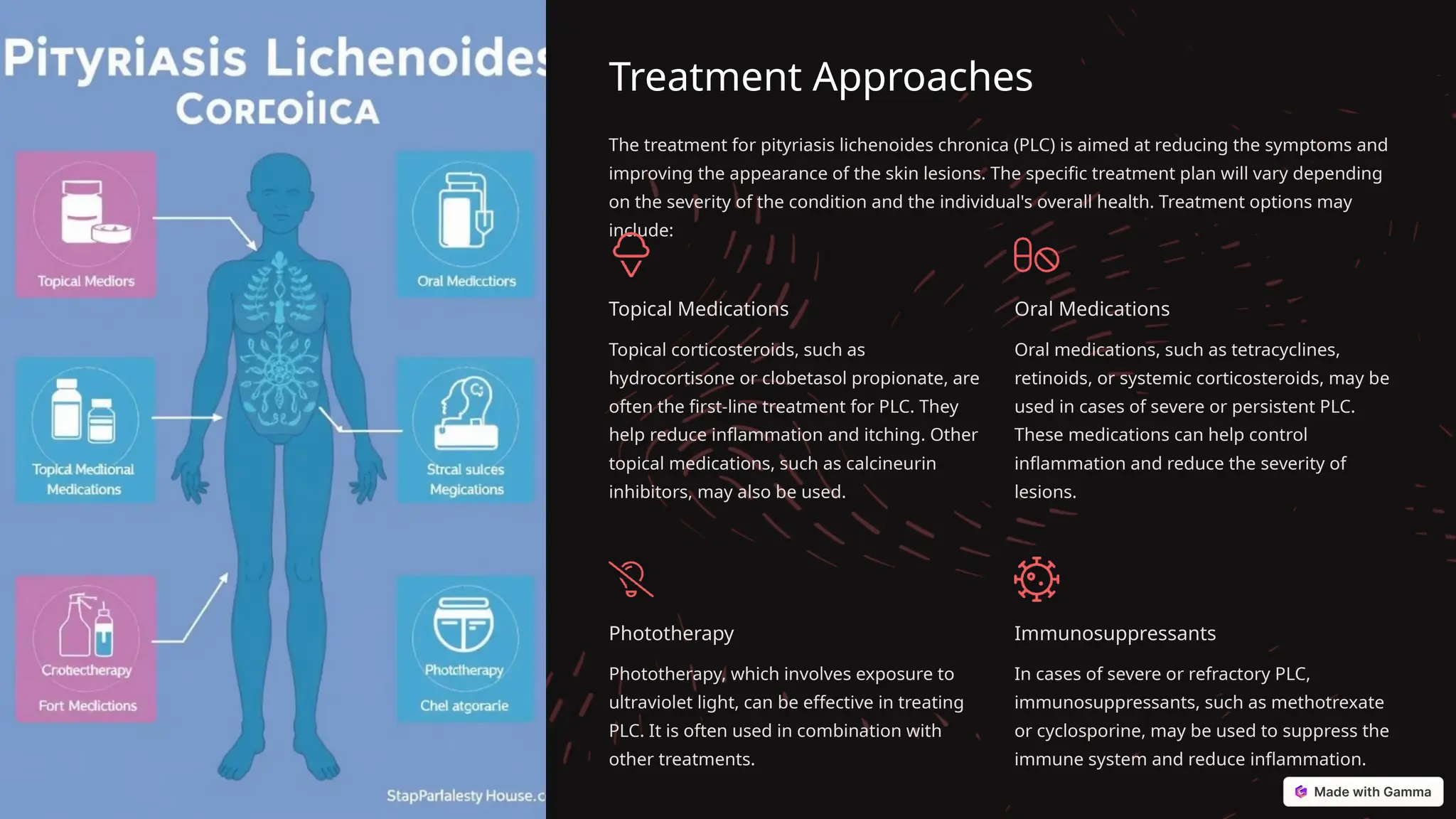
Pityriasis lichenoides chronica (PLC) is a chronic inflammatory skin disorder characterized by small, itchy papules and scales, primarily affecting adults aged 20-40. The condition is believed to be autoimmune in nature and may be triggered by genetic and environmental factors, including viral infections like Epstein-Barr virus. Treatment focuses on managing symptoms and may include topical and oral medications, phototherapy, and immunosuppressants, but relapses are common, requiring ongoing management.