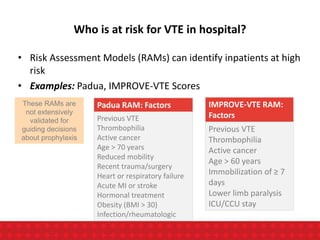
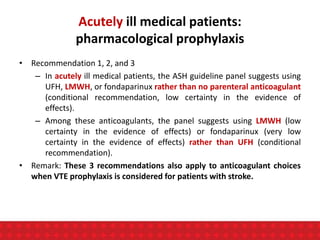
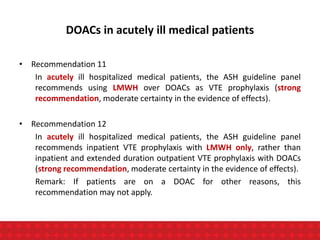
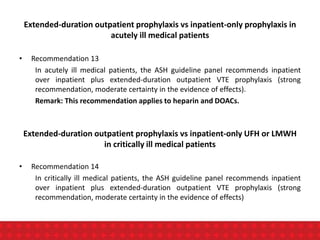
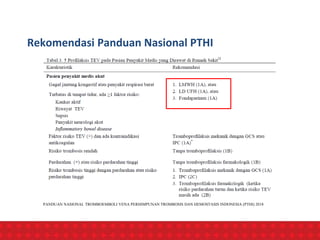
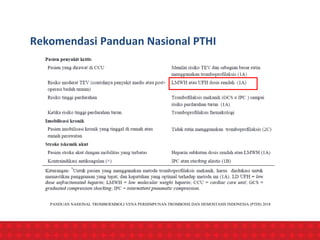
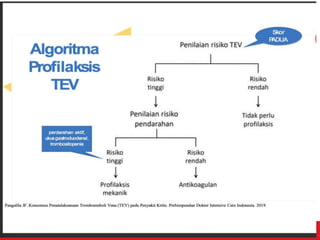
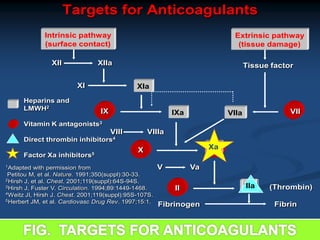
The document discusses venous thromboembolism (VTE) risk assessment and prophylaxis for hospitalized medical patients. It provides recommendations from American Society of Hematology 2018 guidelines and Indonesian Thrombosis and Hemostasis Society 2018 national guidelines. The recommendations suggest using low molecular weight heparin or unfractionated heparin for VTE prophylaxis in acutely ill or critically ill medical patients based on their risk assessment scores. Mechanical prophylaxis alone or combined with pharmacological prophylaxis is conditionally recommended if patients cannot receive anticoagulants. Extended duration outpatient prophylaxis after hospital discharge is not routinely recommended.


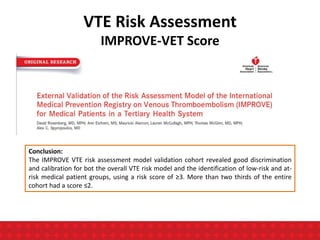
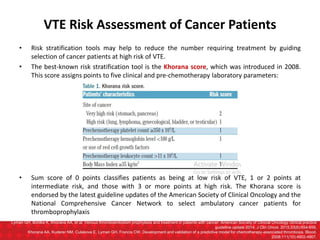
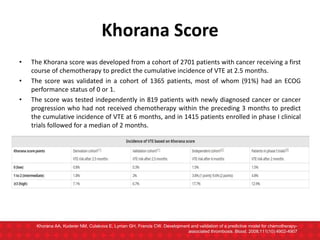
![• The IMPROVE [International Medical Prevention Registry on Venous Thromboembolism]
Predictive score was designed to assesses the risk of VTE in hospitalised medical patients.
• The IMPROVE Predictive score for VTE includes 4 independent risk factors for VTE present at
admission.
• The IMPROVE Associative score includes 7 variables present either at admission or during
hospitalization.
Spyropoulos AC, Anderson FA Jr, Fitzgerald G, Decousus H, Pini M, Chong BH, Zotz RB, Bergmann JF, Tapson V, Froehlich JB, Monreal M, Merli GJ, Pavanello R, Turpie AG,
Nakamura M, Piovella F, Kakkar AK, Spencer FA; IMPROVE Investigators. Predictive and associative models to identify hospitalized medical patients at risk for VTE. Chest.
2011 Sep;140(3):706-14. doi: 10.1378/chest.10-1944. Epub 2011 Mar 24. PMID:21436241
VTE Risk Assessment
IMPROVE-VET Score](https://image.slidesharecdn.com/vteassessmentandprophylaxis-231013093041-1590dc3a/85/VTE-assessment-and-prophylaxis-ppt-12-320.jpg)
















![Ann Intern Med.2007;146:278-88
During anticoagulant prophylaxis, patients had a :
-significant reductions in any PE (RR, 0.43 [CI, 0.26 to 0.71];
-Significant reduction in fatal PE (RR, 0.38 [CI, 0.21 to 0.69];
-non-significant reduction in symptomatic deep venous thrombosis (RR, 0.47
[CI, 0.22 to 1.00]),
-non- significant increase in major bleeding (RR, 1.32 [CI, 0.73 to 2.37]).
-Anticoagulant prophylaxis had no effect on all-cause mortality (RR, 0.97 [CI,
0.79 to 1.19]).
CONCLUSION : Anticoagulant prophylaxis is effective in preventing
symptomatic venous thromboembolism during anticoagulant
prophylaxis in at-risk hospitalized medical patients
Annals Internal Medicine Review. 2007](https://image.slidesharecdn.com/vteassessmentandprophylaxis-231013093041-1590dc3a/85/VTE-assessment-and-prophylaxis-ppt-55-320.jpg)