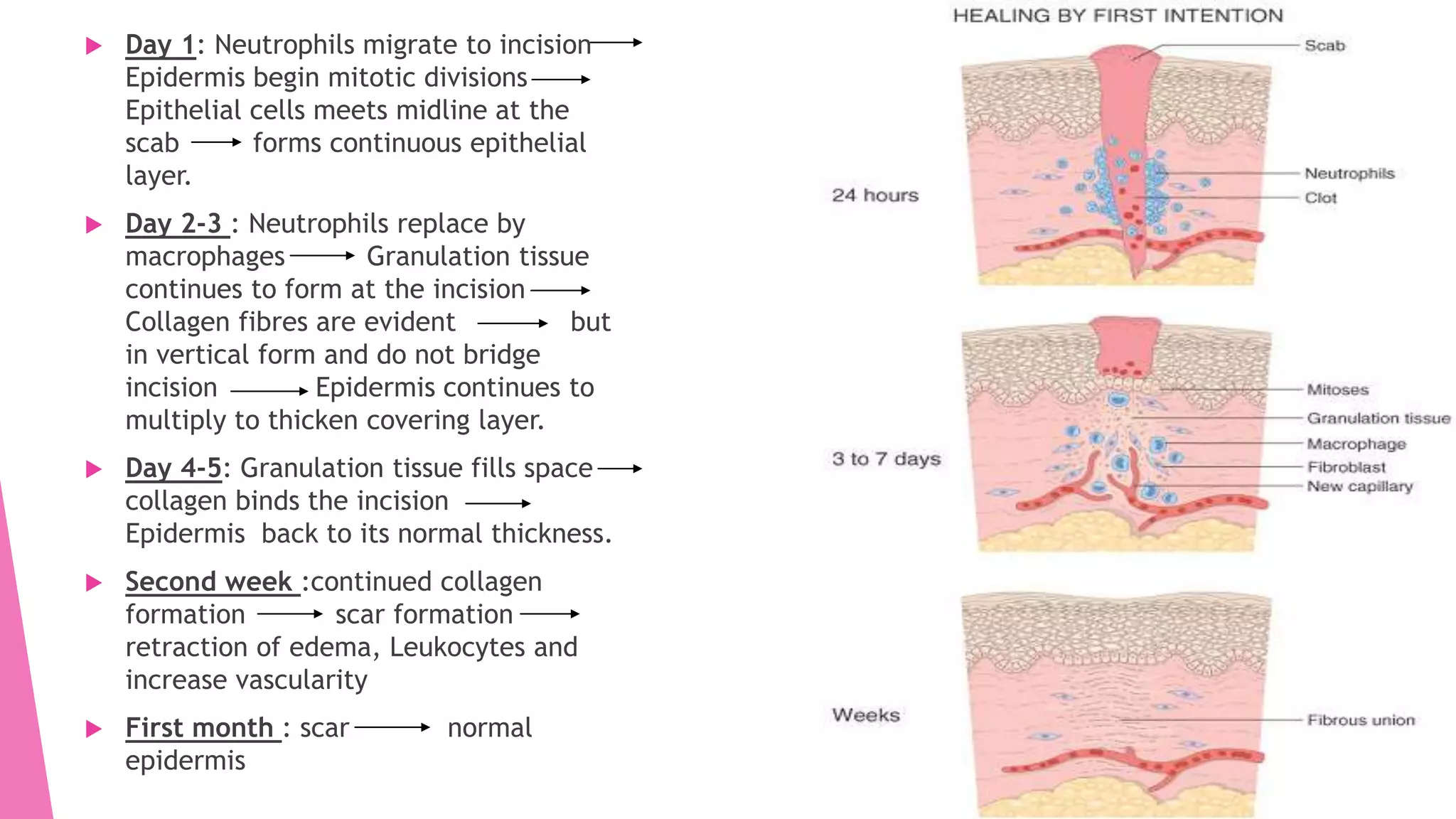
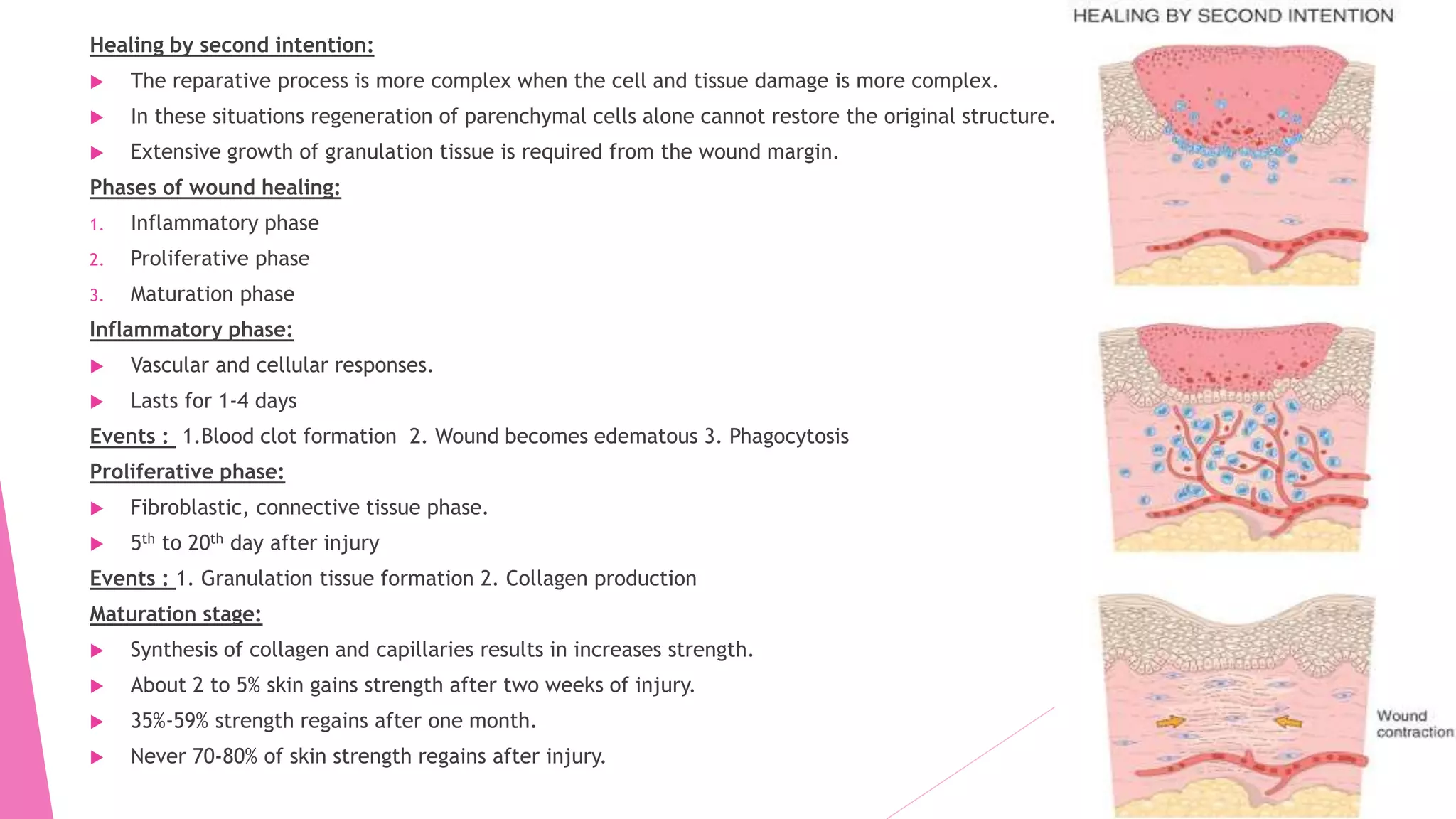
This document summarizes the processes of healing and wound contraction in inflammation. It discusses that healing involves regeneration and repair through two main processes: 1) regeneration occurs through proliferation of parenchymal cells under growth factor regulation, and 2) repair replaces injured tissue with fibrous tissue through granulation tissue formation and wound contraction by myofibroblasts. The healing process generally occurs in three phases: inflammatory, proliferative, and maturation phases, involving blood clot formation, granulation tissue growth, collagen deposition, and scar strengthening over time.