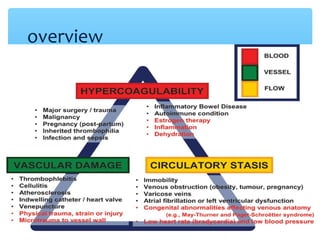
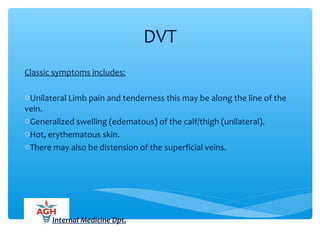
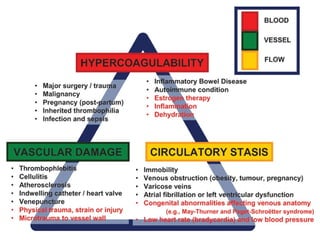
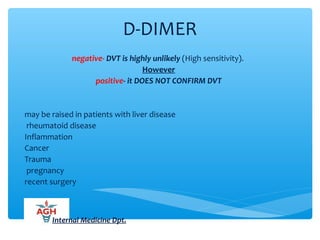
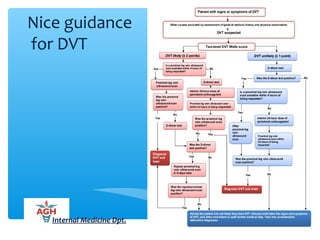
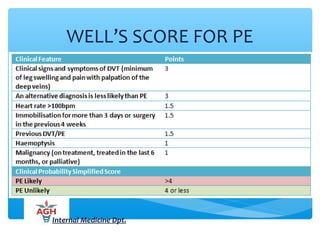
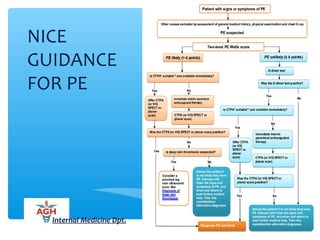
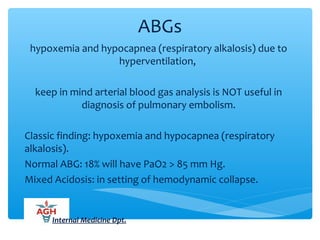
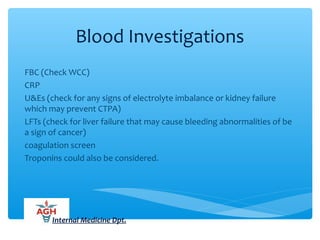
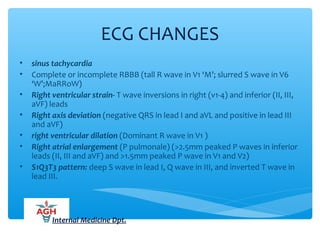
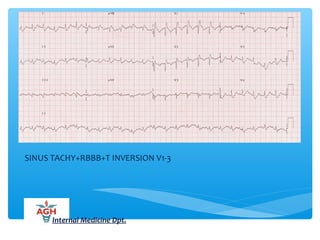
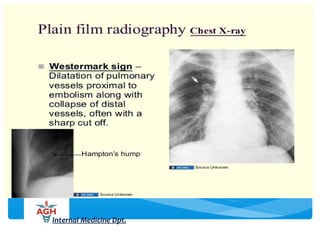
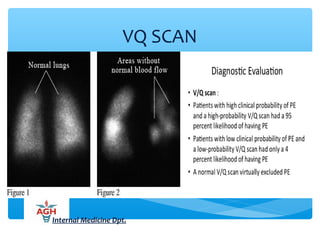
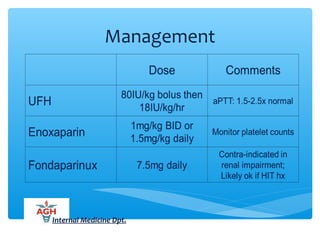
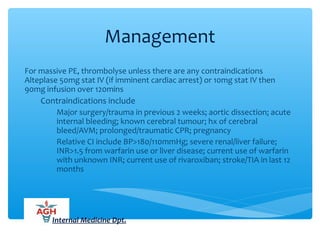
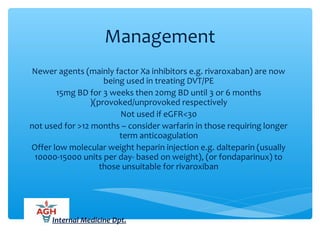
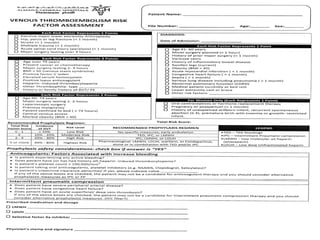
This document provides an overview of venous thromboembolism (VTE) including deep vein thrombosis (DVT) and pulmonary embolism (PE). It discusses risk factors, diagnostic criteria and scoring systems, diagnostic testing including D-dimer and imaging, differential diagnoses, management including anticoagulation options, prevention, and special considerations. The objectives are to review VTE, risks, scoring, diagnosis of DVT and PE, and management approaches. Medical education aims to ensure community health, not just provide career training.